Strategic Approaches to Reduce Endotoxin Contamination in Recombinant Proteins: From Prevention to Removal
This comprehensive article provides researchers, scientists, and drug development professionals with advanced strategies for controlling endotoxin contamination throughout recombinant protein production.
Strategic Approaches to Reduce Endotoxin Contamination in Recombinant Proteins: From Prevention to Removal
Abstract
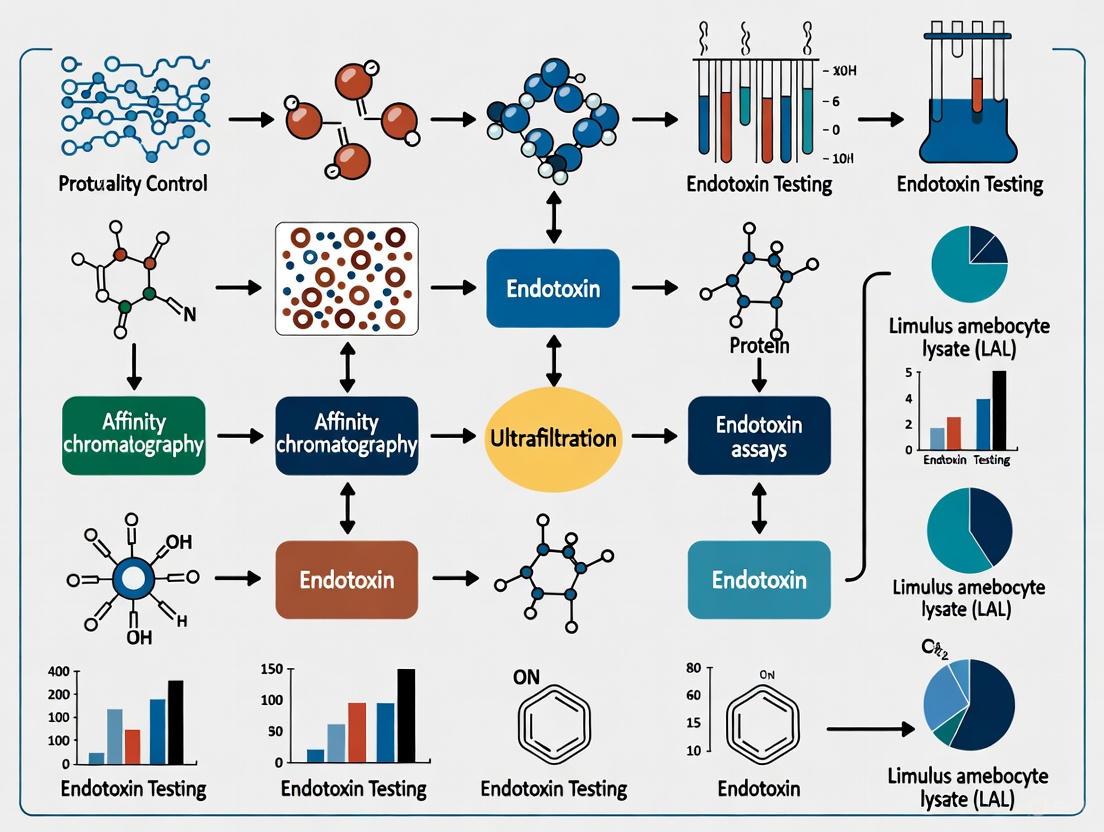
This comprehensive article provides researchers, scientists, and drug development professionals with advanced strategies for controlling endotoxin contamination throughout recombinant protein production. Covering foundational principles to cutting-edge methodologies, we explore preventive controls, comparative analysis of removal techniques including ultrafiltration, chromatography, and novel affinity methods, troubleshooting for common challenges like Low Endotoxin Recovery (LER), and validation frameworks for compliance with global regulatory standards. The content synthesizes current industry practices with emerging research to deliver a actionable guide for ensuring product safety and efficacy in biomedical applications.
Understanding Endotoxin Contamination: Risks, Sources, and Regulatory Foundations
What Are Endotoxins? Defining LPS Structure and Pyrogenic Effects
What are endotoxins and why are they a problem in research?
Endotoxins, more commonly known scientifically as Lipopolysaccharide (LPS), are complex molecules found in the outer membrane of Gram-negative bacteria such as E. coli and Salmonella [1] [2]. They are collectively termed "endotoxins" because they are toxins released when the bacterial cell disintegrates, as opposed to "exotoxins" which are secreted by live bacteria [3] [4].
For researchers, especially those working with recombinant proteins and cell cultures, endotoxin contamination represents a significant problem. Even minute amounts of endotoxin can have substantial impacts on experimental outcomes and product safety [4] [5].
- Immune System Activation: LPS is a potent activator of the mammalian immune system. It binds to the CD14/TLR4/MD2 receptor complex on immune cells like monocytes and macrophages, triggering a robust pro-inflammatory response [1] [4]. This can lead to the secretion of cytokines, fever, and in severe cases, septic shock [1] [2].
- Experimental Artifacts: In cell-based assays, endotoxin contamination can cause unintended immune activation, distorting research results and leading to false conclusions [5]. For example, in studies involving microglia or other immune cells, endotoxin-contaminated tau protein can provoke an inflammatory response that is misinterpreted as a disease-specific effect [6].
- Regulatory and Safety Concerns: For biological pharmaceuticals and therapeutics intended for parenteral (injected) use, strict limits on endotoxin levels are enforced. The United States Pharmacopeia (USP) sets a limit of 5 Endotoxin Units (EU) per kg of body weight for products administered intravenously over an hour [4] [7]. Contamination can lead to adverse patient reactions, including fever and shock, and result in product recalls [3].
What is the structure of LPS?
The potent biological effects of endotoxins are directly linked to their unique molecular architecture. LPS are large, amphipathic molecules, meaning they have both hydrophilic (water-attracting) and hydrophobic (water-repelling) regions [1]. Their structure can be divided into three distinct domains, each with a specific function.
Domains of LPS Structure
| Domain | Chemical Composition | Function and Properties |
|---|---|---|
| Lipid A [1] [2] | A phosphorylated glucosamine disaccharide decorated with multiple fatty acid chains (e.g., often hexa-acylated in E. coli) [2]. | - Hydrophobic anchor that embeds LPS in the bacterial outer membrane [1].- The endotoxic center responsible for most of the biological toxicity; a potent pyrogen [1] [2]. |
| Core Oligosaccharide [1] [2] | An inner and outer core containing sugars like heptose and 3-Deoxy-D-manno-oct-2-ulosonic acid (KDO) [1]. | - Connects Lipid A to the O-antigen [1].- Contributes to membrane stability [2].- Less variable than the O-antigen [1]. |
| O-Antigen (O Polysaccharide) [1] [2] | A repeating, variable chain of oligosaccharides (2-8 sugars per unit) projecting out from the core [2]. | - The most variable part of LPS, determining serological specificity (e.g., over 160 variants in E. coli) [1] [2].- Helps bacteria evade host immune defenses [2]. |
The following diagram illustrates the spatial relationship of these three domains within the bacterial outer membrane.
Some bacteria, such as Neisseria and Haemophilus, produce a form of LPS that lacks the long O-antigen chain. This is known as Lipooligosaccharide (LOS) and is often associated with increased virulence and ability to mimic host molecules [1].
How do I detect and measure endotoxin contamination?
Detecting and quantifying endotoxin levels is a critical quality control step. The following table compares the primary methods available.
Endotoxin Detection Methods
| Method | Principle | Sensitivity & Key Features | Regulatory Status |
|---|---|---|---|
| Limulus Amebocyte Lysate (LAL) [3] [7] | Lysate from horseshoe crab blood cells clots or changes in the presence of endotoxin. | - Gel-clot: Qualitative (clot/not); sensitivity ~0.03 EU/mL [4].- Turbidimetric: Measures turbidity change; quantitative [4].- Chromogenic: Measures color change from substrate hydrolysis; quantitative [4]. | USP standard for pharmaceutical and device testing [7]. |
| Recombinant Assays [7] | Uses recombinant enzymes instead of natural crab lysate to detect endotoxin. | - Avoids use of animal-derived components.- May have longer incubation times or reduced dynamic range. | Considered an alternative method; may require additional validation [7]. |
| Fluorescent LAL Assays (e.g., Qubit) [7] | A subset of LAL assays that uses fluorescence for detection. | - High sensitivity (0.01 - 10.0 EU/mL).- Easy-to-use workflow with automated calculation on compatible fluorometers. | Can be validated to comply with Pharmacopeia standards [7]. |
| Rabbit Pyrogen Test [3] [4] | Measures fever response in rabbits after injection of a test sample. | - In vivo test.- Less sensitive than LAL tests.- Requires more time, expense, and specialized training. | Official method in pharmacopeias, but largely supplanted by in vitro LAL tests [3]. |
For any LAL-based method, it is crucial to perform a validation to check for assay interference. This involves a "spike recovery" test, where a known amount of endotoxin is added to the sample. The recovery of this spike should be between 50-200% (with many labs aiming for 75-150%) to ensure the sample matrix itself is not inhibiting or enhancing the assay reaction [7] [8].
What methods can remove endotoxins from protein samples?
Removing bound endotoxin from recombinant proteins, especially those expressed in E. coli, is a common challenge. Endotoxin-protein interactions are often hydrophobic and ionic, making them difficult to disrupt without affecting the protein of interest [4]. The table below summarizes common removal techniques.
Endotoxin Removal Methods
| Method | Mechanism of Action | Best Suited For |
|---|---|---|
| Triton X-114 Phase Separation [6] [4] | Exploits the amphiphilic nature of LPS. Upon heating, the detergent solution separates into detergent-rich (containing LPS) and aqueous phases (containing protein). | Proteins stable in non-ionic detergents; a key step in protocols for sensitive cell culture work [6]. |
| Ion-Exchange Chromatography [4] | Separates based on charge. The negative charge of the LPS core polysaccharide can be exploited to bind it to a resin while the protein flows through, or vice versa. | Proteins with a charge significantly different from the negative charge of LPS. |
| Affinity Adsorbents [4] | Uses resins with immobilized molecules (e.g., polymyxin B) that have a high binding affinity for the Lipid A portion of LPS. | A highly specific method for polishing steps to remove trace endotoxin. |
| Gel Filtration Chromatography [4] | Separates molecules based on size. If the protein and LPS aggregates are of sufficiently different sizes, they can be separated. | Proteins with a molecular weight significantly different from LPS aggregates. |
Detailed Protocol: Triton X-114 Phase Separation
This protocol is highly effective for removing bound endotoxin from recombinant proteins, as demonstrated for tau protein used in microglial cell culture [6].
Workflow Overview:
Step-by-Step Instructions:
- Treat with Triton X-114: In a 1.5 mL microcentrifuge tube, add 25% Triton X-114 stock solution to your protein sample to achieve a final concentration of 2% detergent. It is recommended to use a protein concentration greater than 0.2 mg/mL to minimize losses [6].
- Incubate Cold: Incubate the mixture at 4°C for one hour with constant rotation. This allows the detergent to interact with the endotoxin [6].
- Induce Phase Separation: Transfer the tube to a 37°C water bath for 10 minutes. The solution will become turbid as it separates into two phases [6].
- Centrifuge: Centrifuge the tube at 20,000 x g for 20 minutes at 37°C. This will complete the phase separation, resulting in a small, dense detergent-rich pellet (containing the endotoxin) and a top aqueous phase (containing your protein) [6].
- Collect Aqueous Phase: Carefully collect the top aqueous layer without disturbing the bottom detergent phase. If the interface is disturbed, repeat the centrifugation [6].
- Repeat Cycles: To ensure maximum endotoxin removal, repeat the treatment cycle (steps 1-5) two more times for a total of three phase separations [6].
- Remove Residual Detergent: After the third cycle, pass the collected aqueous phase through a detergent-removal spin column (following manufacturer's instructions) to eliminate any residual Triton X-114 from the final protein preparation [6].
Verification of Removal: After purification, it is essential to quantify the remaining endotoxin levels using an LAL assay [6]. Furthermore, a functional validation using a cell-based assay, such as monitoring the inflammatory response in endotoxin-sensitive cells (e.g., HEK-Blue hTLR4 reporter cells or iPSC-derived microglia), is highly recommended to confirm the biological relevance of the removal [6].
The Scientist's Toolkit: Essential Reagents for Endotoxin Control
| Reagent / Material | Function in Endotoxin Control |
|---|---|
| Triton X-114 [6] | A non-ionic detergent used in phase separation protocols to solubilize and separate endotoxin from proteins. |
| Limulus Amebocyte Lysate (LAL) [3] [7] | The key reagent derived from horseshoe crab blood used in the majority of in vitro endotoxin detection tests. |
| Endotoxin Standards [7] | Known concentrations of endotoxin used to calibrate LAL assays and generate standard curves for accurate quantification. |
| Detergent Removal Spin Columns [6] | Used to clean up residual detergents (like Triton X-114) from protein samples after endotoxin removal procedures. |
| Endotoxin-Free Water & Buffers [3] [5] | Critical base reagents used in all steps of protein preparation and testing to prevent the introduction of new contamination. |
| Endotoxin-Free Plastics [7] [5] | Specially manufactured labware (tubes, tips, plates) that do not leach endotoxins, which can easily adsorb to plastics. |
Frequently Asked Questions (FAQs)
Q1: Why are my mammalian cell cultures activating unexpectedly, showing high cytokine secretion? This is a classic sign of endotoxin contamination. LPS is a potent activator of immune cells like macrophages, triggering cytokine release. You should screen your culture media, supplements (e.g., FBS), and any recombinant proteins or other additives added to the culture using an LAL test [4] [5].
Q2: My recombinant protein is expressed in E. coli and is very "sticky." How can I prevent endotoxin contamination from the start? Prevention is always better than cure. Use endotoxin-free plasmids, water, and buffers from the beginning of your protein expression and purification workflow. Store purified proteins in low endotoxin affinity plastic containers and maintain strict aseptic technique to avoid bacterial growth in your stocks [5].
Q3: I've purified my protein, but the LAL test shows high endotoxin. Can I just filter it out? No. Standard sterilizing filters (0.22 µm) remove bacteria but not the much smaller endotoxin molecules. Furthermore, endotoxins often form stable aggregates or bind tightly to your protein of interest, making them impossible to remove by simple filtration. You will need to employ a dedicated removal technique like Triton X-114 phase separation or affinity chromatography [3] [4].
Q4: Is "sterile" technique enough to control for endotoxins? No. This is a critical distinction. "Sterile" means the absence of viable microorganisms. "Endotoxin-free" means the absence of the heat-stable endotoxin molecules themselves. LPS can withstand standard autoclaving and remain fully active. Therefore, a solution can be sterile but still pyrogenic (fever-causing) due to high endotoxin levels [3] [7].
Frequently Asked Questions (FAQs)
Q1: What are endotoxins, and why are they a significant concern in pharmaceutical and research applications? Endotoxins, also known as lipopolysaccharides (LPS), are toxic components found in the cell wall of gram-negative bacteria like E. coli [9]. They are a major contaminant in recombinant proteins produced using bacterial expression systems. The primary concern is their potent biological activity; even trace amounts can trigger pyrogenic (fever) responses in patients [10]. Upon entering the bloodstream, endotoxins can cause severe immune reactions, including inflammation and septic shock, a life-threatening condition characterized by persistent hypotension and organ dysfunction despite adequate fluid resuscitation [9] [11].
Q2: My recombinant protein is intended for cell culture experiments. Why is endotoxin removal critical? Endotoxin contamination in protein preparations can cause false outcomes in research by inducing unintended cellular responses [9]. For instance, in studies involving microglia or other immune cells, endotoxins can activate inflammatory pathways, leading to the secretion of cytokines and confounding the results [6]. Therefore, effective endotoxin removal is a prerequisite for obtaining reliable and biologically relevant data from cell-based assays.
Q3: What are the most effective methods for removing endotoxins from protein solutions? Several methods are available, each with different mechanisms, efficiencies, and limitations. The choice of method depends on the nature of your protein and the required purity level.
- Affinity Chromatography: This method uses ligands (e.g., polymyxin B) that specifically bind to the lipid A portion of endotoxins. It offers high efficiency and specificity, effectively removing endotoxins while preserving the target protein [9] [12].
- Ion Exchange Chromatography: This technique exploits the strong negative charge of endotoxins. Under standard conditions (pH > 2), endotoxins bind to positively charged resins, while many target proteins flow through. It provides high efficiency and is easily scalable [9].
- Phase Separation (e.g., with Triton X-114): This is a non-chromatographic method that uses a detergent. The solution is cycled between cold and warm temperatures, causing endotoxins to partition into a detergent-rich phase, which is separated from the aqueous protein-containing phase by centrifugation. It offers moderate efficiency and is a relatively simple protocol [6] [9].
- Ultrafiltration: This physical separation method uses membranes with a specific molecular weight cutoff (e.g., 100 kDa) to retain large endotoxin aggregates while allowing smaller proteins to pass. Its efficiency is moderate and can be variable [9].
Table 1: Comparison of Common Endotoxin Removal Methods
| Method | Mechanism | Efficiency | Specificity | Key Limitations |
|---|---|---|---|---|
| Affinity Chromatography | Specific ligand binding (e.g., Polymyxin B) | High [9] | High [9] | High cost; may require elevated ionic strength for elution [9] |
| Ion Exchange Chromatography | Electrostatic charge interactions | High [9] | Medium [9] | Sensitive to pH and salt conditions [9] |
| Phase Separation | Temperature-driven partitioning using detergents | Moderate (45-99%) [9] | Low [9] | Potential for trace detergent residues; may require multiple cycles [6] [9] |
| Ultrafiltration | Size-based physical separation | Moderate (28.9-99.8%) [9] | Low [9] | Ineffective at removing smaller endotoxin fragments [9] |
Q4: How do I quantify endotoxin levels to validate the success of my removal process? The Limulus Amebocyte Lysate (LAL) test is the standard and FDA-accepted method for endotoxin quantification, replacing the older rabbit pyrogen test [13]. This test is available in several formats (gel clot, turbidimetric, chromogenic). Alternatively, ELISA kits are available that can detect endotoxins with high sensitivity, down to 0.5 pg/ml [14]. For biologically relevant validation, you can use cell-based assays, such as HEK-Blue hTLR4 reporter cells, which secrete an easily detectable enzyme (SEAP) upon activation by endotoxins in a dose-dependent manner [6].
Troubleshooting Guides
Problem: Inconsistent Endotoxin Removal with Triton X-114 Phase Separation
Possible Causes and Solutions:
Cause 1: Inefficient Phase Separation
- Solution: Ensure precise temperature control during the protocol. The initial incubation with Triton X-114 must be at 4°C for 1 hour with rotation to form a homogenous solution. The phase separation step must then be performed at 37°C for 10 minutes in a water bath, followed by centrifugation at 37°C [6]. The solution should appear turbid after the 37°C incubation.
Cause 2: Cross-Contamination of Phases
- Solution: After centrifugation, take extreme care when collecting the top, protein-containing aqueous phase. Do not disturb the lower, detergent-rich phase where the endotoxins reside. If the interface is disturbed, repeat the centrifugation step [6].
Cause 3: Insufficient Cleaning Cycles
Problem: Low Protein Recovery After Affinity Chromatography
Possible Causes and Solutions:
Cause 1: Non-Specific Binding of Target Protein
- Solution: While affinity resins like Polymyxin B are designed for specificity, some proteins may still bind non-specifically. Optimize the binding buffer's pH and ionic strength to minimize unwanted interactions while maintaining endotoxin binding. Using a different removal method, such as ion exchange chromatography, might be more suitable for your specific protein [9].
Cause 2: Protein Loss During Detergent Removal
- Solution: If using a detergent-based method followed by a detergent removal column, note that protein loss is greater if the initial protein concentration is too low. It is recommended to use a protein concentration greater than 0.2 mg/mL before proceeding with detergent removal spin columns [6].
Detailed Experimental Protocol: Endotoxin Removal via Triton X-114 Phase Separation
This protocol is adapted from a published method for purifying E. coli-derived tau protein and is broadly applicable to other recombinant proteins [6].
Summary: The protocol uses the non-ionic detergent Triton X-114, which forms a homogeneous solution with the protein at low temperatures but separates into detergent-rich and aqueous phases upon warming. Endotoxins, being highly hydrophobic, partition into the detergent phase, while the target protein remains in the aqueous phase.
Graphical Workflow:
Key Resources Required:
- REAGENTS: Triton X-114, 1x DPBS, Detergent removal spin columns, Endotoxin-free water [6].
- EQUIPMENT: Microcentrifuge tubes, water baths (4°C and 37°C), centrifuge, rotation mixer.
Step-by-Step Method Details [6]:
- Add Triton X-114: In a 1.5 mL microcentrifuge tube, add 25% Triton X-114 stock to your protein solution to achieve a final concentration of 2% Triton X-114.
- Cold Incubation: Incubate the mixture at 4°C for 1 hour with constant rotation to form a homogenous solution.
- Warm Incubation & Phase Separation: Transfer the tube to a 37°C water bath and incubate for 10 minutes. The solution will become turbid.
- Centrifugation: Centrifuge the tube at 20,000 x g for 20 minutes at 37°C. This will complete the phase separation, resulting in a top aqueous layer (containing your protein) and a bottom detergent layer (containing endotoxins).
- Collect Aqueous Phase: Carefully collect the top aqueous layer without disturbing the bottom detergent layer. If the layers are mixed, repeat the centrifugation.
- Repeat Process: Subject the collected aqueous phase to the same process (steps 1-5) two more times, for a total of three phase separations.
- Remove Residual Detergent: a. Prepare a detergent removal spin column by centrifuging to remove storage solution and equilibrating it with three washes of the buffer matching your protein sample. b. Apply the Triton X-114-treated protein from Step 6 to the prepared spin column and incubate at room temperature for 2 minutes. c. Centrifuge the column to collect the purified, detergent-free protein.
- Endotoxin Quantification: Measure the endotoxin level in the final protein preparation using an LAL assay or another validated method to confirm removal efficacy [6] [14].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Endotoxin Removal and Detection
| Item Name | Function/Brief Explanation | Example Source/Reference |
|---|---|---|
| Triton X-114 | A non-ionic detergent used in temperature-driven phase separation to partition endotoxins away from the target protein. | MP Biomedicals [6] |
| Polymyxin B Agarose Resin | An affinity chromatography matrix. The antibiotic Polymyxin B binds specifically to the lipid A domain of endotoxin, neutralizing and removing it from solution. | EndotoxinOUT Kits [12] |
| HEK-Blue hTLR4 Cells | A reporter cell line used to biologically validate endotoxin removal. These cells express the human Toll-like receptor 4 (TLR4) complex and secrete SEAP upon endotoxin stimulation. | InvivoGen [6] |
| Limulus Amebocyte Lysate (LAL) | The standard reagent for quantifying endotoxin levels, based on the clotting enzyme cascade from horseshoe crab blood. | FDA-approved test method [13] |
| Endotoxin ELISA Kit | An immunoassay kit for the quantitative detection of endotoxin in various samples, such as serum, plasma, and cell culture supernatants. | Various suppliers [14] |
| Detergent Removal Spin Columns | Used to remove residual detergent (like Triton X-114) from protein samples after phase separation, preparing them for cell culture or other sensitive applications. | Thermo Scientific [6] |
Endotoxin-Induced Signaling Pathway to Septic Shock
Understanding the body's extreme response to endotoxins underscores the critical importance of their removal from therapeutics. The following diagram outlines the key pathway from exposure to the critical state of septic shock.
Frequently Asked Questions
Q1: What are the most common sources of endotoxin contamination in a laboratory setting? The most common sources of endotoxin contamination include the bacterial hosts used for recombinant protein expression (particularly E. coli), laboratory water, and raw materials like cell culture media and sera [15] [16]. Endotoxins are lipopolysaccharides (LPS) from the outer membrane of Gram-negative bacteria and are released in large amounts upon bacterial death and lysis [15] [9]. A single E. coli cell contains about 2 million LPS molecules, which can easily co-purify with the target protein or DNA [15] [16]. Contamination can also spread via contaminated air, human skin, and inadequately treated glassware or plasticware [16].
Q2: How sensitive are human immune cells to endotoxin contamination? Certain human immune cells are exquisitely sensitive to endotoxins. Research shows that primary human CD1c+ dendritic cells can be activated by LPS concentrations as low as 0.002–2 ng/ml, which is equivalent to the levels of endotoxin contamination sometimes found in commercially available recombinant proteins [17]. This high sensitivity is closely correlated with high CD14 expression levels on these cells. Such low-level contamination can lead to erroneous data in experiments involving sensitive cell types.
Q3: What are the regulatory endotoxin limits for injectable products? For products administered parenterally (by injection) to humans and preclinical animal models, the endotoxin limit is set at 5.0 Endotoxin Units (EU) per kilogram of body weight when administered over one hour [18] [4]. For intrathecal injections, the limit is much stricter at 0.2 EU/kg [18]. For specific materials like Water for Injection (WFI), the limit is 0.25 EU/ml [18]. In practice, the goal for research and therapy is to maintain endotoxin levels as low as possible to prevent adverse effects.
Q4: Why is standard autoclaving insufficient for endotoxin removal? Endotoxins are remarkably heat-stable, so standard autoclaving or sterilization protocols do not effectively destroy them [16]. To destroy endotoxins on glassware, dry-heat depyrogenation at high temperatures for extended periods is required, such as 180°C for 4 hours or 250°C for 30 minutes [18] [16].
Troubleshooting Guide: Identifying and Addressing Contamination
Problem: Inconsistent Cell Culture Results or Unexplained Immune Activation
Potential Cause: Endotoxin contamination in your recombinant protein preparation or cell culture reagents.
Diagnostic Steps:
- Test Your Reagents: Use a Limulus Amebocyte Lysate (LAL) assay to quantify endotoxin levels in your recombinant proteins, buffers, and culture media [17] [18] [16]. The LAL assay is the standard method and comes in gel-clot, turbidimetric, and chromogenic formats [18] [4].
- Check Your Water Source: Laboratory pure water is a very common source of endotoxins. Ensure your water purification system is well-maintained and that the water used for preparing buffers and media is endotoxin-free [16] [4].
- Inspect Your Plasticware and Glassware: Use only certified pyrogen-free plasticware. Be aware that endotoxins adhere strongly to glass; standard washing and autoclaving will not remove them [15] [16].
Solutions:
- For Contaminated Proteins: Purify the protein using an appropriate endotoxin removal method (see Table 2 and the protocol below).
- For Contaminated Water: Replace with certified endotoxin-free water.
- For Contaminated Glassware: Discard if possible, or decontaminate by baking at 180°C overnight [15] [16].
Problem: Low Transfection Efficiency in Sensitive Cell Lines
Potential Cause: Endotoxin contamination in plasmid DNA preparations. Endotoxins can significantly reduce transfection efficiency, especially in primary cells and sensitive cultured cell lines [15].
Diagnostic Steps: Measure the endotoxin level in your plasmid DNA preparation using an LAL assay. The table below compares endotoxin levels and resulting transfection efficiency for different plasmid purification methods [15]:
Table 1: Endotoxin Contamination and Transfection Efficiency of Various Plasmid Prep Methods
| Plasmid Preparation Method | Endotoxin (EU†/µg DNA) | Relative Transfection Efficiency |
|---|---|---|
| EndoFree Plasmid Kits | < 0.04 | 154% |
| QIAGEN Plasmid Plus Kits | < 1.0 | 100% |
| QIAGEN Plasmid Kits | 9.3 | 100% |
| 2x CsCl Gradient Centrifugation | 2.6 | 99% |
| Silica Slurry | 1230 | 24% |
Solutions: Switch to an endotoxin-removing or endotoxin-free plasmid purification kit, such as those listed in the table above, which integrate a specific step to prevent LPS from binding to the purification resin [15].
Endotoxin Removal Method Comparison
Various techniques can be employed to remove endotoxins from protein samples. The choice of method depends on the properties of your target protein and the required level of purity.
Table 2: Comparison of Endotoxin Removal Methods
| Technology | Mechanism | Efficiency | Specificity | Key Limitations |
|---|---|---|---|---|
| Affinity Chromatography | Ligand (e.g., polymyxin B) binds LPS with high specificity [9] [19]. | High (≥90%) [19] | High | Can be expensive; may require pH/salt optimization [9]. |
| Ion Exchange Chromatography | Endotoxins (pI~2) bind to resin under appropriate pH conditions [9]. | High | Medium | Sensitive to pH and salt conditions; may bind highly charged target proteins [9]. |
| Phase Separation (Triton X-114) | Temperature-induced separation; endotoxins partition into detergent phase [9]. | Moderate (45-99%) [9] | Low | Risk of detergent residue; may degrade sensitive proteins [9]. |
| Ultrafiltration | Physical separation based on size of endotoxin micelles (>100 kDa) [9]. | Moderate (28.9-99.8%) [9] | Low | Fails to remove smaller endotoxin forms [9]. |
| Activated Carbon Adsorption | Non-specific adsorption to large surface area [9]. | High (~93.5%) [9] | Low | Non-selective; can cause significant product loss [9]. |
Detailed Protocol: Endotoxin Removal via Triton X-114 Phase Separation
This is a referenced protocol for removing endotoxins from recombinant proteins using Triton X-114 phase separation [9].
- Addition of Triton X-114: Add Triton X-114 to the protein sample to achieve a final concentration of 1% (v/v).
- Low-Temperature Incubation (4°C): Incubate the mixture at 4°C for 30 minutes with constant stirring to ensure complete solubilization and a homogeneous solution.
- High-Temperature Phase Separation (37°C): Transfer the sample to a 37°C water bath and incubate for 10 minutes. The solution will become cloudy as it separates into two phases: a detergent-rich phase (containing the endotoxins) and an aqueous phase (containing the target protein).
- Centrifugation: Centrifuge at 20,000 × g for 10 minutes at 25°C to fully separate the two phases.
- Collection of Aqueous Phase: Carefully aspirate and collect the upper, clear aqueous phase, which contains your target protein. Take care to avoid the lower, viscous detergent phase.
- Repeat Phase Separation (Optional): To further reduce endotoxin levels, subject the collected aqueous phase to 1–2 additional rounds of Triton X-114 phase separation (repeat steps 1–5).
- Endotoxin Quantification: Measure the endotoxin level in the final aqueous phase using a Limulus Amebocyte Lysate (LAL) assay to confirm the success of the removal process.
TLR4-Mediated Endotoxin Signaling Pathway
Endotoxins like LPS trigger a potent immune response by activating the Toll-like Receptor 4 (TLR4) pathway on innate immune cells. The following diagram illustrates the key steps in this signaling cascade, which culminates in the release of pro-inflammatory cytokines [17] [4].
The Scientist's Toolkit: Essential Reagents for Endotoxin Management
Table 3: Key Reagents and Kits for Endotoxin Detection and Removal
| Item | Function | Example Use Case |
|---|---|---|
| LAL Assay Kit | Quantifies endotoxin levels in samples via gel-clot, turbidimetric, or chromogenic methods [18] [4]. | Routine testing of purified proteins, buffers, and culture media before use in sensitive cell-based assays. |
| High-Capacity Endotoxin Removal Resin | Affinity resin (e.g., cellulose with poly(ε-lysine)) that selectively binds endotoxins for removal from protein solutions [19]. | Rapidly cleaning up contaminated antibody or protein samples with high recovery (>85%) and >90% endotoxin removal [19]. |
| Endotoxin-Free Plasmid Kits | DNA purification kits with a dedicated buffer to remove endotoxins during the protocol [15]. | Preparing transfection-grade DNA for sensitive cells like primary immune cells, where efficiency is critical. |
| Endotoxin-Free Water & Buffers | Certified, sterile fluids guaranteed to have endotoxin levels below a specified limit (e.g., <0.005 EU/mL). | Preparing all solutions for cell culture and protein work to prevent the introduction of contaminants. |
| Triton X-114 | Non-ionic detergent used for temperature-driven phase separation to remove endotoxins from proteins [9]. | A cost-effective method for bulk removal of endotoxins from recombinant proteins that are stable in the presence of detergent. |
Bacterial Endotoxin Testing (BET) is a critical safety requirement for parenteral drugs and medical devices. The United States Pharmacopeia (USP) chapter <85> and the European Pharmacopoeia (EP) chapter 2.6.14 are the harmonized standards that outline the validated methods for this testing. These chapters describe the use of Limulus Amebocyte Lysate (LAL) for detecting and quantifying endotoxins. A cornerstone of these regulations is the establishment of an endotoxin tolerance limit, calculated using the K/M formula, to ensure that a product dose, when administered to a patient, will not elicit a pyrogenic response [18]. Adherence to these standards is non-negotiable for the release of products for human use, making them foundational to quality control in recombinant protein research and pharmaceutical manufacturing.
FAQ: Understanding the Standards and Calculations
Q1: What is the fundamental purpose of USP <85> and EP 2.6.14? The primary purpose of these harmonized chapters is to provide the standards and procedures for the Bacterial Endotoxins Test (BET). This test uses Limulus Amebocyte Lysate (LAL) to detect and quantify the presence of bacterial endotoxins, which are pyrogenic lipopolysaccharides from gram-negative bacteria, in pharmaceutical products, medical devices, and raw materials [18] [20]. The test ensures patient safety by preventing febrile reactions that can be caused by contaminated injectable drugs or devices.
Q2: How is the endotoxin acceptance limit for my drug product calculated? The acceptance limit is derived from the formula K/M, which sets the maximum allowable endotoxin level per unit of product [18].
- K is the threshold pyrogenic dose of endotoxin per kilogram of body weight. It is defined as:
- 5.0 EU/kg for most intravenous and intramuscular products.
- 0.2 EU/kg for intrathecal drug products, due to the heightened sensitivity of the central nervous system.
- M is the maximum human dose per kilogram of body weight that would be administered in a single one-hour period. This is the larger of either the maximum recommended human dose from the product labeling or the dose used in the rabbit pyrogen test.
The resulting limit is expressed as EU/mL for liquids or EU/mg for solids.
Q3: Can you provide an example of the K/M calculation? Yes. The FDA provides a clear example for Cyanocobalamin Injection [18]:
- Product: Cyanocobalamin Injection
- Potency: 1000 mcg/mL
- Maximum Human Dose (M): 14.3 mcg/kg (as per product labeling)
- Endotoxin Limit (K/M): = 5.0 EU/kg / 14.3 mcg/kg = 0.35 EU/mcg
- Conversion to EU/mL: Multiply by the product potency: 1000 mcg/mL × 0.35 EU/mcg = 350 EU/mL
This means each milliliter of Cyanocobalamin Injection must contain no more than 350 Endotoxin Units (EU).
Q4: Are there specific products with predefined endotoxin limits? Yes. Certain products, like waters for pharmaceutical use, have predefined limits because the administered volume can be large and variable. According to the USP [18]:
- Water for Injection, Sterile Water for Injection, and Sterile Water for Irrigation: ≤ 0.25 EU/mL
- Bacteriostatic Water for Injection and Sterile Water for Inhalation: ≤ 0.5 EU/mL
Q5: What are the four principal LAL test methods recognized by the pharmacopeias? The four basic methods approved for end-product release testing are [18] [20]:
- Gel-Clot: A qualitative or semi-quantitative method based on clot formation.
- Turbidimetric: A quantitative method that measures the increase in turbidity.
- Chromogenic: A quantitative method that uses a synthetic chromogenic substrate to produce a color change.
- Colorimetric (Lowry protein): Another quantitative color-based method.
Table 1: Comparison of Compendial Bacterial Endotoxin Test Methods
| Method | Principle | Detection | Output | Key Advantage | Key Disadvantage |
|---|---|---|---|---|---|
| Gel-Clot | Clot formation | Visual | Qualitative / Semi-quantitative | Considered the most sensitive and accurate; less susceptible to interference [20] | Time-consuming; subjective; not automated [20] |
| Turbidimetric | Turbidity development | Spectrophotometric | Quantitative | Quantitative result based on gel-clot principle [20] | Susceptible to interference from turbid or colored samples [18] |
| Chromogenic | Chromophore release | Spectrophotometric (405 nm) | Quantitative | User-friendly; can be automated [20] | Can be interfered with by colored samples or those that cause precipitation [18] [20] |
| Kinetic Assays | Turbidity or color development over time | Spectrophotometric | Quantitative | Automated; provides insights into assay performance; improved data integrity [21] | Requires specialized instrumentation and software [21] |
Troubleshooting Common Endotoxin Testing Issues
Problem 1: Invalid Assay or Inhibition/Enhancement The test sample interferes with the LAL reaction, either inhibiting it (leading to false negatives) or enhancing it (leading to false positives).
- Root Cause: Sample properties such as pH outside the range of 6.0-8.0, high viscosity, or the presence of interfering substances like chelating agents (EDTA), denaturants, strong acids/bases, or organic solvents [18] [20].
- Solution:
- Dilution: The most common approach. Dilute the sample to reduce the concentration of the interfering substance, but ensure the dilution does not exceed the Maximum Valid Dilution (MVD).
- pH Adjustment: Neutralize the sample to a pH between 6.0 and 8.0 using endotoxin-free acid, base, or buffers [20].
- Validation: The method must be validated for the specific product. This involves spiking the product with a known amount of endotoxin and demonstrating that the recovery is within 50%-200% of the known value to prove the interference has been overcome [18].
Problem 2: High Variability in Replicate Measurements The coefficient of variation (CV) between duplicate or replicate samples exceeds the acceptable limit (often 10% or 25%) [20].
- Root Cause: Inconsistent pipetting technique, improper mixing of reagents and sample, or using reagents from different manufacturers [18].
- Solution:
Problem 3: False Positive Results The test indicates the presence of endotoxin when there is none.
- Root Cause:
- Solution:
- Use Specific Reagents: Employ LAL reagents that are resistant to β-glucans, or switch to recombinant Factor C (rFC) or recombinant Cascade Reagent (rCR) methods, which are not activated by glucans [22] [23].
- Sample Treatment: For colored samples, use a method less susceptible to interference, such as the gel-clot method [20].
Experimental Protocol: Inhibitory/Enhancing Factor Testing
This protocol is essential for validating that your sample matrix does not interfere with the LAL test, as required by USP <85> and EP 2.6.14.
Objective: To demonstrate that the sample under test does not inhibit or enhance the LAL reaction, ensuring accurate endotoxin quantification.
Materials:
- Test sample (recombinant protein solution)
- LAL reagent (gel-clot, chromogenic, or turbidimetric)
- Endotoxin Standard Control (ESC)
- Endotoxin-free water (LRW)
- Depyrogenated glassware or plasticware
- Water bath or microplate reader (temperature-controlled at 37°C ± 1°C)
Procedure:
- Preparation of Spiked Sample (Test for Interference):
- Prepare a dilution of the test sample at the planned Maximum Valid Dilution (MVD).
- Create the "Spiked Product" by adding ESC to this dilution to achieve a concentration of 2λ, where λ is the sensitivity of the LAL reagent.
- Create the "Unspiked Product" by adding an equal volume of LRW to another aliquot of the diluted sample.
Preparation of Positive Controls:
- Create a "Positive Product Control (PPC)" by adding ESC to LRW to a concentration of 2λ.
- Create a "Negative Control" using LRW only.
Assay Performance:
- Test all four preparations (Spiked Product, Unspiked Product, PPC, and Negative Control) in duplicate using your chosen LAL method (e.g., kinetic chromogenic).
- Incubate at 37°C for the specified time.
Calculation and Acceptance Criteria:
- Calculate the mean measured endotoxin concentration in the Spiked Product and the PPC.
- The test is valid if: The Negative Control shows no detectable endotoxin, and the result for the PPC is within 50%-200% of the known 2λ concentration.
- The sample is non-interfering if: The measured endotoxin concentration in the Spiked Product is within 50%-200% of the measured concentration in the PPC [18]. If recovery is outside this range, the sample is interfering, and further dilution or treatment is required.
Visualizing the Endotoxin Detection Pathways
The following diagrams illustrate the key enzymatic cascades involved in traditional LAL and modern recombinant testing methods.
Diagram 1: Traditional LAL Cascade with Potential for False Positives. This pathway shows how endotoxin (LPS) activates Factors C, B, and the pro-clotting enzyme, leading to clot formation. It also highlights how (1,3)-β-D-Glucan can activate Factor G, causing a false positive result [22] [23] [20].
Diagram 2: Recombinant Factor C (rFC) Pathway. This animal-free method uses a single recombinant enzyme (Factor C) that is activated specifically by endotoxin. It then cleaves a synthetic fluorogenic substrate to produce a measurable signal. This pathway is not activated by β-Glucans, eliminating a major source of false positives [24] [23].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Endotoxin Testing and Contamination Control
| Item | Function/Description | Key Considerations for Recombinant Protein Research |
|---|---|---|
| LAL Reagents | Aqueous extract from horseshoe crab blood cells used to detect endotoxin. | Available in gel-clot, chromogenic, and turbidimetric formats. Choose based on required sensitivity and equipment [22] [20]. |
| Recombinant Reagents (rFC/rCR) | Animal-free reagents produced via recombinant DNA technology. | rFC is a single protein, while rCR mimics the natural LAL cascade. Both eliminate false positives from β-glucans and support sustainability [24] [23]. |
| Endotoxin Standards | Known concentrations of endotoxin used to create standard curves and validate tests. | Critical for determining assay sensitivity (λ) and performing spike-and-recovery studies for validation [18]. |
| Endotoxin-Free Water | Water with non-detectable levels of endotoxin, used for reconstituting reagents, dilutions, and controls. | Essential for preventing background contamination that can compromise results. Typically < 0.005 EU/mL [25]. |
| Depyrogenation Tools | Processes to destroy endotoxins on equipment. | Dry Heat: The standard method for glassware (e.g., 250°C for 45 minutes) [26]. Washing: For heat-sensitive materials, use endotoxin-free detergents followed by thorough rinsing with endotoxin-free water [26]. |
| Certified Plasticware | Tubes, pipette tips, and plates tested and certified to be low in endotoxins. | Prevents the introduction of endotoxins from lab consumables. Look for certification levels such as < 0.1 EU/mL [25]. |
Frequently Asked Questions (FAQs)
Q1: Why is endotoxin contamination a critical concern in my recombinant protein research? Endotoxins, or lipopolysaccharides (LPS), are potent immune stimulants found in the cell wall of Gram-negative bacteria like E. coli, a common host for recombinant protein production. Even trace amounts can have profound effects:
- Extreme Sensitivity: Some primary human immune cells, like CD1c+ dendritic cells, can be activated by concentrations as low as 0.002–2 ng/ml of LPS, a range equivalent to the residual contamination found in some commercial protein preparations [17].
- Diverse Experimental Artifacts: In vitro, endotoxins can distort cell membranes, induce cytokine production (e.g., IL-1β, IL-6, IL-8, IL-12, TNFα), alter gene expression, and cause cell death. These effects can completely obscure the true biological activity of your recombinant protein [17] [27].
- Pyrogenic Response: In vivo, endotoxins are pyrogenic and can cause fever, respiratory distress, and potentially fatal septic shock [27].
Q2: My protein is >95% pure by SDS-PAGE. Could it still have problematic endotoxin levels? Yes, absolutely. Standard purity analyses like SDS-PAGE cannot detect endotoxin contamination. A protein can be highly pure regarding other proteins but still carry significant amounts of LPS. Endotoxin is a chemical contaminant, not a proteinaceous one, and must be specifically tested for using methods like the LAL assay [17] [27].
Q3: What is the acceptable limit for endotoxin in my research samples? Acceptable limits depend on the application, particularly the sensitivity of your experimental system. For sensitive cell-based assays, especially those involving primary immune cells, you should aim for the lowest levels possible. The following table summarizes the minimal concentrations shown to activate sensitive cells, which can serve as a benchmark [17]:
| Cell Type | Minimum Activating LPS Concentration | Key Cytokines Produced |
|---|---|---|
| Primary Human CD1c+ Dendritic Cells | 0.002 ng/ml | IL-1β, IL-6, IL-8, IL-12, TNFα |
| Primary Human Monocytes | 0.02 ng/ml | IL-1β, IL-6, IL-8, IL-12, TNFα |
| THP-1 Monocytic Cell Line | 0.2 ng/ml | IL-1β, IL-6, IL-8, IL-12, TNFα |
Q4: How can I effectively remove endotoxins from my protein samples? Several chromatographic methods leverage the negative charge and hydrophobic properties of endotoxins. The choice of method depends on your protein's characteristics.
| Method | Principle | Key Consideration |
|---|---|---|
| Affinity Chromatography (e.g., Poly(ε-lysine) ligands) | Cationic ligands selectively bind endotoxins under physiological conditions [28]. | High selectivity for LPS without binding most proteins. |
| Immobilized Metal-Affinity Chromatography (IMAC) with detergent | His-tagged protein binds to Ni-NTA; endotoxin is washed away with non-ionic detergent before protein elution [29]. | Effective for His-tagged proteins; can achieve <0.2 EU/mg [29]. |
| Anion Exchange Chromatography | Binds negatively charged endotoxins at high pH, allowing protein to flow through [28]. | Requires pH-mediated destabilization of endotoxin structure. |
| Cation Exchange Chromatography | Binds positively charged protein at low pH (~4), allowing endotoxin to flow through [28]. | Suitable for basic proteins. |
| Novel Affinity Adsorbents (e.g., Factor C domains) | Uses immobilised LPS-binding domains (e.g., CES3) from horseshoe crab Factor C to specifically capture endotoxins [10]. | High specificity; can be produced in an LPS-free plant system [10]. |
Q5: How do I validate my endotoxin testing method to ensure accurate results? For the LAL test, a Positive Product Control (PPC) recovery validation is essential to rule out that your sample matrix is not inhibiting or enhancing the enzymatic reaction, which would lead to false negatives or positives [8]. This involves:
- Spiked Sample: Testing your sample spiked with a known amount of endotoxin standard (e.g., 0.5 EU/mL).
- Calculation: The measured endotoxin in the spiked sample must be within 50-200% of the known spike value to prove the test is valid for your product [30] [8]. For quantitative kinetic methods, this validation is built into each assay run [8].
Troubleshooting Guides
Problem: High Endotoxin Levels After Standard Affinity Purification
Potential Causes and Solutions:
Cause: Endotoxins are co-purifying with your protein via strong hydrophobic or charge interactions.
- Solution: Incorporate a specific endotoxin removal step. Use an affinity adsorbent like poly(ε-lysine)-cellulose beads (e.g., Cellufine ETclean) in a spin-column format. This can be done after your primary purification. Optimize the buffer conditions (ionic strength and pH) to maximize endotoxin binding while keeping your protein in solution [28].
- Solution: For His-tagged proteins, add a wash step with a non-ionic detergent (e.g., Triton X-114) to the IMAC column before elution. This protocol has been shown to reduce endotoxin to 0.2 EU/mg with nearly 100% protein recovery [29].
Cause: Your starting material (cell lysate) has an extremely high endotoxin load, overwhelming the purification system.
- Solution: Focus on prevention. Optimize fermentation to minimize bacterial lysis. If possible, use a purification tag that allows for purification under denaturing conditions (e.g., urea), which dissociates endotoxin aggregates and facilitates their removal [31].
Problem: Inconsistent Endotoxin Measurements with LAL Assay
Potential Causes and Solutions:
Cause: Matrix interference – components in your sample buffer are inhibiting or enhancing the LAL reaction.
Cause: The standard curve is invalid or the assay is not performed under controlled conditions.
- Solution: Ensure the correlation coefficient (r) of your standard curve is ≥ 0.980 [30]. Run the assay in a controlled environment and use validated, endotoxin-free labware. Routinely qualify your pipettes and microplate reader.
Experimental Protocols & Data Visualization
Protocol 1: Validated Kinetic Chromogenic LAL Test
This protocol is based on methods validated according to ICH Q2 and EU Pharmacopoeia guidelines for use as a limit test for impurities [30].
Research Reagent Solutions:
- LAL Reagent: Kinetic chromogenic LAL test kit (e.g., Pyrotell-T, EndoZyme).
- Endotoxin Standard: Certified reference standard endotoxin.
- Endotoxin-Free Water: Used for reconstitution and blanks.
Methodology:
- Reconstitution: Reconstitute the LAL reagent and endotoxin standard according to the manufacturer's instructions using endotoxin-free water.
- Standard Curve: Prepare at least three different concentrations of endotoxin standard in duplicate to generate a standard curve.
- Sample Preparation: Dilute the protein sample appropriately in endotoxin-free water. Include a positive product control (PPC) by spiking an aliquot of the diluted sample with the middle concentration of the standard curve (e.g., 0.5 EU/mL).
- Incubation: Add 100 µL of each standard, blank, unspiked sample, and PPC sample to a pyrogen-free microtiter plate. Add 100 µL of LAL reagent to each well.
- Measurement: Immediately place the plate in a pre-warmed microplate reader at 37°C. Measure the absorbance or fluorescence continuously (kinetic mode) for at least 90 minutes.
- Analysis: Calculate the standard curve using a non-linear regression model. The correlation coefficient must be ≥ 0.980. The time of signal onset (reaction time) is inversely proportional to the endotoxin concentration. The endotoxin concentration in the samples is calculated by comparing their reaction times to the standard curve. The PPC recovery must be between 50% and 200% for the test to be valid [30] [8].
Protocol 2: Endotoxin Depletion Using Affinity Adsorption
This protocol uses affinity matrices to selectively bind and remove endotoxins from protein solutions [28] [10].
Research Reagent Solutions:
- Affinity Matrix: Poly(ε-lysine)-cellulose beads (e.g., Cellufine ETclean) or Factor C domain (CES3)-immobilized cellulose beads.
- Binding/Wash Buffer: Physiological buffer (e.g., 20mM Tris, 150mM NaCl, pH 7.4). The ionic strength (µ) is critical for selectivity and should be optimized [28].
- Sterile, Endotoxin-Free Column or Spin Units.
Methodology:
- Equilibration: Equilibrate the affinity column or spin cartridge with 5-10 column volumes (CV) of your selected binding buffer.
- Sample Preparation: Adjust your protein sample's buffer to match the binding buffer using dialysis or desalting. Ensure the pH and ionic strength are within the optimal range for endotoxin binding and protein stability (e.g., µ = 0.05-0.4) [28].
- Loading: Load the prepared protein sample onto the equilibrated column. Collect the flow-through.
- Washing: Wash the column with 5-10 CV of binding buffer to recover any remaining protein. Combine the flow-through and wash fractions.
- Analysis: The combined protein-containing fraction should now have reduced endotoxin levels. Concentrate the protein if necessary and measure both protein concentration and endotoxin levels (see Protocol 1) to determine the specific activity (EU/mg).
Endotoxin Removal and Control Methods: A Practical Guide for Laboratory and Production
In recombinant protein research, controlling bioburden—the population of viable microorganisms on or in a product or material—is fundamental to preventing endotoxin contamination [32]. Endotoxins, lipopolysaccharides (LPS) from the outer membrane of Gram-negative bacteria, are potent pyrogens that can trigger severe inflammatory responses and compromise research integrity and patient safety [33] [34]. This technical support center provides a strategic framework for upstream bioburden control, offering detailed protocols, troubleshooting guides, and FAQs to help researchers safeguard their cell culture and fermentation processes.
Core Concepts: Bioburden and Endotoxins
What is Bioburden?
Bioburden refers to the total number of viable microorganisms (e.g., bacteria, fungi, and mold) present on a surface, in a substance, or within a material before sterilization [32] [35]. In upstream bioprocessing, this includes contaminants potentially introduced via raw materials, equipment, the environment, and personnel. Controlling bioburden is critical because it is the primary source of endotoxins; when Gram-negative bacteria die or lyse, they release these toxic, heat-stable molecules into the process stream [32] [34].
Bioburden vs. Endotoxin Testing
It is essential to distinguish between bioburden and endotoxin testing, as they evaluate different quality attributes. The table below summarizes their key differences:
Table 1: Key Differences Between Bioburden and Endotoxin Testing
| Attribute | Bioburden | Endotoxin |
|---|---|---|
| Definition | Total number of viable microorganisms [33] | Toxic substances (LPS) in the outer membrane of Gram-negative bacteria [33] |
| Measurement | Colony-forming units (CFU) [33] | Endotoxin Units (EU) [33] |
| Origin | Air, water, raw materials, personnel [32] [33] | Gram-negative bacteria (e.g., E. coli, Pseudomonas) [33] |
| Health Impact | Indicates contamination risk; can cause product spoilage [33] | Causes fever, inflammation, septic shock [33] [34] |
| Testing Methods | Membrane filtration, direct plate method [35] | Limulus Amebocyte Lysate (LAL) assay, recombinant Factor C (rFC) assay [33] |
Strategic Prevention Framework
A proactive, multi-layered approach is the most effective way to minimize bioburden and subsequent endotoxin contamination.
Source Control
- Raw Materials: Audit suppliers to ensure they exercise documented control over bioburden and endotoxin levels [34]. Test high-risk materials, such as those of natural origin or with high water content.
- Water Systems: Implement rigorous validation and control for water generation and distribution systems, as water is a common source of Gram-negative bacteria and biofilm formation [34].
- Personnel: Provide comprehensive training on aseptic techniques, hygiene, and proper gowning procedures to minimize contamination from operators [32].
Process and Filtration Controls
Sterile filtration is a cornerstone of upstream bioburden control. A multi-stage filtration strategy protects the bioreactor and downstream processes.
Upstream Filtration Strategy for Bioburden Control
- Prefiltration: Uses depth filters (e.g., polypropylene or glass fiber fleece) to remove coarse particles and protect downstream filters. This is ideal for clarifying complex or viscous feedstreams [36].
- Bioburden Reduction: Acts as a pre-sterilization filter to lower the microbial load, protecting the final sterilizing-grade filter and extending its lifespan [37] [36].
- Sterilizing-Grade Filtration: A 0.2 µm membrane filter that serves as the final barrier, ensuring 100% bacteria retention for aseptically added fluids [37].
Environmental and Sanitation Controls
- Cleanroom Management: Maintain controlled environments with advanced air filtration (e.g., HEPA) to minimize airborne contamination [32]. Implement rigorous cleaning and disinfection procedures for all equipment and surfaces [32] [34].
- Endotoxin-Specific Cleaning: Use cleaning tools scientifically proven to remove and retain sub-micron endotoxin debris to prevent cross-contamination [34].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Bioburden and Endotoxin Control
| Item | Function | Key Characteristics & Examples |
|---|---|---|
| Prefilters | Removes coarse particles and colloids to protect and extend the life of final filters [36]. | High dirt-holding capacity. e.g., Sartopure PP3 (polypropylene fleece), Sartopure GF Plus (charged glass fiber) [36]. |
| Bioburden Reduction Filters | Reduces microbial load in fluids before the final sterilizing-grade filter [37] [36]. | Typically 0.1-0.2 µm pore size. e.g., Sartoguard PES (dual-layer PES membrane) [36]. |
| Sterilizing-Grade Filters | Provides a final sterile barrier with 100% bacteria retention for aseptically added fluids [37]. | 0.2 µm pore size. e.g., PPS filters (hydrophilic, dual-layer membrane) [37]. |
| Water Purification Systems | Produces high-purity water to prevent the introduction of microbes and endotoxins via water [34]. | Systems designed to control biofilm formation in generation and distribution loops. |
| LAL/rFC Reagents | Detects and quantifies endotoxin levels in process samples and final products [33]. | Limulus Amebocyte Lysate (LAL) or recombinant Factor C (rFC) for highly sensitive endotoxin testing. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: My process fluid has a very high particle load, and my sterilizing filters are clogging too quickly. What can I do? A: Implement a robust prefiltration strategy. Using a series of depth filters with progressively smaller pore sizes (e.g., starting with a 1.2 µm filter and moving to a 0.65 µm filter) can remove the bulk of the particles and colloids. This protects the more expensive sterilizing-grade filter, reduces change-out frequency, and lowers overall costs [37] [36].
Q: I need to filter a sensitive protein solution. How can I reduce bioburden without losing my product? A: For sensitive biologics like proteins, a bioburden reduction filter with low protein-binding properties is recommended. Filters made of modified Polyethersulfone (PES) are often suitable. It is critical to perform a compatibility and yield study with your specific product during process development to select the optimal filter that minimizes adsorption while effectively reducing microbial load [36].
Q: Our endotoxin tests are failing, but our bioburden results are low. Why is this happening? A: This discrepancy is possible. Bioburden testing only detects viable microorganisms, while endotoxins are stable toxins released from dead Gram-negative bacteria [33]. Your process may be effectively killing bacteria (e.g., via a biocide) but failing to remove the endotoxins they have already released. Investigate sources of Gram-negative bacteria in your water systems, raw materials, and dead legs in process equipment where biofilms can form [34].
Q: Is it necessary to perform both bioburden and endotoxin testing? A: Yes, for a comprehensive contamination control strategy, both are often required. Bioburden testing is typically performed on non-sterile samples as part of validation and periodic monitoring to ensure sterilization processes are effective. Bacterial endotoxin testing is required on a lot-by-lot basis for parenteral products or devices labeled as "non-pyrogenic" to ensure they are safe for patient use [33].
Troubleshooting Common Scenarios
Table 3: Troubleshooting Guide for Bioburden Control
| Problem | Potential Root Cause | Corrective & Preventive Actions |
|---|---|---|
| Consistently High Bioburden in Cell Culture Media | - Contaminated raw materials.- Inadequate sterilization of media or feed tanks.- Biofilm in water system or transfer lines. | - Audit and test raw material suppliers [34].- Validate thermal or filter sterilization cycles.- Increase sanitization frequency of water systems and process equipment [34]. |
| Unexpected Spike in Endotoxin Levels | - Breakdown in aseptic technique.- Gram-negative biofilm dislodged from equipment.- Compromised sterile filter. | - Retrain personnel on aseptic practices [32].- Inspect and clean equipment for biofilm hotspots [34].- Perform integrity testing on sterilizing-grade filters. |
| Rapid Fouling of Sterilizing Filters | - High particulate load in feed fluid.- Inadequate or missing prefiltration step. | - Add or optimize a prefilter train for gradual particle removal [37] [36].- Analyze fluid composition to select the optimal prefilter media (e.g., fleece for high capacity, membrane for precise retention) [36]. |
Experimental Protocols
Protocol: Validating a Bioburden Testing Method for a Fluid
This protocol ensures your bioburden testing method accurately recovers microorganisms from your process fluid.
- Sample Preparation: Use a sterile lot of your process fluid (e.g., culture media or buffer).
- Inoculation: Inoculate the fluid with a known, low concentration (e.g., 10-100 CFU) of standard organisms, such as Bacillus atrophaeus spores (aerobic) and Pseudomonas aeruginosa (Gram-negative) [33].
- Extraction & Enumeration: Process the inoculated sample according to your chosen method (e.g., membrane filtration). Culture the filters and enumerate the recovered colonies.
- Calculation: Calculate the method's recovery efficiency by comparing the number of recovered organisms to the number in the original inoculum.
- Recovery Efficiency (%) = (Number of CFU Recovered / Number of CFU Inoculated) x 100
- Validation Criterion: A recovery rate of ≥50% is often considered acceptable, demonstrating that the method does not inhibit microbial growth and provides a valid count [33].
Protocol: Routine Environmental Monitoring for Bioburden
Regular monitoring of the manufacturing environment is crucial for proactive contamination control [35].
- Surface Monitoring: Use contact plates (RODAC plates) containing a general nutrient agar (like Tryptic Soy Agar) to sample critical surfaces (e.g., bioreactor ports, workbenches) after processing.
- Air Monitoring: Use an active air sampler to draw a measured volume of air from the critical zone (e.g., near the fluid addition port) onto an agar plate.
- Incubation: Incubate the plates as per guidelines (e.g., 20-25°C for 5-7 days for fungi and 30-35°C for 3-5 days for bacteria) [35].
- Data Interpretation: Count the colonies and compare them to established alert and action limits. Investigate any breaches of action limits to identify and eliminate the contamination source.
Effective upstream bioburden control in cell culture and fermentation is not a single action but a continuous, multi-layered strategy. It integrates rigorous source control, a well-designed filtration train, disciplined environmental monitoring, and thorough testing. By adopting the preventative measures, troubleshooting guides, and protocols outlined in this technical support center, researchers and drug development professionals can significantly mitigate the risks of bioburden and endotoxin contamination, thereby ensuring the safety, quality, and success of their recombinant protein research and production.
Frequently Asked Questions (FAQs)
FAQ 1: What are the key mechanisms of ultrafiltration and size exclusion chromatography for endotoxin separation?
- Ultrafiltration (UF) relies on size-based exclusion using membranes with a specific molecular weight cutoff (MWCO). Endotoxin aggregates (>100 kDa) are retained while smaller proteins pass through [9] [38].
- Size Exclusion Chromatography (SEC) separates molecules based on their hydrodynamic volume and how they partition between the mobile phase and the pores of the resin. Larger molecules, like endotoxin micelles, elute first, while smaller molecules elute later [39].
FAQ 2: When should I choose ultrafiltration over size exclusion chromatography? The choice depends on your sample characteristics and process goals. The following table compares the core features of each method:
| Feature | Ultrafiltration (UF) | Size Exclusion Chromatography (SEC) |
|---|---|---|
| Primary Mechanism | Size-based sieving through a membrane [9] | Size-based partitioning into resin pores [39] |
| Endotoxin Removal Efficiency | 28.9% to 99.8% [9] | Varies; can be limited by aggregate size [39] |
| Best Suited For | Small peptides and APIs significantly smaller than endotoxin aggregates [38] | Separating proteins from larger endotoxin micellar structures [39] |
| Process Scalability | Highly scalable for large volumes [9] | Scalable, but resin volume and flow rates can be limiting |
| Key Limitations | Low filtration rates with viscous products; ineffective if protein size is similar to endotoxins [38] | Limited resolution if endotoxins form small aggregates or bind to proteins [39] |
FAQ 3: Why is my endotoxin removal efficiency low with a 10 kDa ultrafiltration membrane? Low efficiency can occur due to:
- Protein Concentration: High protein concentrations can shield endotoxins or increase solution viscosity [9].
- Endotoxin Aggregation State: Endotoxins can form vesicles of 300-1000 kDa, but may also exist in smaller forms that pass through the membrane [38].
- Molecular Interactions: Stable endotoxin-protein complexes can form, preventing their separation by size alone [40] [38].
- Detergent Interference: The presence of detergents can disrupt endotoxin aggregates, reducing their effective size [9].
FAQ 4: Can these methods handle all my protein samples? No. These physical methods are highly dependent on the size difference between your target protein and the endotoxin aggregates. They are generally ineffective for proteins with a molecular weight close to or larger than that of the endotoxin micelles [38]. Furthermore, if endotoxins form stable, bound complexes with your protein of interest, charge-based or affinity methods may be required [39] [38].
Troubleshooting Guides
Problem 1: Poor Endotoxin Clearance in Ultrafiltration
Potential Causes and Solutions:
Cause: Incorrect Membrane Molecular Weight Cutoff (MWCO)
- Solution: Use a membrane with a 100 kDa MWCO, which is more effective for retaining large endotoxin aggregates while allowing smaller proteins to pass through [9].
- Preventive Action: Characterize the aggregate size of endotoxins in your specific solution buffer, as it can vary.
Cause: Low Transmembrane Pressure or Flow Rate
- Solution: For Tangential Flow Filtration (TFF), optimize the cross-flow rate and transmembrane pressure to maintain a stable flux without forming a polarized gel layer that can foul the membrane.
- Diagnostic Step: Monitor the filtrate flow rate. A declining rate indicates membrane fouling or concentration polarization.
Cause: Endotoxin-Protein Complexation
Problem 2: Inadequate Separation in Size Exclusion Chromatography
Potential Causes and Solutions:
Cause: Protein and Endoxin Co-Elution
- Solution: Ensure the resin pore size is appropriate. Smaller pores enhance the separation of smaller proteins from larger endotoxin structures via size exclusion [9].
- Alternative Approach: If co-elution persists, consider using an anion-exchange resin in void-exclusion mode (VEAX), where the protein is repelled and elutes first while the negatively charged endotoxin binds to the resin [41].
Cause: Sample Volume is Too Large
- Solution: The sample load volume should typically be 1-5% of the total column volume to achieve good resolution. Overloading will lead to poor separation.
- Corrective Action: Concentrate your sample and use a higher protein concentration with a smaller injection volume.
Cause: Endotoxin Aggregates are Disrupted
- Solution: Avoid solutions with high concentrations of detergents or solvents that can break down large endotoxin micelles into smaller monomers that co-elute with the target protein [39].
- Preventive Action: Use buffers that promote endotoxin aggregation, such as those containing divalent cations like Mg²⁺.
Experimental Protocols
Detailed Protocol: Endotoxin Removal via Ultrafiltration
This protocol outlines the steps for endotoxin removal from a recombinant protein solution using a 100 kDa molecular weight cutoff membrane [9] [38].
Research Reagent Solutions:
| Item | Function |
|---|---|
| 100 kDa MWCO Ultrafiltration Device | The core unit for size-based separation; can be a stirred cell or tangential flow filter. |
| Protein Buffer (e.g., PBS) | A compatible, low-endotoxin buffer to maintain protein stability and function. |
| Triton X-114 Detergent | A nonionic surfactant used to pre-treat samples and dissociate endotoxin-protein complexes [9]. |
| LAL Reagent Kit | For quantifying endotoxin levels before and after processing to validate removal efficiency [9]. |
Methodology:
- Sample Pre-treatment (Optional but Recommended): If endotoxin-protein complexes are suspected, add Triton X-114 to the protein sample to a final concentration of 1% (v/v). Incubate at 4°C for 30 minutes with constant stirring to create a homogeneous solution [9].
- System Setup and Equilibration: Assemble the ultrafiltration device according to the manufacturer's instructions. Pre-rinse the membrane with several volumes of endotoxin-free water, followed by equilibration with your protein buffer.
- Sample Processing: Load the protein solution into the ultrafiltration device. For stirred cells, apply gentle pressure (e.g., nitrogen gas) with constant stirring. For Tangential Flow Filtration (TFF), establish the recommended cross-flow rate and transmembrane pressure.
- Diafiltration: To enhance endotoxin removal, continuously add fresh buffer to the sample retentate at the same rate as the filtrate is being removed. This process dilutes and removes endotoxins from the retentate. A diafiltration volume of 5-10 is typical.
- Retentate Recovery: Once processing is complete, recover the concentrated protein solution from the retentate.
- Endotoxin Quantification: Use the LAL assay to measure endotoxin levels in both the initial sample and the final retentate to determine the removal efficiency [9].
Workflow Diagram: Ultrafiltration Process
The following diagram illustrates the key steps and decision points in the ultrafiltration process for endotoxin removal.
Decision Pathway: Selecting a Physical Separation Method
This flowchart provides a logical framework for deciding whether ultrafiltration or size exclusion is the most appropriate technique for a given experimental context.
FAQs on Endotoxin Removal in Recombinant Protein Research
Fundamental Concepts
1. What are endotoxins and why must they be removed from recombinant protein preparations? Endotoxins, also known as lipopolysaccharides (LPS), are toxic components found in the outer membrane of Gram-negative bacteria like E. coli, a common host for recombinant protein expression. They can bind to biomolecules during production and, if introduced into the bloodstream of a mammalian host, trigger severe immune responses such as inflammation or septic shock. Their removal is therefore critical to ensure the safety, reliability, and validity of proteins used in research, diagnostics, and therapeutics [9].
2. How do Ion Exchange, Affinity, and Multimodal Chromatography function in endotoxin removal? These techniques exploit different properties of endotoxins for separation:
- Ion Exchange Chromatography (IEX): Primarily uses charge differences. Endotoxins have a very low isoelectric point (pI~2), making them strongly negatively charged at most chromatographic pH levels. In Anion Exchange Chromatography (AEC), endotoxins bind to the positively charged resin, allowing the target protein to flow through if it is positively charged under the same conditions [9].
- Affinity Chromatography: Utilizes highly specific ligands immobilized on a solid support to bind endotoxins. Common ligands include Polymyxin B, histidine, or other specialized molecules that capture LPS. The target protein passes through while endotoxins remain bound to the ligand [42] [9].
- Multimodal Chromatography: Also known as Mixed-Mode Chromatography, it combines multiple interaction mechanisms, such as ion exchange and hydrophobic interaction, within a single resin. This provides more opportunities for effective separation, which is particularly valuable for challenging purifications, such as those involving proteins with low pIs or complex impurities [43].
Method Selection and Optimization
3. How do I choose the right chromatographic method for my protein? Selection depends on the properties of your target protein and the required purity. The table below compares the core methods.
Comparison of Endotoxin Removal Methods [9]
| Method | Efficiency | Specificity | Cost | Key Limitations |
|---|---|---|---|---|
| Affinity Chromatography | High | High | High | Expensive ligands; may require specific elution conditions |
| Ion Exchange Chromatography | High | Medium | Medium | Sensitive to pH and salt conditions; relies on charge differences |
| Phase Separation (Triton X-114) | Moderate | Low | Low | Potential for trace detergent residues in final product |
| Ultrafiltration | Moderate | Low | Low | Ineffective at removing small endotoxin aggregates |
| Adsorption (e.g., Activated Carbon) | High | Medium | Medium | Non-selective; can cause significant product loss |
For acidic proteins (low pI), anion exchange chromatography is often highly effective because the protein will not bind the resin, while endotoxins will. For sensitive proteins, a weak anion exchanger multimodal resin may be preferable as it can reduce binding strength and improve yield for low pI proteins [43]. When the primary goal is high specificity, affinity chromatography is the best choice, though at a higher cost [9].
4. What are key factors for optimizing an Ion Exchange Chromatography run?
- Selectivity and Capacity: The resin's selectivity for target ions and its exchange capacity are paramount. Capacity is influenced by pore size, surface area, and functional group density [44].
- Chemical Compatibility: Ensure the resin is compatible with your solution's pH, temperature, and concentration to avoid degradation [44].
- Binding and Elution Conditions: Optimize buffer pH and ionic strength to ensure endotoxins bind while your target protein does not. A common elution strategy employs a increasing salt gradient to disrupt ionic interactions [45].
Troubleshooting Common Issues
5. My protein recovery is low after Affinity Chromatography. What could be wrong? Low recovery in affinity purification can stem from several issues:
- Harsh Elution Conditions: Acidic elution buffers (e.g., glycine-HCl, pH 2.5-3.0) commonly used for elution can denature some proteins. Immediately neutralize collected fractions with a Tris buffer [45]. Consider testing milder elution conditions like competitive ligands or changes in ionic strength.
- Ligand Specificity: The affinity ligand (e.g., Polymyxin B) might also have some non-specific binding to your target protein. Re-evaluate the ligand's specificity or switch to a different purification mode [42] [19].
- Non-Specific Binding: Ensure your wash buffers contain low levels of detergent or appropriate salt to minimize non-specific ionic binding without eluting your target [45].
6. I'm seeing peak tailing and broadening in my Ion Exchange chromatogram. How can I fix this? Peak shape issues in IEX often relate to column packing or binding kinetics.
- Secondary Interactions: Tailing can arise from undesirable interactions between the protein and active sites on the resin. Try using a different resin with a more inert stationary phase [46].
- Column Overload: If the mass of the loaded sample is too high, it can lead to tailing or fronting. Reduce the injection volume or dilute your sample [46].
- Poor Column Packing or Voids: If all peaks are tailing, it may indicate a physical problem with the column, such as a void at the inlet. Examine the inlet frit, use a guard column, or consider replacing the column [46].
7. Endotoxin levels are still too high after a single purification step. What should I do? Achieving sufficient endotoxin clearance often requires a multi-faceted approach.
- Combine Orthogonal Methods: Use methods based on different principles sequentially. For example, a common and effective strategy is to use Triton X-114 phase separation followed by anion exchange chromatography [42] [9].
- Optimize and Repeat: Some methods, like Triton X-114 separation, can be repeated 1-2 times on the same sample to further reduce endotoxin levels [9].
- Verify Sample Conditions: For IEX, the efficiency is highly sensitive to pH. Confirm that the buffer pH ensures your protein and endotoxins are in the desired charge state [9].
Troubleshooting Guides
Chromatography Performance Issues
Liquid chromatography performance issues can be diagnosed systematically. The following workflow helps isolate the root cause of common problems like peak tailing, ghost peaks, and pressure fluctuations.
Troubleshooting LC Performance Issues
Endotoxin Clearance Failure
When endotoxin levels remain high post-purification, follow this logical pathway to identify and correct the problem.
Endotoxin Clearance Failure Guide
Detailed Experimental Protocols
Protocol 1: Endotoxin Removal by Triton X-114 Phase Separation
This is a highly effective method for removing endotoxins from recombinant protein preparations, with studies showing a reduction of greater than 99% and protein recovery over 90% [42].
Workflow Overview:
Triton X-114 Phase Separation Workflow
Materials and Reagents:
- Protein sample containing endotoxins.
- Triton X-114 detergent.
- Appropriate buffers (e.g., phosphate-buffered saline).
- Thermostatic water baths at 4°C and 37°C.
- Centrifuge capable of 20,000 × g.
- Limulus Amebocyte Lysate (LAL) assay kit for endotoxin quantification.
Step-by-Step Procedure [9]:
- Addition of Triton X-114: Add Triton X-114 to the protein sample to achieve a final concentration of 1% (v/v).
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring. This ensures complete solubilization and formation of a homogeneous solution.
- High-Temperature Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes. This induces phase separation into a detergent-rich phase (containing endotoxins) and an aqueous phase (containing the target protein).
- Centrifugation: Centrifuge the sample at 20,000 × g for 10 minutes at 25°C to fully separate the two phases.
- Collection of Aqueous Phase: Carefully aspirate and collect the upper aqueous phase, which contains the target protein. Take care to avoid contamination with the lower Triton X-114 detergent phase.
- Repeat Phase Separation (Optional): To further reduce endotoxin levels, subject the collected aqueous phase to 1–2 additional rounds of Triton X-114 phase separation (repeat steps 1–5).
- Endotoxin Quantification: Measure the endotoxin level in the final aqueous phase using a Limulus Amebocyte Lysate (LAL) assay to confirm reduction.
Protocol 2: Endotoxin Removal Using Affinity Resins
This protocol uses a specialized affinity resin with ligands designed to specifically bind endotoxins.
Materials and Reagents:
- High Capacity Endotoxin Removal Resin (e.g., Pierce).
- Spin columns.
- Equilibration buffer: Endotoxin-free phosphate-buffered saline (PBS), pH 7.2.
- Regeneration solutions: 0.2N NaOH and 2M NaCl.
- LAL assay kit and protein assay kit (e.g., BCA).
Step-by-Step Procedure (Spin-Column Method) [19]:
- Column Preparation: Centrifuge the storage spin column at 500 × g for 1 minute to remove the storage buffer.
- Column Regeneration (Optional): Wash the column sequentially with 0.2N NaOH, 2M NaCl, and finally with endotoxin-free water.
- Equilibration: Equilibrate the resin three times with endotoxin-free PBS, pH 7.2.
- Sample Binding: Apply the protein sample (in a buffer like PBS, pH 7.2) to the column. Incubate at room temperature (22°C) with gentle end-over-end mixing for 1 hour.
- Collection: Centrifuge the column at 500 × g for 1 minute to collect the purified flow-through sample.
- Analysis: Measure the endotoxin level in the flow-through using an LAL assay and determine protein recovery with a protein assay.
Performance Data of an Affinity Resin [19]: The table below demonstrates the efficiency of a high-capacity affinity resin in removing endotoxins from various proteins.
Endotoxin Removal from Different Proteins
| Protein | Molecular Weight (Da) | Isoelectric Point (pI) | Initial Endotoxins (EU/mL) | Endotoxin Removal (%) | Protein Recovery (%) |
|---|---|---|---|---|---|
| Cytochrome C | 12,000 | 10.6 | 10,000 | >99% | ≥85% |
| Myoglobin | 17,000 | 6.8 | 10,000 | >99% | ≥85% |
| BSA | 66,000 | 4.9 | 10,000 | >99% | ≥85% |
| BGG | 150,000 | 7.4 | 10,000 | >99% | ≥85% |
The Scientist's Toolkit: Essential Research Reagents
Key materials and their functions for setting up endotoxin removal experiments are listed below.
Essential Reagents for Endotoxin Removal Work
| Item | Function/Description | Key Considerations |
|---|---|---|
| Triton X-114 | A nonionic detergent used in temperature-induced phase separation to partition endotoxins into a detergent-rich phase [42] [9]. | Effective for proteins stable at 37°C; requires careful handling to avoid detergent residues. |
| Polymyxin B Agarose | An affinity resin where Polymyxin B is immobilized as a ligand to specifically bind and remove endotoxin [42]. | High specificity; ideal for final polishing steps. |
| High Capacity Endotoxin Removal Resin | A commercial affinity resin composed of cellulose and poly(ε-lysine) for highly effective, broad-spectrum endotoxin removal [19]. | Works across various protein sizes and pIs; high protein recovery. |
| Anion Exchange Resin (e.g., Q Sepharose) | A positively charged resin that binds negatively charged endotoxins, allowing proteins to flow through under appropriate pH conditions [9]. | Selectivity depends on the relative charge of the protein and endotoxin at the working pH. |
| Multimodal Anion Exchange Resin (e.g., Nuvia wPrime) | A resin with a weak anion exchanger functionality that combines charge and hydrophobic interactions for polishing difficult-to-separate samples [43]. | Useful for low pI proteins and complex impurities like aggregates and host cell proteins. |
| Limulus Amebocyte Lysate (LAL) | A reagent derived from horseshoe crab blood used in a gel-clot or chromogenic assay to detect and quantify endotoxin levels [42] [19]. | The gold-standard method for endotoxin detection; essential for validating purification success. |
Triton X-114 Properties and Specifications
What are the key physicochemical properties of Triton X-114 I should know for experiment planning?
Triton X-114 is a non-ionic detergent widely used for its unique temperature-dependent phase separation behavior. Below is a summary of its core properties for your experimental design. [47] [48]
| Property | Specification / Value |
|---|---|
| Type | Non-ionic detergent [47] [48] |
| Molecular Weight | Average 537 g/mol [47] |
| Molecular Formula | C14H22O•[C2H4O]8 or C28H50O8 [47] [48] |
| Critical Micelle Concentration (CMC) | 0.2 - 0.35 mM (20-25°C) [47] [48] |
| Cloud Point | ~23 °C [47] [48] |
| Pour Point | ~ -9 °C [47] |
| Hydrophile-Lipophile Balance (HLB) | 12.4 [47] |
Frequently Asked Questions (FAQs)
Why is Triton X-114 particularly effective for reducing endotoxin contamination in recombinant protein preparations?
Triton X-114 is effective because of its unique phase separation property at low temperatures (cloud point of 23°C). Endotoxins, which are lipopolysaccharides (LPS) from bacterial cell walls, are highly hydrophobic and partition preferentially into the detergent-rich phase when a Triton X-114 solution is warmed past its cloud point. In contrast, many recombinant proteins remain in the aqueous phase. By performing sequential cycles of cold-temperature solubilization and warm-temperature phase separation, you can efficiently separate your protein of interest from endotoxin contaminants. [47]
I am not seeing phase separation in my experiment. What could be going wrong?
Several factors can inhibit phase separation:
- Temperature: Ensure the solution is being incubated above the cloud point of 23°C. Use a controlled water bath or incubator for accuracy.
- Detergent Concentration: The final concentration of Triton X-114 must be high enough to form micelles and, upon heating, a detergent-rich phase. It should be well above the Critical Micelle Concentration (CMC of 0.2-0.35 mM). [47] [48]
- Solution Composition: High salt concentrations or certain buffer components can raise or lower the cloud point, interfering with separation. The protein sample itself can also affect this. You may need to empirically adjust buffer conditions. [49]
My protein is recovering in low yield after the phase separation. How can I improve this?
Protein loss can occur due to:
- Non-specific Binding: Phase-separating proteins can be notoriously "sticky" and adsorb to tube walls. Use low-binding tubes during the purification and phase separation steps. [49]
- Inadvertent Co-partitioning: If your protein has hydrophobic domains, it might be partitioning into the detergent phase with the endotoxins. Optimizing the buffer pH and salt composition can help. The buffer pH should be at least one unit away from the isoelectric point (pI) of your protein to maximize its solubility in the aqueous phase. [49]
- Protein Aggregation: Some proteins are aggregation-prone. Maintaining a moderate salt concentration and working at room temperature during initial purification can help prevent this. For extremely sensitive proteins, avoid freeze-thaw cycles by using freshly purified protein for phase separation assays. [49]
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| No phase separation | Incubation temperature below cloud point.Detergent concentration too low. | Incubate sample above 23°C (e.g., 30-37°C).Ensure final [Triton X-114] is >0.35 mM. |
| Low protein recovery | Protein is partitioning into detergent phase.Non-specific binding to tube walls.Protein precipitation. | Adjust buffer pH relative to protein pI.Use low-binding microcentrifuge tubes. [49]Include solubilizing tags (e.g., MBP) or arginine in buffer. [49] |
| High endotoxin levels persist | Insufficient separation cycles.Detergent-rich phase contamination during aqueous phase collection. | Perform 2-3 sequential cycles of phase separation.Carefully remove the aqueous phase after each centrifugation; leave a generous gap between phases. |
| Protein instability/aggregation | Harsh purification conditions.Repeated freeze-thaw cycles. | Purify in higher salt buffers and at room temperature if possible. [49]Aliquot protein, avoid freeze-thaw; use fresh if needed. [49] |
Experimental Protocol: Endotoxin Removal using Triton X-114 Phase Separation
This protocol provides a detailed methodology for using Triton X-114 to reduce endotoxin contamination from recombinant protein samples. [47] [49]
Workflow: Endotoxin Removal
Materials and Reagents
- Recombinant Protein Sample: Pre-purified, in a compatible buffer (e.g., Tris, PBS).
- Triton X-114 Detergent: 10% (v/v) stock solution in ultrapure water. [47]
- Low-Binding Microcentrifuge Tubes: Critical to minimize protein loss. [49]
- Temperature-Controlled Water Baths or Incubators: Set at 4°C and 37°C.
- Bench-top Centrifuge: Capable of maintaining 37°C.
Step-by-Step Procedure
- Preparation: Pre-cool a microcentrifuge tube and your protein sample on ice. Ensure the 10% Triton X-114 stock is liquid and mixed.
- Solubilization: Add Triton X-114 from the 10% stock to your protein sample to a final concentration of 2% (v/v). For example, add 20 µL of 10% Triton X-114 to 80 µL of protein sample.
- Equilibration: Mix the solution thoroughly but gently by pipetting or inversion. Incubate the mixture on ice for 15 minutes. This ensures complete solubilization and mixing.
- Phase Separation: Transfer the tube to a 37°C heat block or water bath. Incubate for 10 minutes. The solution will become cloudy, indicating the formation of a detergent-rich phase and an aqueous phase.
- Phase Separation: Centrifuge the tube at 13,000 x g for 10 minutes at 37°C. This ensures the two phases are cleanly separated. It is critical to perform this centrifugation at a temperature above the cloud point.
- Aqueous Phase Collection: Carefully aspirate the upper, aqueous phase (which should contain your protein) and transfer it to a new, pre-warmed (37°C) low-binding tube. Take care not to disturb the lower, viscous detergent phase (which contains the endotoxins) or the interface.
- Cycle Repetition: For maximum endotoxin removal, repeat steps 2-6 on the collected aqueous phase for 2-3 total cycles. After the final cycle, the aqueous phase is ready for downstream applications or storage.
The Scientist's Toolkit: Essential Research Reagents
| Item | Function in the Experiment |
|---|---|
| Triton X-114 | Non-ionic detergent with a low cloud point (23°C); enables temperature-driven phase separation for partitioning endotoxins away from proteins. [47] [48] |
| Low-Binding Tubes | Plasticware with a special polymer coating that minimizes adsorption of proteins to the tube walls, thereby increasing recovery yield. [49] |
| Solubilizing Fusion Tags (MBP, GFP) | Tags like Maltose-Binding Protein (MBP) can be fused to the target protein to improve its solubility during expression and purification, preventing aggregation and loss. [49] |
| Arginine Hydrochloride | Added to purification and storage buffers; its guanidinium group can disrupt protein-protein interactions, reduce aggregation, and improve the solubility of challenging proteins. [49] |
Safety and Handling Information
Triton X-114 requires careful handling. Consult its Safety Data Sheet (SDS) before use. Key safety notes from the manufacturer include: [47]
- Signal Word: Danger
- Hazard Statements: Harmful if swallowed, causes serious eye damage, causes skin irritation.
- Environmental Hazard: Very toxic to aquatic life with long-lasting effects.
- Personal Protective Equipment (PPE): Wear eyeshields, gloves, and an appropriate respirator filter.
- Flash Point: 251 °C (closed cup).
FAQs: Endotoxin Removal Technologies
Q1: What are the key advantages of membrane chromatography over traditional column chromatography for endotoxin removal?
Membrane chromatography offers several distinct advantages for endotoxin removal in downstream bioprocessing. Unlike traditional resin-based columns where solute transport to binding sites relies on slow diffusion, membrane systems utilize convective flow through pores, significantly reducing mass transfer resistance and allowing for faster processing times [50]. This is particularly advantageous for separating large biomolecules like endotoxin aggregates. Furthermore, membrane adsorbers can handle much higher flow rates at lower back pressures, avoid bed compaction issues, and are easily scalable by increasing membrane surface area, simplifying process development and reducing buffer consumption [50].
Q2: My research requires very high protein recovery. Which endotoxin removal method is least likely to bind my target protein?
For applications demanding high protein recovery, ion exchange chromatography is often the preferred choice. This method capitalizes on the strong negative charge of endotoxins (pI ~2). Under carefully optimized conditions (typically pH >2), endotoxins bind strongly to the positively charged resin, while most therapeutic proteins, which are positively charged, flow through the column without being retained, leading to high recovery rates [9]. Alternatively, affinity chromatography with ligands like polymyxin B offers high specificity for endotoxins, though there is a potential for modest recovery efficiency of the target protein and may require elevated ionic strength for elution [9].
Q3: After using a phase separation method with Triton X-114, I'm concerned about detergent residues. How can this be mitigated?
Residual Triton X-114 in the final protein preparation is a valid concern, as it can interfere with downstream applications. The primary mitigation strategy is to perform multiple rounds of phase separation. After the initial cycle of cold and warm incubation and centrifugation, the upper aqueous phase (containing the protein) is collected and the process is repeated with fresh Triton X-114. This 1-2 additional rounds significantly reduce both endotoxin and detergent carryover [9]. For sensitive applications, a subsequent buffer exchange or dialysis step can further ensure the removal of trace detergent residues.
Q4: The binding capacity of my ion exchange membrane for endotoxins seems low. What factors could be affecting this?
The binding capacity of ion exchange membranes can be influenced by several operational parameters. The pH and salt concentration of your binding buffer are critical; even slight deviations can prevent endotoxins from binding or cause them to elute prematurely [9] [51]. The membrane ligand density itself is a factor, as membranes generally have fewer binding sites compared to traditional resin beads [50]. Finally, the composition of your sample, such as high protein or impurity load, can compete for binding sites and reduce the effective capacity for endotoxins. Optimizing buffer conditions and ensuring your sample is appropriately conditioned (e.g., through dilution or buffer exchange) can help maximize capacity.
Troubleshooting Guides
Table 1: Troubleshooting Membrane Chromatography and Adsorption Methods
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Protein Recovery | Overly stringent binding/wash conditions; non-specific binding to adsorbent. | Reduce ionic strength of wash buffer (e.g., lower NaCl to 250 mM or less) [51]; Use a step-wise imidazole gradient for elution [51]; Add a mild non-ionic detergent (e.g., 0.1% Triton X-100) to binding buffer to minimize non-specific interactions [51]. |
| Incomplete Endotoxin Removal | Insufficient binding capacity; sample overloaded; incorrect buffer pH. | Ensure sample endotoxin load is within membrane/resin capacity; Re-optimize pH to ensure endotoxins are negatively charged; Add a second polishing step with a different mechanism (e.g., follow ion exchange with affinity adsorption) [9]. |
| High Backpressure in Membrane System | Membrane fouling from particulates; clogged pre-filter or membrane pores. | Clarify sample by centrifugation (e.g., 15 min at 10,000 x g) and/or 0.8 µm filtration before loading [51]; Incorporate a pre-filter or guard column; Use radial flow or cross-flow modules that are less prone to fouling [50]. |
| Poor Separation Efficiency | Void volumes from poorly cut tubing or improper fittings; excessive system dispersion. | Inspect and re-cut tubing to ensure a planar surface [52]; Check and tighten all connections to eliminate voids [52]; Reduce extra-column tubing length to minimize band broadening [52]. |
Table 2: Troubleshooting Endotoxin Detection Assays
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Inhibition/Enhancement of LAL Assay | Sample contains interfering substances (e.g., chelators, surfactants, high salt). | Dilute sample to reduce interferent concentration below the inhibition threshold [22]; Use a chromogenic LAL kit resistant to (1,3)-β-D-glucan to avoid false positives [22]; Validate spike recovery for your sample matrix (50-200% recovery is acceptable) [22]. |
| Low Assay Sensitivity | Using an inappropriate standard curve range; detector settings not optimized. | Use the kit's low-range standard curve (e.g., 0.01–0.1 EU/mL) for greater sensitivity [22]; Ensure the detector's data acquisition rate is set to capture at least 10 data points across the peak for accurate quantification [52]. |
| Jagged or Noisy Baseline | Dissolved air in mobile phase; dirty flow cell; insufficient mobile phase mixing; temperature fluctuations. | Degas all buffers and rinse solutions thoroughly [52]; Clean the flow cell according to manufacturer instructions; Ensure mobile phase is being mixed adequately [52]. |
Experimental Protocols for Endotoxin Removal
Protocol 1: Endotoxin Removal by Triton X-114 Phase Separation
Principle: This method uses a non-ionic detergent that undergoes temperature-induced phase separation. At temperatures above 23°C, the solution separates into a detergent-rich phase and an aqueous phase, with endotoxins partitioning into the detergent phase [9].
Procedure [9]:
- Add Triton X-114: Add Triton X-114 to the protein sample to a final concentration of 1% (v/v).
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring to form a homogeneous solution.
- High-Temperature Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes to induce phase separation.
- Centrifugation: Centrifuge at 20,000 × g for 10 minutes at 25°C to fully separate the two phases.
- Collection: Carefully collect the upper aqueous phase (contains the target protein), avoiding the lower detergent phase.
- Repeat: For further endotoxin reduction, subject the collected aqueous phase to 1–2 additional rounds of phase separation.
- Quantification: Measure final endotoxin levels using a Limulus Amebocyte Lysate (LAL) assay.
Protocol 2: Endotoxin Clearance Using Anion Exchange Membrane Chromatography
Principle: Leverages the strong negative charge of endotoxins (pI ~2). At neutral to basic pH, endotoxins bind to the positively charged functional groups on the membrane, while many target proteins flow through [9] [50].
Procedure:
- Membrane Equilibration: Equilibrate the anion exchange membrane (e.g., Q membrane) with 5-10 column volumes (CV) of a low-salt binding buffer (e.g., 20-50 mM Tris-HCl, pH 7.4-8.0).
- Sample Preparation: Adjust the protein sample to the same pH and ionic strength as the binding buffer. This may require dialysis or buffer exchange. For crude samples, clarify by centrifugation and filtration (0.45µm or 0.8µm) [51].
- Sample Loading: Load the prepared sample onto the membrane. The high flow rates achievable with membrane systems can significantly reduce processing time [50].
- Washing: Wash the membrane with 5-10 CV of binding buffer to elute the target protein while endotoxins remain bound.
- Strip and Regenerate: After use, strip any bound endotoxins and other impurities with a high-salt buffer (e.g., 1-2 M NaCl) or NaOH (e.g., 0.1-0.5 M). Re-equilibrate the membrane for storage or future use.
Signaling Pathways and Workflows
Endotoxin Detection LAL Pathway
Membrane Chromatography Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Key Reagents for Endotoxin Removal and Detection
| Item | Function & Application | Key Characteristics |
|---|---|---|
| Triton X-114 | Non-ionic detergent for temperature-driven phase separation of endotoxins from proteins [9]. | Effective for a range of proteins; achieves 45-99% removal; requires careful handling to avoid detergent residues [9]. |
| Anion Exchange Membranes (e.g., Q membrane) | Positively charged membranes for flow-through endotoxin removal based on electrostatic interaction [9] [50]. | High flow rates, rapid processing, scalable; ideal for polishing steps; binding is highly sensitive to pH and salt [9] [50]. |
| Polymyxin B Affinity Resin/Ligand | Affinity chromatography resin/ligand that specifically binds the lipid A moiety of endotoxin [9]. | High specificity and efficiency; concerns about ligand leakage and potential toxicity in some therapeutic applications [9]. |
| Pierge LAL Chromogenic Endotoxin Quantitation Kit | In vitro quantitative measurement of endotoxin via a chromogenic reaction [22]. | Sensitive (0.01-1.0 EU/mL), quantitative, colorimetric readout at 405 nm; resistant to β-glucan interference [22]. |
| Pierce Rapid Gel Clot Endotoxin Assay Kit | Qualitative determination of endotoxin presence via visual clot formation [22]. | Economical, simple, equipment-free; provides a yes/no result at defined sensitivity (e.g., 0.03-0.5 EU/mL) [22]. |
| Endotoxin Removal Resin (e.g., ε-poly-L-lysine based) | High-capacity affinity resin for removing endotoxins from protein solutions [22]. | High binding capacity, uses a non-toxic amino acid polymer; effective in a batch or column format [22]. |
Fundamental Concepts: Endotoxins and the Principle of Dry Heat Depyrogenation
What are endotoxins and why must they be removed?
Endotoxins, also known as lipopolysaccharides (LPS), are toxic components found in the outer membrane of Gram-negative bacteria such as E. coli [4] [9]. When recombinant proteins are produced in these bacterial systems, endotoxin contamination is inevitable [10]. Unlike exotoxins, endotoxins are released upon bacterial death or lysis [4]. The lipid A moiety of LPS is responsible for its potent toxicity, triggering severe immune responses in mammals by over-activating innate immune cells through pattern recognition receptors like TLR4/MD-2 complexes [4]. This can cause fever, inflammation, tissue damage, septic shock, and even death when contaminated products enter the bloodstream [4] [9]. For pharmaceutical products, regulatory standards require endotoxin limits below 5 Endotoxin Units (EU) per kg body weight for items administered parenterally [4]. Even trace amounts can cause false outcomes in research or adverse effects in clinical applications, making effective depyrogenation essential [9] [17].
How does dry heat destroy endotoxins?
Dry heat depyrogenation works through thermal destruction of the endotoxin molecule [53]. The process requires significantly higher temperatures than those needed for sterilization because endotoxins are remarkably stable and resistant to conventional heat treatment [4] [54]. The effectiveness is quantified using the Fh value, which measures heat input in minutes equivalent to the lethality or endotoxin destruction effect delivered by dry heat at a reference temperature of 250°C, with a minimum z-value of 46.5°C [53]. The process must achieve at least a 3-log reduction (99.9% destruction) of bacterial endotoxin to be considered effective [53].
Table 1: Key Technical Parameters for Dry Heat Depyrogenation
| Parameter | Typical Range | Minimum Effective Conditions | Application Context |
|---|---|---|---|
| Temperature for Ovens | 160-190°C (sterilization); ≥200°C (depyrogenation) | 250°C for 30 min [55] [53] | Glassware, metal instruments, heat-stable materials [54] [53] |
| Exposure Time for Ovens | 30-120 minutes | 30 minutes at 250°C [53] | Same as above |
| Temperature for Tunnels | 220-350°C | 325-400°C [55] | Glass containers prior to aseptic filling [53] |
| Exposure Time for Tunnels | Several minutes | A few minutes [55] | Continuous processing of vials and containers [53] |
| Validation Requirement | 3-log reduction of endotoxin | Endotoxin challenge studies [53] | Mandatory for pharmaceutical manufacturing |
Detailed Dry Heat Depyrogenation Protocols
What are the standard operating procedures for dry heat depyrogenation?
Protocol 1: Batch Processing Using a Dry Heat Oven
This method is suitable for laboratory glassware, metal instruments, and other heat-stable materials that can withstand high temperatures [54] [53].
- Step 1: Preparation - Thoroughly clean items to remove any visible residues or particulate matter. Use pyrogen-free water for final rinsing if washing is performed [54].
- Step 2: Loading - Arrange items to allow free circulation of hot air around all surfaces. Avoid overcrowding the chamber [53].
- Step 3: Parameter Setting - Set temperature to a minimum of 250°C with a holding time of at least 30 minutes. Higher temperatures may require shorter exposure times [53].
- Step 4: Process Initiation - Start the cycle only after verifying the temperature setpoint. Monitor the actual temperature throughout the process [53].
- Step 5: Cooling - After the holding time is complete, allow items to cool to room temperature before removal. For critical applications, cool in a controlled environment to prevent recontamination [53].
- Step 6: Storage - Store depyrogenated items in closed, clean containers or packaging to prevent pyrogen recontamination [54].
Protocol 2: Continuous Processing Using a Depyrogenation Tunnel
This automated system is typically used in pharmaceutical manufacturing for glass containers prior to aseptic filling [53].
- Step 1: Tunnel Preparation - Verify that the tunnel's pre-heating, hot, and cooling zones are at their designated setpoints. Ensure HEPA filters are intact and air flow patterns are appropriate for an ISO 5/Grade A environment [53].
- Step 2: Belt Speed Calibration - Set the conveyor belt speed based on validation studies to ensure the required depyrogenation dwell time in the hot zone. The exposure time is a function of tunnel length, temperature, and belt speed [53].
- Step 3: Temperature Verification - Confirm that the hot zone maintains temperatures typically between 220°C and 350°C, with some tunnels operating as high as 400°C [55] [53].
- Step 4: Process Monitoring - Continuously monitor and document the temperature profile and belt speed throughout the operation. The "depyrogenation dwell time" is critical and must be maintained [53].
- Step 5: Cooling Phase - Ensure containers are properly cooled in the cooling zone before entering the aseptic filling area [53].
Figure 1: Dry Heat Depyrogenation Workflow Decision Tree
How do I validate my dry heat depyrogenation process?
Validation is mandatory to prove the process consistently achieves a 3-log reduction of bacterial endotoxin [53]. The lifecycle approach includes three stages:
- Stage 1: Process Design - Define User Requirement Specifications (URS), Critical Quality Attributes (CQAs), and Critical Process Parameters (CPPs). For dry heat depyrogenation, the CPPs are time and temperature [53].
- Stage 2: Process Qualification - Perform Installation Qualification (IQ) and Operational Qualification (OQ) of equipment, followed by Performance Qualification (PQ) of the depyrogenation process [53].
- Stage 3: Continued Process Verification - Implement ongoing monitoring to ensure the process remains in a state of control during routine production [53].
Key Validation Studies:
- Empty Chamber Temperature Distribution - Confirm uniform heat distribution throughout the empty chamber or tunnel using calibrated thermocouples placed in multiple locations [53].
- Loaded Chamber Heat Penetration - Identify "cold spots" and determine worst-case conditions using temperature sensors placed throughout the load, particularly in areas most challenging to heat [53].
- Endotoxin Challenge Studies - Inoculate containers with a known quantity of endotoxin (typically 5,000 EU) and verify at least a 3-log reduction after processing. Use worst-case conditions (increased belt speed, lower temperature setpoint) [53].
Troubleshooting Common Issues
What are the most common depyrogenation failures and their solutions?
Table 2: Troubleshooting Guide for Dry Heat Depyrogenation
| Problem | Potential Causes | Corrective Actions |
|---|---|---|
| Failure to achieve endotoxin reduction | Insufficient temperature or time, incorrect calibration, cold spots in chamber, improper loading [53] | Verify calibration of temperature sensors and belt speed controllers; review validation studies for minimum parameters; improve load configuration for better air circulation [53] |
| Inconsistent results between batches | Variable loading patterns, equipment malfunction, operator error [53] | Standardize loading procedures; implement preventive maintenance; enhance staff training; increase process monitoring [53] |
| Damage to heat-sensitive materials | Excessive temperature or exposure time [55] | Review material specifications; adjust parameters within validated ranges; consider alternative depyrogenation methods for sensitive materials [55] [54] |
| Pyrogen contamination after processing | Improper handling post-depyrogenation, inadequate storage, environmental contamination [54] | Use sterile, depyrogenated forceps for handling; implement aseptic techniques; store items in pyrogen-free containers [54] |
| Failed validation studies | Incorrect sensor placement, inadequate worst-case conditions, recovery method issues [53] | Review study design with quality unit; ensure proper endotoxin spiking and recovery methods; verify sensor calibration pre- and post-study [53] |
How can I prevent endotoxin contamination before depyrogenation becomes necessary?
Prevention is more effective than removal. Implement these practices to minimize initial endotoxin contamination:
- Use pyrogen-free reagents and water (e.g., Lonza LAL grade water or equivalent) [54].
- Wear gloves and change them frequently during procedures. Spray gloves with Cavicide before touching tubes and reagents [54].
- Use sterile, depyrogenated glassware, pipets, and consumables. For reusable items that tolerate high temperatures, bake at 250°C for 2 hours or 200°C overnight [54].
- Conduct procedures in a laminar flow hood when possible [54].
- Avoid cellulose-based filters, which can be a source of beta-glucans that interfere with LAL assays and may be pro-inflammatory [54].
- Be mindful of personal contamination sources - avoid breathing, coughing, or sneezing toward materials, and change gloves immediately after touching non-sterile surfaces [54].
Frequently Asked Questions
Can I use autoclaving for depyrogenation?
No. Standard autoclave cycles (typically 121°C for 15-20 minutes) will sterilize materials but will not effectively destroy endotoxins [54]. The high thermal stability of endotoxins requires the more intense conditions provided by dry heat depyrogenation [4] [54].
What temperature and time combination is minimally effective?
The European Pharmacopeia Chapter 2.6.8 establishes dry heat at a minimum of 250°C for at least 30 minutes for depyrogenation of materials such as glassware [53]. However, time and temperature are inversely related - higher temperatures require shorter exposure times [55] [53].
How do I depyrogenate materials that cannot withstand high temperatures?
For heat-labile materials, several alternatives exist:
- For plastic tubing, stir bars, and other temperature-sensitive tools, flush with Cavicide followed by thorough rinsing with sterile, endotoxin-free water [54].
- Acid or alkali hydrolysis using 0.05N HCl at 100°C for 30 minutes or 0.25N NaOH at 56°C for 1 hour [54].
- Ethylene oxide sterilization, hydrogen peroxide gas-plasma sterilization, or gamma irradiation [54].
- For protein solutions, use affinity chromatography, ultrafiltration, or phase separation methods instead of dry heat [42] [19] [9].
How is dry heat depyrogenation monitored and controlled?
The process requires precise monitoring of time and temperature [53]. Use calibrated thermocouples with an accuracy of ±0.5°C for dry heat sterilizers or ±1.0°C for depyrogenation ovens and tunnels [55] [53]. For depyrogenation tunnels, conveyor belt speed must also be calibrated and monitored as it directly affects exposure time [53]. Modern systems often use wireless data loggers that can withstand the high temperatures and follow the conveyor belt movements [55].
The Scientist's Toolkit
What equipment and reagents are essential for effective dry heat depyrogenation?
Table 3: Essential Research Reagent Solutions for Dry Heat Depyrogenation
| Item | Function/Application | Specifications/Quality Requirements |
|---|---|---|
| Validated Dry Heat Oven or Tunnel | Provides controlled high-temperature environment for endotoxin destruction | Calibrated temperature sensors (±1°C accuracy); timer; uniform heat distribution; for tunnels: calibrated belt speed control [55] [53] |
| Temperature Monitoring System | Validation and routine monitoring of time-temperature parameters | Thermocouples or wireless data loggers with pre- and post-calibration verification; withstand temperatures up to 400°C [55] |
| Endotoxin-Free Water | Cleaning and rinsing of items before depyrogenation | LAL-grade water (e.g., Lonza LAL grade water, ACC Pyroclear certified LAL reagent water) [54] |
| Calibrated Endotoxin Standards | For validation challenge studies | Certified endotoxin standards from E. coli or other Gram-negative bacteria [53] [17] |
| LAL Assay Kit | Quantifying endotoxin levels pre- and post-depyrogenation | Gel-clot, chromogenic, or turbidimetric methods; sensitivity of at least 0.03 EU/mL [42] [4] |
| Pyrogen-Free Containers | Storage of depyrogenated items | Sterile, depyrogenated packaging; sealed containers to prevent recontamination [54] |
| Heat-Resistant Handling Tools | Manipulating items post-depyrogenation | Depyrogenated forceps, tongs; made of materials that can withstand high temperatures [54] |
Where does dry heat depyrogenation fit within a comprehensive endotoxin control strategy?
Dry heat depyrogenation is specifically suited for heat-stable materials like glassware, metal instruments, and glass containers in pharmaceutical manufacturing [54] [53]. It should be implemented as part of a broader endotoxin control strategy that includes:
- Prevention of initial contamination through aseptic techniques and pyrogen-free reagents [54].
- Selection of appropriate endotoxin removal methods based on the material characteristics [54] [9].
- Rigorous environmental monitoring and process controls [53].
- Comprehensive documentation and validation of all critical processes [53].
For recombinant protein research specifically, dry heat ensures that all containers and tools contacting the final product do not introduce endotoxins, complementing other endotoxin removal methods used during protein purification itself [42] [19] [9].
Solving Endotoxin Challenges: Optimization and Troubleshooting for Complex Scenarios
Addressing Low Endotoxin Recovery (LER) Effects in Testing
Frequently Asked Questions (FAQs) on Low Endotoxin Recovery
Q1: What is Low Endotoxin Recovery (LER) and why is it a critical concern? Low Endotoxin Recovery (LER) is a phenomenon describing the loss of detectable endotoxin activity over time in certain sample matrices when measured by standard Limulus Amebocyte Lysate (LAL) assays. It was first formally reported by Chen and Vinther in 2013, though related issues were observed as early as 1998 [56] [57]. LER poses a significant risk to patient safety and product quality because it can lead to false-negative results during routine quality control testing. This means contaminated pharmaceutical products or recombinant proteins could release undetected endotoxins into the human bloodstream, potentially causing life-threatening inflammatory reactions [56] [58].
Q2: What is the mechanistic basis for LER? LER occurs when formulation components, such as chelating agents (e.g., citrate, phosphate buffers) and detergents (e.g., polysorbate, Triton X-100), disrupt the aggregate structure of lipopolysaccharide (LPS), the active molecule in endotoxins [57] [58]. The process is time- and temperature-dependent [56]. Chelators remove essential divalent cations (like Mg²⁺ and Ca²⁺) that stabilize LPS aggregates. Subsequently, detergents intercalate into the weakened aggregates, dispersing them into monomers or smaller micelles [58]. These smaller forms are not efficiently recognized by Factor C, the key enzyme in the LAL cascade, leading to a loss of signal in LAL-based tests [57] [58].
Q3: Is masked endotoxin still biologically active? Yes, evidence confirms that masked endotoxin retains its biological activity. A key study demonstrated that while endotoxin masked in LER conditions (e.g., by citrate and polysorbate) was undetectable in Factor C-based assays (like LAL), it was still potently active in a TLR4-NF-κB reporter gene assay [58]. Furthermore, this masked LPS induced the expression of pro-inflammatory cytokines (e.g., TNF-α, CXCL8) and surface activation markers in primary human monocytes. This demonstrates that the masked endotoxin can still activate immune pathways, emphasizing the potential health risk [58].
Q4: Does LER affect only purified control standard endotoxin (CSE) or also naturally occurring endotoxin (NOE)? Research indicates that LER can affect both purified Control Standard Endotoxin (CSE) and Naturally Occurring Endotoxin (NOE). One study showed that a recombinant protein preparation contaminated with NOE from E. coli triggered an immune response in cells, even though the same sample showed no endotoxin detection in standard LAL and recombinant Factor C assays. This confirms that the masking effect is not an artifact exclusive to purified standards and can occur with natural contamination relevant to manufacturing [58].
Q5: What are some strategies to overcome LER in testing? Mitigating LER requires a multi-faceted approach:
- Use of Alternative Detection Assays: Employ cell-based assays, such as a TLR4-NF-κB reporter gene assay, which can detect masked endotoxin that LAL misses [58].
- Specialized Sample Preparation: Utilize commercial kits designed to "unmask" endotoxin. For example, the ENDO-RS kit has been shown in studies to reliably detect endotoxin under LER conditions [56].
- Novel Testing Platforms: Technologies like ENDOLISA, an ELISA-style assay that uses a bacteriophage-derived protein to capture endotoxin and recombinant Factor C (rFC) for detection, can be more robust against common interferents and achieve higher sensitivity in complex matrices like cell and gene therapy products [59].
- Conduct Hold-Time Studies: Regulatory agencies recommend conducting hold-time studies to assess if, and when, LER occurs in a specific product over time. This is crucial for defining a valid testing window [56].
Troubleshooting Guide: Common Endotoxin Assay Failures
This guide addresses common failures that can occur during endotoxin testing, which are separate from, but sometimes related to, LER.
| Problem | Possible Cause | Solution |
|---|---|---|
| Negative Control Failure | Contamination from non-sterile supplies, glassware, or the environment; poor aseptic technique [60]. | Use certified endotoxin-free consumables, depyrogenate glassware at 250°C for 45 min, and maintain strict sterile technique. Locate assay preparation away from air conditioners and vortexers [26] [60]. |
| Poor Coefficient of Variation (%CV) | Improper pipetting technique; not following manufacturer's vortexing instructions [60]. | Adhere strictly to the assay protocol, ensure proper vortex mixing, and use good pipetting practices [60]. |
| Positive Product Control (PPC) Failure | The product matrix itself interferes with the assay (inhibition or enhancement) [59] [60]. | Adjust the sample pH to 6-8 using endotoxin-free buffers, HCl, or NaOH. For severe interference, consider alternative, more robust methods like ENDOLISA [59] [60]. |
| Low Endotoxin Recovery (LER) | Interaction of endotoxin with chelators and detergents in the formulation, leading to masking [56] [57]. | Perform a hold-time study, use a cell-based assay (e.g., TLR4 reporter), or employ a specialized demasking protocol like the ENDO-RS kit [56] [58]. |
Quantitative Data on Endotoxin Removal and Detection
Endotoxin Removal Efficiency of Different Methods
The following table summarizes data on the effectiveness of various methods for removing endotoxin from protein samples.
| Method / Reagent | Target Substance | Removal Efficiency | Key Findings / Applicability | Citation |
|---|---|---|---|---|
| Triton X-114 Phase Separation | Recombinant Tau Protein | Protocol for removal provided | Effective for removing bound endotoxin from E. coli-derived proteins; requires multiple phase separation cycles and subsequent detergent removal [6]. | |
| Pierce High Capacity Endotoxin Removal Resin | Various Proteins/Antibodies | ≥90% (across proteins of different MW and pI) | Effective for proteins of varying sizes (12-150 kDa) and isoelectric points (pI 4.9-10.6); protein recovery ≥85% at 1 mg/mL [19]. | |
| Pierce High Capacity Endotoxin Removal Resin | Different E. coli Strains | >99% (for 4 strains tested) | Effectively removes endotoxin from 011:B4, 026:B6, 0127:B8, and 0128:B12 strains [19]. |
Endotoxin Detection in Complex Biological Samples
This table shows the performance of an endotoxin removal resin on complex samples.
| Protein / Source | Initial Endotoxin (EU/mL) | Final Endotoxin (EU/mL) |
|---|---|---|
| Anti-fractalkine / Cell Culture Supernatant | 8.26 | <1 |
| His-tagged GFP / E. coli | 9780 | <1 |
| IgG / Human Serum | 78 | <1 |
Source: Adapted from Thermo Fisher application note [19].
Detailed Experimental Protocols
Protocol 1: Removing Bound Endotoxin with Triton X-114
This protocol is detailed for tau protein but can be adapted for other recombinant proteins [6].
Summary of Steps:
- Add Triton X-114 to the protein solution to a final concentration of 2%.
- Incubate at 4°C for 1 hour with rotation.
- Incubate at 37°C for 10 minutes in a water bath (the solution will turn turbid).
- Centrifuge at 20,000 x g for 20 minutes at 37°C. This causes phase separation: the top aqueous layer contains the protein, and the bottom detergent layer contains the endotoxin.
- Carefully collect the top layer without disturbing the bottom layer.
- Repeat steps 1-5 for a total of three phase separation cycles.
- After the third cycle, the detergent is removed from the protein solution using a detergent removal spin column according to the manufacturer's instructions.
Protocol 2: Detecting Biologically Active Endoxin Using a TLR4 Reporter Assay
This protocol is used to validate endotoxin removal and detect masked, biologically active endotoxin that may be missed by LAL [58].
Summary of Steps:
- Cell Seeding and Transfection:
- Seed HEK293 cells (or a similar line) in a cell culture plate.
- Transiently transfect the cells with a plasmid mix containing genes for the human LPS receptor complex (TLR4, MD-2, and CD14) and an NF-κB-luciferase reporter plasmid. A control should be transfected with an empty vector.
- Stimulation:
- After ~24 hours, stimulate the transfected cells with your test protein sample, a known LPS standard (positive control), and an endotoxin-free buffer (negative control).
- Incubation and Detection:
- Incubate the cells for another ~24 hours.
- Lyse the cells and measure the luciferase activity using a luminometer. Activation of the TLR4 pathway by endotoxin will induce NF-κB activity, leading to luciferase expression and a luminescent signal.
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Kit | Function | Application Note |
|---|---|---|
| Triton X-114 | A non-ionic detergent used in phase separation to partition endotoxin away from the protein of interest [6]. | Used in multiple cycles for effective removal of bound endotoxin from recombinant proteins [6]. |
| Pierce High Capacity Endotoxin Removal Resin | An affinity resin composed of cellulose and poly(ε-lysine) that binds endotoxins, allowing them to be separated from protein samples via centrifugation [19]. | Effective for a wide range of protein sizes, charges, and sources; suitable for samples ≥0.25 mg/mL for good recovery [19]. |
| HEK-Blue hTLR4 Cells | A reporter cell line engineered to express the human TLR4/MD-2/CD14 receptor complex. Secretes SEAP upon endotoxin stimulation [6]. | Used to quantify biologically active endotoxin in a cell-based assay, which can detect masked endotoxin [6] [58]. |
| ENDO-RS Kit | A sample preparation kit designed to overcome LER by "demasking" endotoxin, making it detectable again in LAL-style assays [56]. | Critical for validating testing methods for products susceptible to LER, helping to fulfill regulatory requirements [56]. |
| ENDOLISA | A quantitative, fluorescent ELISA-like assay that uses a bacteriophage-derived protein for capture and recombinant Factor C (rFC) for detection [59]. | Highly effective for testing challenging samples like cell and gene therapies, overcoming common interferences [59]. |
Optimizing Buffer Conditions for Maximum Endotoxin Removal Efficiency
Endotoxin contamination presents a significant challenge in recombinant protein research, particularly for proteins expressed in E. coli systems. These lipopolysaccharides (LPS) can trigger severe immune responses in mammalian systems, potentially skewing experimental results and compromising therapeutic applications. This technical support center addresses the critical role of buffer optimization in achieving effective endotoxin removal, providing researchers with practical methodologies to enhance purification efficiency while maintaining protein integrity.
FAQs: Buffer Composition and Endotoxin Removal
How does buffer pH affect endotoxin removal efficiency?
Buffer pH significantly impacts endotoxin removal efficiency by influencing the charge characteristics of both endotoxins and target proteins. Endotoxins carry a strong negative charge (pI~2) across most physiological pH ranges, while proteins exhibit variable charge depending on their isoelectric points.
Key consideration: For anion-exchange chromatography, maintain buffer pH > 2 to ensure endotoxins remain negatively charged and bind effectively to positively charged resins, allowing target proteins to flow through [9]. Optimal pH conditions depend on your specific protein's isoelectric point and stability profile.
What buffer additives effectively enhance endotoxin removal?
Several buffer additives significantly improve endotoxin removal efficiency:
- Detergents: Triton X-114 at 0.1-2% concentration enables temperature-dependent phase separation [6] [9] [61]
- Amino acids: 0.5M arginine facilitates endotoxin stripping through ion-exchange mechanisms [62]
- Salts: Controlled ionic strength modulates electrostatic interactions in chromatographic separations [9]
Critical note: Additive selection must consider compatibility with downstream applications and the need for complete removal post-purification.
Why does my endotoxin removal method yield inconsistent results?
Inconsistent results often stem from variable buffer conditions or inadequate process control:
- Fluctuating temperature during phase separation methods
- Insufficient pre-sanitization of equipment and resins [62]
- Variations in buffer ionic strength affecting binding efficiency
- Incomplete detergent removal after phase separation [6]
Implement stringent process controls and consistent buffer preparation protocols to improve reproducibility.
Troubleshooting Guides
Problem: Low Endotoxin Recovery (LER) in Spiked Samples
Potential Causes:
- Masking of endotoxins by buffer components
- Suboptimal pH or ionic strength
- Detergent interference with detection assays
Solutions:
- Evaluate alternative buffer systems with different compositions
- Incorporate arginine (0.5M) to disrupt protein-endotoxin interactions [62]
- Validate detection methods with appropriate controls
- Implement pre-treatment sanitization with 0.5M NaOH for all equipment [62]
Problem: Significant Protein Loss During Endotoxin Removal
Potential Causes:
- Non-specific binding to chromatographic media
- Protein partitioning into detergent phase during phase separation
- Protein precipitation under optimized buffer conditions
Solutions:
- Modify buffer ionic strength to reduce non-specific binding
- Optimize detergent concentration (test 0.1% vs 2% Triton X-114) [6] [61]
- Incorporate protein-stabilizing additives compatible with your removal method
- Implement controlled, gradual buffer exchange steps
Problem: Incomplete Endotoxin Clearance After Multiple Cycles
Potential Causes:
- Insufficient detergent concentration or contact time
- Suboptimal temperature control during phase separation
- Saturation of binding capacity in chromatographic approaches
Solutions:
- Increase Triton X-114 concentration to 2% and ensure proper incubation times [6]
- Maintain precise temperature control (4°C for binding, 37°C for separation) [6]
- Implement multiple processing cycles (typically 3) for phase separation methods [6]
- Consider orthogonal methods (combining phase separation with chromatography)
Experimental Protocols
Protocol 1: Triton X-114 Phase Separation for Endotoxin Removal
This method exploits the temperature-dependent phase separation of Triton X-114 to partition endotoxins into the detergent-rich phase [6] [9] [61].
Materials:
- Triton X-114 (MP Biomedicals, 193971) [6]
- Protein sample (>0.2 mg/mL recommended) [6]
- Detergent removal spin columns (Thermo Scientific, 87779) [6]
- Thermostatic water bath
Procedure:
- Add Triton X-114 to protein solution to achieve 2% final concentration [6]
- Incubate at 4°C for 1 hour with constant rotation [6]
- Transfer to 37°C water bath for 10 minutes until solution appears turbid [6]
- Centrifuge at 20,000 × g for 20 minutes at 37°C [6]
- Carefully collect upper aqueous phase without disturbing lower detergent phase [6]
- Repeat steps 1-5 for two additional cycles [6]
- Process through detergent removal column according to manufacturer instructions [6]
- Quantify endotoxin levels using LAL or rFC assay [62] [63]
Buffer Optimization Notes:
- Protein concentration >0.2 mg/mL minimizes protein loss during detergent removal [6]
- For sensitive proteins, test reduced Triton X-114 concentrations (as low as 0.1%) [61]
- Maintain precise temperature control throughout phase separation steps
Protocol 2: Arginine-Assisted Endotoxin Stripping from IgG
This method utilizes arginine in an ion-exchange process to dissociate endotoxins from antibodies during protein A purification [62].
Materials:
- L-Arginine (0.5M solution in PBS)
- Protein A resin
- 0.5M NaOH sanitization solution
- AKTA or similar chromatography system
Procedure:
- Sanitize all equipment and protein A resin with 0.5M NaOH [62]
- Load IgG sample onto protein A column
- Wash with PBS to remove unbound contaminants
- Apply 0.5M arginine in PBS to strip endotoxins from bound IgG [62]
- Elute IgG with standard elution buffer
- Validate endotoxin reduction by LAL assay [62]
Buffer Optimization Notes:
- Arginine concentration of 0.5M provides optimal endotoxin stripping without antibody denaturation [62]
- Maintain pH 7.2-7.4 for PBS-based arginine solutions
- Ensure complete removal of NaOH sanitization solution before sample application
Quantitative Data Comparison
Table 1: Comparison of Endotoxin Removal Efficiency Across Buffer Conditions
| Method | Buffer Conditions | Efficiency | Protein Recovery | Key Limitations |
|---|---|---|---|---|
| Triton X-114 Phase Separation [6] [61] | 2% Triton X-114, 3 cycles | >99% reduction [61] | ~80% [61] | Multiple cycles required; detergent removal needed |
| Ion-Exchange Chromatography [9] | pH >2, low ionic strength | High | Medium-High | Sensitive to pH/salt conditions |
| Affinity Chromatography [9] | Specialized ligands, varied ionic strength | High | Medium | Expensive; requires optimized elution |
| Ultrafiltration [9] | Physiological pH, 100 kDa MWCO | 28.9-99.8% | High | Fails to remove small endotoxins |
Table 2: Detergent Concentration Optimization for Phase Separation
| Triton X-114 Concentration | Incubation Conditions | Endotoxin Reduction | Applications |
|---|---|---|---|
| 0.1% [61] | Single wash, 4°C→37°C | ~99% | Ni-NTA purification adjunct |
| 1% [9] | Single cycle, 30min @4°C, 10min @37°C | 45-99% | General protein purification |
| 2% [6] | Three cycles, 1hr @4°C, 10min @37°C | >99% | Critical applications (e.g., neuronal cultures) |
Research Reagent Solutions
Table 3: Essential Materials for Endotoxin Removal Protocols
| Reagent/Equipment | Function | Example Sources |
|---|---|---|
| Triton X-114 | Temperature-dependent phase separation | MP Biomedicals [6] |
| Recombinant Factor C (rFC) | Endotoxin quantification | Multiple commercial suppliers [63] |
| Detergent Removal Columns | Post-processing detergent elimination | Thermo Scientific [6] |
| Protein A Resin | Antibody purification platform | Multiple commercial suppliers [62] |
| L-Arginine | Endotoxin stripping agent | Standard chemical suppliers [62] |
| HEK-Blue hTLR4 Cells | Biological validation of endotoxin removal | InvivoGen [6] |
Experimental Workflow Visualization
Key Takeaways for Researchers
Successful endotoxin removal requires meticulous attention to buffer conditions tailored to your specific protein and purification methodology. The optimal approach often involves method combination and rigorous validation using both biochemical (LAL/rFC) and biological (cell-based) assays. Implementation of pre-emptive sanitization protocols and consistent buffer preparation practices significantly enhances reproducibility across experiments. As regulatory standards evolve toward recombinant testing methods [63], establishing robust, well-documented purification workflows becomes increasingly critical for both basic research and therapeutic development.
Fundamental Concepts: The Interplay of Process Variables and Endotoxins
In the purification of recombinant proteins from gram-negative bacteria like E. coli, endotoxin contamination is a critical concern. Endotoxins, or lipopolysaccharides (LPS), are heat-stable components of the bacterial outer membrane that can elicit severe immune responses (e.g., fever, sepsis) in humans, even at concentrations as low as ≤5.0 EU/kg/h [64]. The physical and chemical conditions of your purification process—specifically pH and conductivity—directly influence both the behavior of your target protein and the removal efficiency of these endotoxins.
Endotoxins possess a strong negative charge due to their phosphate groups in lipid A and core polysaccharide regions, giving them a very low isoelectric point (pI ~2) [9]. Your target protein, depending on its amino acid composition, will have its own distinct pI and charge profile. Manipulating pH and conductivity (a measure of ionic strength) allows you to exploit these differences in charge to separate endotoxins from your protein. Furthermore, these process variables affect protein solubility and aggregation. For instance, uncontrolled pH shifts can drive protein aggregation into Inclusion Bodies (IBs), which can trap endotoxins and complicate downstream purification [65]. A foundational understanding of this interplay is the first step in developing a robust, low-endotoxin process.
Troubleshooting Guides and FAQs
FAQ: How do pH and conductivity specifically affect endotoxin removal?
The charge characteristics of endotoxins and your target protein are the determining factors. At a pH above 2, endotoxins are strongly anionic (negatively charged). Most proteins are also negatively charged at a pH above their pI. However, if you operate at a pH between the pI of your protein and the pI of endotoxins (~2), your protein can be cationic (positively charged) while endotoxins remain anionic. This charge difference is the basis for effective separation using anion-exchange chromatography, where endotoxins bind to the positively charged resin and your protein flows through [9]. Conductivity, or ionic strength, interferes with these electrostatic interactions. High salt concentrations can shield the charges, causing endotoxins to leach from chromatography resins and co-elute with your target protein.
Troubleshooting Guide: Common Scenarios and Solutions
| Problem Description | Potential Root Cause | Recommended Solution |
|---|---|---|
| High endotoxin levels after Ion-Exchange Chromatography (IEC) | Conductivity of the load sample is too high, disrupting electrostatic binding of endotoxins. | Dilute the load sample or use a buffer with lower salt concentration to reduce conductivity prior to loading onto the IEC column [9]. |
| Low protein recovery after Triton X-114 phase separation | Inefficient phase separation due to incorrect temperature or detergent concentration. | Ensure the solution is incubated at 4°C for complete solubilization, followed by a strict 37°C incubation for 10 min to induce clean phase separation before centrifugation [9]. |
| Protein precipitation or aggregation during purification | Drastic or uncontrolled pH shifts during the process. | Implement tighter pH control. Studies show controlled pH at 7.5 reduces non-specific aggregation compared to uncontrolled pH, which can drop to 6.5 and rise to 8.5 [65]. |
| Inconsistent endotoxin quantification results (LAL assay) | Sample pH outside the optimal range (6.0-8.0), inhibiting the enzymatic cascade. | Adjust the pH of a small sample aliquot to 6.0-8.0 using sterile, endotoxin-free NaOH or HCl before performing the assay [66]. |
| Low endotoxin binding to affinity resins in high-salt buffers | Hydrophobic, not electrostatic, interactions are the primary binding mechanism in these conditions. | Consider using specialized resins designed for high-salt environments, such as magnetic nanoparticles functionalized with boronic acid ligands [64]. |
FAQ: My protein is acidic (low pI). How can I remove endotoxins without losing my product?
For acidic proteins that are negatively charged in standard buffers, anion-exchange chromatography is not suitable, as both the protein and endotoxins will bind. In this case, consider the following strategies:
- Use of Detergents: Triton X-114 phase separation is highly effective. Endotoxins partition into the detergent-rich phase, while many proteins remain in the aqueous phase. This method can achieve 45-99% endotoxin removal and is largely independent of the protein's charge [9].
- Explore Multimodal Resins: Innovative materials like magnetic bifunctional nano-agents (MagBER) combine multiple binding mechanisms (e.g., interactions with titanium dioxide and boronic acid ligands) that can function effectively across various solution conditions, including those challenging for standard ion-exchange [64].
Detailed Experimental Protocols
Protocol 1: Endotoxin Removal via Triton X-114 Phase Separation
This is a robust method for separating endotoxins from proteins based on their differential solubility in a non-ionic detergent [9].
Workflow Overview:
Materials & Reagents:
- Purified protein sample
- Triton X-114 detergent
- Ice bath and 37°C water bath or incubator
- Centrifuge
- Pipettes and endotoxin-free tubes
Step-by-Step Method:
- Addition of Detergent: Add Triton X-114 to your protein sample to achieve a final concentration of 1% (v/v). Mix gently.
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring. This ensures complete solubilization and a homogeneous solution.
- High-Temperature Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes. This will induce phase separation into a detergent-rich phase (containing endotoxins) and an aqueous phase.
- Centrifugation: Centrifuge the sample at 20,000 × g for 10 minutes at 25°C to fully separate the two phases.
- Collection: Carefully aspirate the upper aqueous phase, which contains your target protein. Avoid any contamination with the lower detergent phase.
- Repeat (Optional): For further endotoxin reduction, subject the collected aqueous phase to 1–2 additional rounds of phase separation.
- Verification: Measure the endotoxin level in the final protein sample using a Limulus Amebocyte Lysate (LAL) assay [9].
Protocol 2: Endotoxin Quantification via Chromogenic LAL Assay
This protocol provides a quantitative and sensitive measurement of endotoxin concentration in your final sample [22] [67].
Workflow Overview:
Materials & Reagents:
- Pierce Chromogenic Endotoxin Quantitation Kit (or equivalent) [22]
- LAL reagent water (endotoxin-free)
- Microplate reader capable of reading at 405 nm
- Endotoxin-free pipette tips and tubes
- Water bath or incubator (37°C)
Step-by-Step Method:
- Standard Curve Preparation: Reconstitute the Control Standard Endotoxin (CSE) and prepare a dilution series as per kit instructions (e.g., 1.0, 0.1, 0.01, and 0.001 EU/mL) to generate a standard curve [66].
- Sample Preparation: If necessary, dilute your protein sample in LAL reagent water to fall within the assay's linear range (0.01–1.0 EU/mL). Check the pH of the sample and adjust it to 6.0–8.0 using endotoxin-free NaOH or HCl [66].
- Reaction Setup: In a microplate, mix each standard and sample with the LAL reagent. Incubate at 37°C for the recommended time (10-30 minutes, depending on the desired sensitivity).
- Chromogenic Development: Add the chromogenic substrate (Ac-Ile-Glu-Ala-Arg-pNA) to each well and incubate further. The activated clotting enzyme in the LAL will cleave the substrate, releasing yellow p-nitroaniline (pNA).
- Measurement and Analysis: Stop the reaction and measure the absorbance at 405 nm. The intensity of the yellow color is proportional to the endotoxin concentration. Plot the standard curve and calculate the endotoxin concentration in your samples [22].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and materials critical for managing process variables and controlling endotoxins in recombinant protein research.
| Item | Function/Application | Key Considerations |
|---|---|---|
| Triton X-114 | Non-ionic detergent for temperature-induced phase separation of endotoxins [9]. | Effective for a wide range of proteins; requires careful temperature control to avoid protein denaturation. |
| Anion-Exchange Resin | Chromatography media that binds negatively charged endotoxins, allowing positively charged proteins to flow through [9]. | Efficiency is highly dependent on low conductivity and a pH that ensures the target protein is not negatively charged. |
| Pierce Chromogenic LAL Kit | Quantitative endpoint assay for accurate measurement of endotoxin levels [22]. | Provides high sensitivity (0.01 EU/mL); sample pH must be 6.0-8.0 for valid results. |
| Magnetic Boronic Acid Particles | Functionalized nano-agents for endotoxin removal via cis-diol binding mechanism [64]. | Offers a bifunctional binding mechanism; can be effective in complex matrices where traditional methods fail. |
| LAL Reagent Water | Endotoxin-free water for reconstituting standards, diluting samples, and preparing buffers [66]. | Essential for preventing false positives in LAL testing and for preparing clean chromatography buffers. |
| Control Standard Endotoxin (CSE) | E. coli lipopolysaccharide used as a calibrated standard for LAL assays [66]. | Required for generating the standard curve; must be reconstituted and stored according to manufacturer specifications. |
Preventing Cross-Contamination in Multi-Product Facilities
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: What are the most critical factors to consider when validating a cleaning process in a multi-product facility? The most critical factors include establishing scientifically justifiable acceptance criteria for residue limits (e.g., based on Acceptable Daily Exposure or Permitted Daily Exposure), not just relying on "visibly clean" [68] [69]. The validation must demonstrate through documented evidence that the cleaning process consistently and reproducibly reduces residues to an acceptable level [70] [68]. This involves testing the effectiveness against all potential materials, including product residues, cleaning agents, and microbial contaminants [70].
Q2: Our recombinant protein preparations from E. coli have high endotoxin levels. What is the most effective method for removal? Among several common techniques, Triton X-114 phase separation has been identified as particularly effective. One study demonstrated it could achieve a reduction of greater than 99% in endotoxin levels while maintaining protein recovery of over 90% [42]. This method is often more effective than affinity chromatography using immobilized polymyxin B or histidine [42] [9].
Q3: How can facility design itself help prevent cross-contamination? Facility design is a primary defense. Key strategies include:
- Unidirectional Flow: Establishing separate and unidirectional paths for personnel and materials to prevent back-flow of potential contaminants [71].
- Segregation and Airlocks: Using physically segregated areas or operational units separated by airlocks, especially for processes with high-risk materials like viral vectors [71].
- HVAC System Design: Implementing a dedicated air-handling system for each operational unit, with HEPA filters on supply and exhaust air, and maintaining proper air-pressure cascades to contain contaminants [71].
Q4: What role does single-use equipment play in contamination control? Single-use equipment significantly reduces the risk of cross-contamination because components are pre-sterilized and used only once, eliminating the need for cleaning validation between batches [71]. This also minimizes downtime and cleaning activities during product changeover [71].
Q5: What are "dirty hold times" and "clean hold times," and why are they validated?
- Dirty Hold Time: The maximum allowable time between the end of equipment use and the start of the cleaning process. Validating this ensures that dried or hardened residues, which are harder to clean, can still be effectively removed [70] [68].
- Clean Hold Time: The maximum allowable time between the completion of equipment cleaning and its next use. This validation provides assurance that the cleaned equipment does not become recontaminated during storage [70].
Experimental Protocols for Endotoxin Removal
Protocol 1: Endotoxin Removal by Triton X-114 Phase Separation
This is a detailed method for removing endotoxins from recombinant protein preparations [42] [9].
- Principle: The nonionic detergent Triton X-114 forms a homogeneous solution at low temperatures but separates into detergent-rich and aqueous phases upon warming. Endoxins partition into the detergent-rich phase, while many proteins remain in the aqueous phase [9].
- Materials:
- Triton X-114
- Protein sample
- Water baths (4°C and 37°C)
- Centrifuge
- Procedure:
- Addition of Detergent: Add Triton X-114 to the protein sample to achieve a final concentration of 1% (v/v) [9].
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring to ensure a homogeneous solution [9].
- Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes to induce phase separation [9].
- Centrifugation: Centrifuge the sample at 20,000 × g for 10 minutes at approximately 25°C to fully separate the two phases [9].
- Collection: Carefully aspirate the upper aqueous phase, which contains the target protein, avoiding the lower detergent phase [9].
- Repeat (Optional): For further endotoxin reduction, subject the collected aqueous phase to 1–2 additional rounds of phase separation [9].
- Analysis: Measure final endotoxin levels using a Limulus Amebocyte Lysate (LAL) assay [42] [9].
Protocol 2: Endotoxin Removal Using Affinity Resin Spin Columns
This protocol uses a specialized affinity resin for high-capacity, specific endotoxin removal [19].
- Principle: A resin composed of cellulose and poly(ε-lysine) binds endotoxins with high specificity, allowing proteins to be collected in the flow-through [19].
- Materials:
- Pierce High Capacity Endotoxin Removal Spin Columns (0.5 mL)
- Endotoxin-free water and buffers (e.g., phosphate-buffered saline)
- 0.2N NaOH and 2M NaCl solutions
- Laboratory centrifuge
- Procedure:
- Column Preparation: Centrifuge the spin column at 500 × g for 1 minute to remove the storage buffer [19].
- Cleaning & Equilibration:
- Sample Application: Apply 1-2 mL of your protein sample to the column [19].
- Incubation: Incubate at 22°C with gentle end-over-end mixing for 1 hour [19].
- Elution: Centrifuge the column at 500 × g for 1 minute to collect the purified sample [19].
- Analysis: Measure endotoxin levels via an LAL assay and determine protein recovery using a protein assay (e.g., BCA assay) [19].
Comparison of Endotoxin Removal Methods
The table below summarizes the key characteristics of common endotoxin removal techniques to help select the appropriate method [9].
Table 1: Comparison of Endotoxin Removal Methods
| Method | Efficiency | Specificity | Cost | Key Limitations |
|---|---|---|---|---|
| Triton X-114 Phase Separation | Moderate to High (45-99%) [9] | Low [9] | Low [9] | Potential for trace detergent residues; may require multiple cycles [9]. |
| Affinity Chromatography | High (>90%) [19] | High [9] | High [9] | Expensive resins; may require optimization of ionic strength for elution [9]. |
| Ion Exchange Chromatography | High [9] | Medium [9] | Medium [9] | Sensitive to pH and salt conditions; relies on charge differences [9]. |
| Ultrafiltration | Moderate (28.9-99.8%) [9] | Low [9] | Low [9] | Ineffective for separating endotoxins from large proteins [9]. |
| Activated Carbon Adsorption | High (e.g., 93.5%) [9] | Medium [9] | Medium [9] | Non-selective; can bind target proteins, leading to product loss [9]. |
Performance Data of Affinity Resin for Various Proteins
The following table provides experimental data demonstrating the effectiveness of an affinity resin across proteins with different properties [19].
Table 2: Endotoxin Removal from Various Proteins Using Affinity Resin
| Protein | Molecular Weight (Da) | Isoelectric Point (pI) | Initial Endotoxins (EU/mL) | Final Endotoxins (EU/mL) | Removal (%) |
|---|---|---|---|---|---|
| Cytochrome C | 12,000 | 10.6 | 10,000 | 1.35 | >99 |
| Myoglobin | 17,000 | 6.8 | 10,000 | 3.67 | >99 |
| BSA | 66,000 | 4.9 | 10,000 | 0.80 | >99 |
| BGG | 150,000 | 7.4 | 10,000 | 4.60 | >99 |
Workflow Visualization
Endotoxin Removal Decision Pathway
Multiproduct Facility Contamination Control Strategy
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagents for Endotoxin Control
| Item | Function/Application |
|---|---|
| Triton X-114 | A nonionic detergent used for temperature-dependent phase separation to remove endotoxins from protein solutions [42] [9]. |
| Polymyxin B Affinity Resin | An affinity chromatography ligand that specifically binds the lipid A portion of endotoxins, enabling high-specificity removal [42] [9]. |
| Limulus Amebocyte Lysate (LAL) | A critical assay derived from horseshoe crab blood used to detect and quantify endotoxin levels in samples [42] [9]. |
| High-Capacity Endotoxin Removal Resin | A ready-to-use resin, often based on cellulose and poly(ε-lysine), for efficient endotoxin removal from various sample types via spin columns or chromatography [19]. |
| Endotoxin-Free Water & Buffers | Essential solvents and solutions certified to have ultra-low endotoxin levels to prevent introduction of contaminants during experiments or processing [19]. |
Strategies for Difficult-to-Clean Molecules and Sensitive Proteins
This technical support resource addresses a critical challenge in biopharmaceutical development: managing endotoxin contamination in recombinant protein research. Endotoxins, or lipopolysaccharides (LPS) from Gram-negative bacterial cell walls, can trigger potent immune responses in mammals, compromising preclinical research data and product safety [72] [4]. Effective contamination control requires integrated strategies spanning equipment cleaning validation, sensitive detection methods, and specialized purification techniques for sensitive proteins.
Frequently Asked Questions (FAQs)
Q1: Why is endotoxin contamination particularly problematic for recombinant proteins?
Endotoxin contamination is especially challenging for recombinant proteins, particularly those expressed in E. coli, because the proteins are produced in a system where the cell wall contains substantial amounts of LPS [4] [73]. During purification, these endotoxins can co-purify with the target protein. Even nanogram quantities can adversely affect biochemical assays and cell-based systems, while in vivo administration can cause pyrogenic responses, inflammation, and septic shock in mammals [4] [73]. This necessitates rigorous removal and prevention strategies to ensure both experimental accuracy and product safety.
Q2: What are the regulatory expectations for equipment cleaning in bioprocessing?
The FDA requires validated cleaning procedures to prevent cross-contamination and drug adulteration [68]. Key expectations include:
- Written Procedures: Detailed Standard Operating Procedures (SOPs) for cleaning equipment under different scenarios [68] [74].
- Validation Protocols: Documented evidence that cleaning processes consistently reduce residues to an acceptable level [68].
- Acceptance Criteria: Established limits for residue carryover, typically including a visual inspection (no visible residue), chemical criteria (e.g., no more than 10 ppm of a product in another), and microbial criteria [74].
Q3: What methods are effective for removing endotoxins from protein solutions?
Several chromatographic and separation techniques can effectively remove endotoxin contaminants, though selection depends on the properties of your target protein [4] [73].
Table: Endotoxin Removal Methods for Protein Preparations
| Method | Mechanism | Reported Efficacy | Considerations |
|---|---|---|---|
| Triton X-114 Phase Separation | Exploits the preferential partitioning of endotoxins into a detergent-rich phase [73]. | Up to 99% reduction after three cycles [73]. | Must ensure detergent removal and that it doesn't denature the target protein. |
| Affinity Chromatography | Uses ligands (e.g., polymyxin B, histidine) that bind specifically to the Lipid A moiety of LPS [4] [73]. | Effective reduction, though dependent on conditions [73]. | Polymyxin B can leak; histidine affinity may require deoxycholate pretreatment [73]. |
| Ion-Exchange Chromatography | Binds either the target protein or the endotoxin based on charge interactions [4]. | Effective for many proteins [4]. | Less specific; success depends on the relative charge of the protein and LPS under selected conditions [73]. |
Q4: When is cleaning validation required for dedicated equipment?
Cleaning validation is required for any equipment used in the production, processing, packing, or holding of drug products, even if the equipment is dedicated to a single product [68] [74]. This is particularly important for difficult-to-clean equipment like fluid bed dryer bags. The FDA enforces that equipment must be cleaned at appropriate intervals to prevent contamination that could alter the drug product's safety, identity, strength, quality, or purity [68] [74].
Troubleshooting Guides
Problem: Persistent Endotoxin Contamination in Recombinant Protein Preparation
Possible Causes and Solutions:
Ineffective Removal Technique for Your Protein
- Cause: The chosen endotoxin removal method may be incompatible with your protein's properties (e.g., hydrophobicity, isoelectric point).
- Solution: Evaluate alternative methods. If affinity chromatography was ineffective, consider Triton X-114 phase separation. The protocol involves adding the detergent to the protein solution, incubating on ice, and then warming the solution to induce phase separation. The protein remains in the detergent-poor aqueous phase, while endotoxins partition into the detergent-rich phase, which can be removed by pipetting [73]. Multiple cycles (e.g., three) can enhance efficacy [73].
Re-introduction of Endotoxins from Buffers or Equipment
- Cause: Using non-sterile, pyrogen-free water and buffers, or equipment that has not been properly cleaned and depyrogenated.
- Solution: Implement strict process controls. Use only Limulus Amoebocyte Lysate (LAL) reagent water or other endotoxin-free water for all buffer preparations [73]. Ensure all glassware, plasticware, and equipment are thoroughly cleaned and depyrogenated, ideally using validated processes that include heating at high temperatures (e.g., 250°C for 45 minutes) to destroy endotoxins [4].
Problem: Inadequate Cleaning of Manufacturing Equipment
Possible Causes and Solutions:
Poorly Designed or Validated Cleaning Process
- Cause: The cleaning procedure does not effectively remove all soil residues, including the target product, intermediates, byproducts, and cleaning agents.
- Solution: Develop and validate a robust cleaning procedure. This includes defining and documenting the rationale for residue limits, which should be logical, practical, achievable, and verifiable [68]. The sensitivity of the analytical methods used for detection must be considered when setting these limits [68].
Inadequate Training and Documentation
- Cause: Complex cleaning procedures, especially for systems with semi-automatic or automatic Clean-in-Place (CIP) systems and intricate parts like ball valves, require well-trained operators.
- Solution: Ensure operators have specific training and knowledge of the systems they are cleaning. Procedures should be highly detailed and documented, especially for critical cleaning steps. Piping and valves should be clearly tagged and identifiable both on diagrams and physically [68].
Experimental Protocols
Detailed Protocol: Triton X-114 Phase Separation for Endotoxin Removal
This protocol is adapted from methods found to effectively remove endotoxins from recombinant protein preparations [73].
Principle: Non-ionic detergents like Triton X-114 form a cloudy solution when cooled but separate into detergent-rich and detergent-poor aqueous phases upon warming. Endotoxins, due to their high hydrophobicity, preferentially partition into the detergent-rich phase, while many proteins remain in the aqueous phase.
Materials:
- Triton X-114
- Protein solution containing endotoxins
- Ice bath
- 37°C water bath or incubator
- Microcentrifuge tubes
- LAL assay kit for endotoxin quantification
Procedure:
- Pre-condensation of Triton X-114: To reduce UV absorbance, pre-condense Triton X-114 by warming the solution to 37°C and discarding the lower, detergent-rich phase. Repeat this process three times [73].
- Add Detergent: Add a pre-determined, optimal concentration of Triton X-114 to your protein solution. The final concentration typically ranges from 1-4% (v/v) [73].
- Incubate on Ice: Incubate the mixture on ice for 15 minutes to allow the solution to become clear.
- Induce Phase Separation: Transfer the tube to a 37°C water bath for 10 minutes. The solution will become cloudy as the two phases separate.
- Centrifuge: Centrifuge the tube at approximately 13,000 × g for 10 minutes at room temperature to complete phase separation. This will yield a small, dense, detergent-rich phase at the bottom of the tube and a large, upper, detergent-poor aqueous phase.
- Recover Protein: Carefully pipette the upper aqueous phase (containing your protein) into a fresh tube.
- Repeat Cycles: To maximize endotoxin removal, repeat steps 2-6 for two additional cycles (three cycles total). The optimal number of cycles should be determined experimentally for your specific protein [73].
- Verify Efficacy: Use an LAL assay (gel-clot, chromogenic, or turbidimetric) to quantify endotoxin levels before and after the procedure to confirm reduction [4] [73].
Notes: The compatibility of this method with your specific protein must be validated. Some proteins may denature in the presence of detergent or may also partition into the detergent phase.
Workflow: Integrated Strategy for Endotoxin Control
The following diagram illustrates a logical workflow for controlling endotoxin contamination, combining prevention, removal, and verification.
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for Endotoxin Management
| Item | Function / Description | Key Consideration |
|---|---|---|
| LAL Assay Kits | Standardized method for detecting and quantifying endotoxin levels in solutions [4]. | Available in gel-clot, turbidimetric, and chromogenic formats; choose based on required sensitivity and throughput [4]. |
| Polymyxin B Sepharose | Affinity chromatography resin that binds the Lipid A portion of endotoxin [73]. | Potential for ligand leakage must be monitored, as it could contaminate the protein preparation [73]. |
| Triton X-114 | Non-ionic detergent used for phase separation to partition endotoxins away from proteins [73]. | Must be pre-condensed to reduce UV absorbance. Compatibility with the target protein's stability is critical [73]. |
| Endotoxin-Removing Membranes | Specialized filters designed to adsorb endotoxins during filtration steps [72]. | Often used in chromatographic separations or as part of a multi-step purification strategy [72]. |
| LAL Reagent Water (LRW) | Sterile, endotoxin-free water specifically for use in LAL tests and preparing solutions [73]. | Essential for preventing false positives in detection assays and for making buffers for sensitive proteins [73]. |
Method Validation and Technology Comparison: Ensuring Efficacy and Compliance
Endotoxins, or lipopolysaccharides (LPS), are complex glycolipids found in the outer membrane of Gram-negative bacteria like E. coli [7]. During recombinant protein production in bacterial systems, these endotoxins are common contaminants that can co-purify with the target protein [27]. Even picogram quantities of endotoxin can activate immune cells, particularly CD1c+ dendritic cells, potentially skewing experimental results and compromising drug safety [17] [27]. Effective detection and quantification are therefore critical, with the Limulus Amebocyte Lysate (LAL) assay being the most widely used method [75] [7]. This technical support center provides troubleshooting guidance for the primary LAL-based techniques—Gel Clot, Turbidimetric, and Chromogenic assays—within the broader context of ensuring the purity and safety of recombinant protein research and therapeutics.
Comparison of Key Endotoxin Detection Methods
The following table summarizes the core principles, outputs, and key applications of the four main endotoxin detection methods.
Table 1: Core Endotoxin Detection Methods
| Method | Principle | Detection Output | Key Applications |
|---|---|---|---|
| Gel Clot LAL [76] [7] | Visual clot formation from endotoxin-activated lysate | Qualitative (Positive/Negative) or semi-quantitative with dilution series | Pharmacopeial referee test; simple, cost-effective quality control [76] |
| Turbidimetric LAL [77] [7] | Measures turbidity increase from clot formation | Quantitative (Absorbance) | Research and quality control requiring precise quantification |
| Chromogenic LAL [7] | Measures color change from a cleaved synthetic peptide-chromogen complex | Quantitative (Absorbance) | High-sensitivity detection in complex samples |
| Fluorescent LAL [7] | Measures fluorescence from a cleaved synthetic peptide-fluorophore complex | Quantitative (Fluorescence) | Ultra-sensitive detection (e.g., 0.01-10 EU/mL) [7] |
Troubleshooting Common Assay Issues
False Positive and Negative Results
Q: My gel clot assay shows firm gels in samples expected to be negative. What could be causing these false positives?
- A: False positives can arise from several sources:
- Environmental Contamination: Disposable labware and consumables can be a significant source of endotoxin contamination. Always use labware certified as endotoxin-free or "apyrogenic," and ensure the specific endotoxin limit is suitable for your assay's sensitivity [75] [78].
- Interfering Substances: Fungal (1→3)-β-D-glucans can also induce clotting in the LAL assay. Use LAL reagents formulated with high levels of a glucan blocker to minimize this interference [75].
- Contaminated Reagents: Ensure all water, buffers, and salts are certified endotoxin-free. Operate in a clean environment, such as a laminar flow hood, and use aseptic technique to avoid direct hand contact with critical items [78].
Q: I am getting negative results in my chromogenic assay when I know the sample contains endotoxin. What are the common causes of false negatives?
- A: False negatives are often due to matrix interference:
- Inhibitory Substances: High protein concentrations (>1% w/v), extreme pH (<4.0 or >9.0), chelators (e.g., EDTA >0.1 M), and organic solvents can inhibit the LAL enzyme reaction [78].
- Solution: Perform a spike recovery test. Dilute the sample to reduce the concentration of interferents, using the Maximum Valid Dilution (MVD) as a guide. Alternatively, adjust the sample pH to 6.5-7.5 or add cations (e.g., 0.05M Ca²⁺) to counteract chelators [78].
Technical and Procedural Errors
Q: The standard curve in my turbidimetric assay is unstable. How can I improve its reliability?
- A: Unstable readings in turbidimetric methods can be addressed by:
- Ensuring Sample Quality: Use fresh samples and control reaction times. Particulate matter, precipitation, or settling in highly turbid solutions can cause erratic readings [77].
- Eliminating Air Bubbles: Even tiny air bubbles in the cuvette can scatter light and lead to unstable measurements. Check the sample for bubbles before reading [77].
- Verifying Instrumentation: Ensure the spectrophotometer's temperature control is precise (37.0 ± 0.1°C) and that the optical system is properly calibrated [78].
Q: My dilution series for the standard curve seems inaccurate. What is the best practice for preparing it?
- A: Errors in the dilution series are a common pitfall that can lead to considerable errors in final results [75].
- Consistency: Keep the starting concentration and dilution type consistent between multiple routine tests [75].
- Technique: To ensure accuracy, the American Pharmaceutical Review recommends that the dilution series should be quantified three times each by three separate technicians prior to the release of a lysate lot for routine use [75].
- Materials: Use pyrogen-free pipette tips, tubes, and water for all dilutions. Vortex lyophilized endotoxin standards vigorously, as endotoxin can adhere to vial surfaces [7] [78].
Essential Reagents and Materials
Using the correct reagents is fundamental to obtaining accurate and reproducible endotoxin testing results.
Table 2: Research Reagent Solutions for Endotoxin Testing
| Item | Function | Key Considerations |
|---|---|---|
| LAL/TAL Reagent [76] [7] | Core enzyme for endotoxin detection | Choose sensitivity (e.g., 0.03 EU/mL) and format (gel-clot, chromogenic, etc.) appropriate for your application. |
| Endotoxin Standard [7] [78] | Calibration and standard curve generation | Use certified, standardized Control Standard Endotoxin (CSE). Vortex vigorously after reconstitution. |
| Endotoxin-Free Water [75] [78] | Sample/reagent dilution, reconstitution | Must be pyrogen-free. The default solvent for all assay preparations. |
| LAL Reagent Water [78] | Specific water for dilution | Validated for use in LAL assays to avoid interference. |
| Pyrogen-Free Labware [75] | Tubes, tips, and plates | Certified to have endotoxin levels below the detection limit of your assay (e.g., <0.005 EU/product). |
| Extracting Solution [75] | Extracting endotoxins from devices | Using water can allow interfering substances to affect the reaction. Use a specialized solution for complex samples. |
Experimental Workflow and Troubleshooting Logic
The following diagram illustrates the standard workflow for performing a quantitative LAL assay (Turbidimetric/Chromogenic) and the key decision points for troubleshooting.
Advanced Troubleshooting: Resolving Complex Issues
Q: My sample continues to interfere with the LAL reaction despite dilution. How can I handle difficult matrices?
- A: For challenging samples like serum, antibodies, or formulations with high salt or chelators:
- Employ Additional Treatments: Beyond dilution, centrifugation (10,000 × g for 15 min) or filtration through 0.22 μm low-binding PVDF filters can remove interfering particulates or proteins [78].
- Validate the Method Rigorously: Conduct a full interference test as per pharmacopeial guidelines (e.g., USP <85>) using three separate sample batches spiked with known endotoxin concentrations. Ensure recovery is within 50-200% (with 75-150% being a more rigorous target for sensitive work) [7] [78].
- Consider the Assay Format: If matrix interference is insurmountable in one format, switching to a different type of LAL assay (e.g., from chromogenic to turbidimetric) or using a recombinant Factor C assay, which is not derived from horseshoe crab blood, may provide a solution [7].
Q: How do I validate that my endotoxin testing process is compliant with regulatory standards?
- A: Key steps for validation and compliance include:
- Reagent Qualification: Revalidate the sensitivity of the LAL reagent with each new lot you receive [78].
- System Suitability: The standard curve must have a correlation coefficient (r) of |r| ≥ 0.980 [7].
- Sample Suitability (Spike Recovery): As mentioned above, the sample must not interfere with the assay, confirmed by spike recovery tests [78].
- Environmental Controls: Regularly decontaminate work surfaces and equipment. Use dry heat (e.g., 250°C for 30 minutes) to depyrogenate glassware and other heat-stable items [78].
Within the broader thesis on methods to reduce endotoxin contamination in recombinant proteins research, this technical support center addresses the critical challenge of endotoxin removal. Endotoxins, or lipopolysaccharides (LPS), from the outer membrane of Gram-negative bacteria, can trigger severe immune responses in humans and interfere with in vitro research processes, compromising both patient safety and experimental validity [9] [7]. This guide provides a comparative analysis of standard removal techniques and troubleshooting support to help researchers, scientists, and drug development professionals select and optimize the most appropriate method for their specific application.
The following table summarizes the core characteristics of the primary endotoxin removal techniques to facilitate an initial comparison.
Table 1: Comparison of Key Endotoxin Removal Methods
| Technology | Efficiency | Specificity | Cost | Key Limitations |
|---|---|---|---|---|
| Ultrafiltration [9] | Moderate (28.9% - 99.8%) | Low | Low | Ineffective for small endotoxins or proteins of similar size; efficiency depends on solution conditions. |
| Adsorption [9] | High | Medium | Medium | Non-specific binding can lead to significant product loss; may require additional steps to remove residual carbon. |
| Phase Separation [9] | Moderate (45% - 99%) | Low | Low | Potential for trace detergent residues; repeated heating/cooling cycles may degrade sensitive biomolecules. |
| Affinity Chromatography [9] | High | High | High | High upfront cost; can have modest recovery efficiency and may require elevated ionic strength for elution. |
| Ion Exchange Chromatography [9] | High | Medium | Medium | Performance is highly sensitive to the pH and salt conditions of the solution. |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My endotoxin levels are still too high after using an ultrafiltration unit. What could be going wrong?
A: Several factors can lead to suboptimal performance in ultrafiltration [9]:
- Protein and Endotoxin Aggregation: The efficiency of ultrafiltration relies on the formation of large endotoxin aggregates (>100 kDa). If your solution conditions prevent aggregation, smaller endotoxin monomers may pass through the membrane. Check your buffer composition, pH, and protein concentration.
- Molecular Interactions: If your target protein binds to endotoxins, it can carry the endotoxins through the membrane. Disrupting these interactions may require optimizing the buffer ionic strength or using detergents.
- Inappropriate Cut-off: Ensure your molecular weight cut-off (MWCO) membrane is appropriate. A 100 kDa MWCO is often used, but verify that your target protein is significantly smaller than the endotoxin aggregates.
Q2: I'm experiencing significant loss of my target protein during activated carbon adsorption. How can I minimize this?
A: Protein loss with activated carbon is common due to its non-specific nature [9]. Consider these steps:
- Optimize Conditions: Perform the adsorption at a slightly acidic pH, which is generally optimal. Also, test different contact times and concentrations of activated carbon (e.g., 1% w/v) to find a balance between endotoxin removal and product loss.
- Explore Alternative Adsorbents: Switch to a more specific adsorption method. Immobilized Polymyxin B affinity chromatography is a high-specificity alternative that uses electrostatic interactions to bind endotoxins while allowing most proteins to flow through, thereby preserving your target molecule [9].
Q3: After phase separation with Triton X-114, my target protein is inactive. What might have caused this?
A: Protein inactivation in phase separation is often linked to the detergent or the process itself [9]:
- Detergent Effects: Non-ionic detergents like Triton X-114 can denature some sensitive proteins. Ensure your protein is compatible with these detergents.
- Temperature Stress: The method requires a heating step (to 37°C) to induce phase separation. This elevated temperature, even if mild, could be denaturing your specific protein.
- Residual Detergent: Trace amounts of Triton X-114 in your final aqueous phase could interfere with downstream assays or protein function. Ensure careful pipetting to avoid the detergent phase and consider methods to remove residual detergent.
Q4: My sample consistently shows assay interference in the LAL test, making results unreliable. How can I overcome this?
A: Assay interference is a common challenge in bacterial endotoxin testing (BET) [7].
- Perform a Spike Recovery Test: This is critical for validation. Spike a known amount of endotoxin into your sample and run the LAL test. The recovery should be between 50-200% (with 75-150% being a more rigorous target). If recovery is outside this range, your sample matrix is interfering with the assay [7].
- Optimize Sample Dilution: Dilute your sample to overcome interference, but ensure you do not exceed the Maximum Valid Dilution (MVD). The MVD is calculated based on the endotoxin limit for your product and is the maximum dilution at which you can still detect the limit [13].
- Use Appropriate Controls: Always use certified endotoxin standards to generate a standard curve and include a positive product control (PPC) with a known endotoxin spike to validate each test run [7].
Detailed Experimental Protocol: Triton X-114 Phase Separation
The following is a detailed protocol for endotoxin removal using Triton X-114, based on a study which found it more effective for certain recombinant proteins than immobilized polymyxin B or histidine affinity chromatography [9].
Aim: To remove endotoxins from a recombinant protein sample using temperature-induced phase separation.
Principle: The non-ionic detergent Triton X-114 forms a homogeneous solution at low temperatures (4°C) but undergoes phase separation at elevated temperatures (37°C), partitioning hydrophobic endotoxins into the detergent-rich phase while leaving the target protein in the aqueous phase [9].
Materials:
- Recombinant protein sample
- Triton X-114 detergent
- Ice bath and 37°C water bath
- Centrifuge
- LAL assay kit for endotoxin quantification
Procedure:
- Addition of Detergent: Add Triton X-114 to the protein sample to achieve a final concentration of 1% (v/v).
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring to ensure complete solubilization and a homogeneous solution.
- High-Temperature Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes to induce phase separation. The solution will become cloudy as two distinct phases form.
- Centrifugation: Centrifuge the sample at 20,000 × g for 10 minutes at 25°C to fully separate the two phases (a dense detergent-rich phase and a light aqueous phase).
- Collection of Aqueous Phase: Carefully aspirate and collect the upper aqueous phase, which contains the target protein. Take extreme care to avoid contaminating the pipette tip with the lower detergent phase.
- Repeat Phase Separation (Optional): To further reduce endotoxin levels, subject the collected aqueous phase to 1–2 additional rounds of Triton X-114 phase separation (repeat steps 1–5).
- Endotoxin Quantification: Measure endotoxin levels in the final aqueous phase using a validated Limulus Amebocyte Lysate (LAL) assay [9] [7].
Experimental Workflow and Method Selection
The following diagrams illustrate a general endotoxin removal workflow and a logical path for selecting the appropriate method.
Endotoxin Removal Workflow
Method Selection Logic
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Endotoxin Removal and Detection
| Item | Function/Brief Explanation |
|---|---|
| Triton X-114 | A non-ionic detergent used in temperature-induced phase separation to partition endotoxins into a detergent-rich phase [9]. |
| Polymyxin B Agarose | An affinity chromatography resin with an immobilized antibiotic that specifically binds the lipid A component of endotoxins [9]. |
| Anion-Exchange Resins | Chromatography media (e.g., Q Sepharose) that bind negatively charged endotoxins at neutral pH, allowing positively charged proteins to pass through [9]. |
| Ultrafiltration Membranes | Membranes with a specific molecular weight cut-off (e.g., 100 kDa) used to separate large endotoxin aggregates from smaller proteins via size exclusion [9]. |
| Limulus Amebocyte Lysate (LAL) | A reagent derived from horseshoe crab blood, essential for gel-clot, chromogenic, or turbidimetric assays to detect and quantify endotoxins [7]. |
| Control Standard Endotoxins (CSE) | Certified endotoxin standards of known concentration used to generate calibration curves and validate each LAL test run [7]. |
What Are Patient-Centric Acceptance Criteria?
A Patient-Centric Quality Standard (PCQS) is a set of patient-relevant attributes and their associated acceptance ranges to which a drug product should conform within the expected patient exposure range. For endotoxins, this means establishing limits that ensure patient safety based on actual product use rather than relying solely on compendial general requirements. This approach understands that not all quality attributes impact the patient equally, and those with potential safety implications must be evaluated within the potential exposure range [79].
The Critical Role of Endotoxin Testing
Endotoxins, or lipopolysaccharides (LPS), are structural glycolipids found in the cell membranes of Gram-negative bacteria like E. coli. They consist of a core oligosaccharide chain, O-specific polysaccharide side chain (O-antigen), and a toxic lipid component (lipid A). When introduced into mammalian systems, endotoxins can trigger powerful immune responses including fever, inflammation, shock, and sepsis [7]. In research settings, even low-level endotoxin contamination can distort cell membranes, affect gene expression and protein production, and activate immune cells, potentially compromising experimental results [27].
Establishing Patient-Centric Endotoxin Limits
Compendial Foundations and Calculations
The fundamental compendial endotoxin limit for parenteral products is based on a threshold pyrogenic dose of 5.0 Endotoxin Units (EU) per kilogram of patient body weight per hour (5.0 EU/kg/h) [80]. This threshold is derived from historical studies comparing pyrogenicity of endotoxins purified from Escherichia coli in humans and rabbits. The acceptance criterion for a specific product is calculated as K/M, where:
- K = threshold pyrogenic dose of endotoxin per kilogram of body weight (5 EU/kg for parenteral drugs)
- M = maximum recommended bolus dose of product (per hour) per kilogram of body weight [80]
The Body Weight Debate: Average vs. Lowest Weight
Recent regulatory discussions have focused on whether to use average body weight or lowest patient body weight when calculating endotoxin acceptance criteria for flat-dose products:
| Approach | Rationale | Considerations |
|---|---|---|
| Average Body Weight (70 kg US, 60 kg Japan) | Compliant with compendial requirements; significant safety margin already exists due to LAL test sensitivity [80] | Supported by lack of clinical evidence for endotoxin-related safety risks; considers actual patient population |
| Lowest Body Weight (as requested by some regulators) | Provides additional safety margin for most vulnerable patients | May create overly tight criteria that risk batch rejection without safety benefit; may impact product supply |
The enhanced patient-centric approach calculates criteria according to pharmacopeial methods while considering contributions from primary packaging, devices, consumables, and administration diluents. The resulting criteria are sufficient to ensure patient safety without further tightening based on batch data or lowest patient weight [80].
Safety Margins in Current Practice
Multiple factors provide substantial safety margins in current endotoxin testing practices:
- LAL Test Sensitivity: The Limulus Amebocyte Lysate (LAL) method is significantly more sensitive than the rabbit pyrogen test (RPT) used in establishing the threshold dose [80]
- Environmental vs. Purified Endotoxins: The threshold pyrogen dose of 5 EU/kg/h was developed using purified Gram-negative LPS from E. coli that are more potent per unit mass than environmental endotoxins found in pharmaceutical products [80]
- Historical Evidence: Analysis of FDA CGMP observations (2011-2021) found only one of 188 endotoxin-related observations involved inappropriate product-acceptance criteria, and endotoxin-related adverse events represent an extremely small proportion of all reported cases [80]
Technical Guide: Endotoxin Testing Methods
Comparison of Bacterial Endotoxin Testing (BET) Methods
| Method | Principle | Sensitivity | Regulatory Status | Best Use Cases |
|---|---|---|---|---|
| Gel-Clot LAL | Qualitative clot formation in presence of endotoxins | Economical, specific, and sensitive | USP <85>, EP 2.6.14, JP <4.01> | Routine testing where quantitative results not essential |
| Chromogenic LAL | Colorimetric measurement of enzyme reaction | Varies by assay; quantitative | USP <85>, EP 2.6.14, JP <4.01> | When precise quantification required |
| Turbidimetric LAL | Turbidity measurement of reaction mixture | Varies by assay; quantitative | USP <85>, EP 2.6.14, JP <4.01> | Kinetic studies and high-throughput testing |
| Fluorescent assays (Qubit, Quant-iT) | Fluorescence-based detection | 0.01-10.0 EU/mL | Can be validated to comply with Pharmacopeia standards | Sensitive detection for in vivo studies and low-limit products |
| Recombinant assays | Recombinant protein substitute for LAL | Varies; may have reduced dynamic range | Requires additional validation as alternative method | Animal-free testing requirements |
Endotoxin Testing Workflow
Troubleshooting Common Endotoxin Testing Issues
Frequently Asked Questions (FAQs)
Q: My endotoxin test results show high variability between replicates. What could be causing this? A: High variability often stems from pipetting technique, particularly with viscous samples. Use positive displacement pipettes for time-sensitive assays, ensure proper vortexing of lyophilized standards (without vigorous mixing of LAL enzyme), and change gloves frequently to prevent cross-contamination. Perform all assays in replicates as recommended by USP guidelines [7].
Q: How should I handle sample interference in my endotoxin testing? A: Sample interference can be addressed through appropriate dilution, but not beyond the Maximum Valid Dilution (MVD). Validate dilution factors during assay development and perform spike recovery tests to ensure accurate detection. USP <85> suggests spike recovery between 50-200%, though many labs maintain stricter 75-150% criteria [7].
Q: What is Low Endotoxin Recovery (LER) and how can I address it? A: LER occurs when endotoxin signals become masked over time in certain formulations, leading to falsely low readings. To address LER, consider using multiple detection methods, evaluate different diluents, and consult regulatory guidelines for specific product types. Some regulators have requested tighter acceptance criteria to provide additional safety margins when LER is suspected [80].
Q: Can I pool finished product samples for endotoxin testing? A: For aqueous-based small-volume parenterals (≤100 mL), you can pool up to three units in a composite sample, but must adjust the MVD by dividing the individual sample MVD by the number of pooled samples. Do not pool products with low initial MVD, suspensions, or in-process samples from different manufacturing stages due to homogeneity concerns [13].
Q: How do I set endotoxin limits for combination therapies? A: For early-phase investigational oncology products used in combination with approved drugs, the FDA allows calculating endotoxin acceptance criteria without considering contribution from the approved drug. However, for marketing applications, sponsors must ensure the total endotoxin from all combination therapy components does not exceed 5 EU/kg/h. This allowance excludes cell/gene therapies and combinations of multiple investigational drugs [80].
Troubleshooting Guide: Common Problems and Solutions
| Problem | Potential Causes | Solutions |
|---|---|---|
| Failed spike recovery | Sample interference, improper standard preparation | Validate dilution factor, vortex standards vigorously, check for chemical interference |
| High background signal | Contaminated reagents or labware | Use endotoxin-free consumables, change gloves frequently, implement contamination controls |
| Non-linear standard curve | Improper standard dilution, degraded reagents | Prepare fresh standards, ensure proper serial dilution technique, check reagent storage conditions |
| Inconsistent replicates | Pipetting error, incomplete mixing | Train on specific assay protocols, use calibrated pipettes, ensure complete sample mixing |
| Out-of-specification results | True contamination, sampling error, testing error | Follow SOPs for retesting, investigate manufacturing process, review testing methodology |
Experimental Protocols for Endotoxin Control
Endotoxin Removal and Prevention Strategies
Detailed Protocol: Affinity Chromatography for Endotoxin Removal
Purpose: To remove endotoxin contamination from recombinant protein solutions during pre-clinical research and development.
Materials:
- Affinity chromatography resin appropriate for target protein
- Endotoxin-free buffers and solutions
- Low-protein-binding columns and tubing
- Endotoxin testing materials (LAL reagent, standards, endotoxin-free tubes)
Procedure:
- Column Preparation: Equilibrate affinity column with 5-10 column volumes of binding buffer
- Sample Loading: Apply protein sample at appropriate flow rate for maximum binding
- Washing: Wash with 10-15 column volumes of binding buffer to remove unbound contaminants
- Endotoxin-Specific Wash: Implement additional wash step with specialized endotoxin-removing buffer (e.g., containing non-ionic detergents or chelating agents)
- Elution: Elute target protein with elution buffer appropriate for the affinity tag
- Post-Processing: Cleave affinity tags if necessary and transfer to final formulation buffer
- Verification: Test final product for endotoxin content using appropriate BET method
Validation: Perform spike recovery tests to demonstrate endotoxin removal capability; document removal efficiency for research records [72].
The Researcher's Toolkit: Essential Reagent Solutions
| Reagent/Tool | Function | Key Considerations |
|---|---|---|
| LAL Reagents | Detection of endotoxins via gel-clot, chromogenic, or turbidimetric methods | Select appropriate sensitivity; ensure proper storage; validate for specific matrix |
| Endotoxin Standards | Calibration and standard curve generation | Use certified standards; vortex vigorously; prepare fresh for each assay |
| Endotoxin-Free Consumables | Prevention of sample contamination | Verify "endotoxin-free" designation (not just "sterile"); check detection range compatibility |
| Affinity Chromatography Resins | Endotoxin removal from protein solutions | Choose appropriate tag system; validate cleaning procedures; monitor binding capacity |
| Endotoxin-Removing Membranes | Additional purification step | Implement as final polish; validate compatibility with target protein |
| Specialized Wash Buffers | Enhanced endotoxin removal during purification | Optimize concentration of detergents/chelators; ensure protein compatibility |
Advanced Topics in Endotoxin Control
Special Considerations for Different Product Types
Biologics and Recombinant Proteins: Due to the potential for endotoxin contamination during expression and purification, implement multiple orthogonal removal methods and rigorous in-process testing. Even picomolar concentrations can cause anomalous results in sensitive systems [27].
Cell and Gene Therapies: These products often cannot be sterilized by conventional methods, making endotoxin prevention throughout manufacturing critical. They are excluded from certain allowances for combination therapies [80].
Medical Devices: Testing should follow rinsing/eluting techniques described in ISO 10993-1 and ISO 10993-12. Most endotoxin-related recalls involve medical devices rather than drug products [80] [13].
Combination Products: When used together, the sum of endotoxins from all components must not exceed 5 EU/kg/h. This may require dosing regimen changes if limits are approached [80].
Implementing Quality by Design (QbD) Concepts
A QbD approach to endotoxin control involves:
- Identifying critical process parameters affecting endotoxin levels
- Establishing design space for endotoxin removal operations
- Implementing real-time monitoring and control strategies
- Developing robust sampling plans that evolve with process knowledge
- Documenting changes through appropriate regulatory pathways (annual reports for drugs/biologics, 30-day notices for devices) [13]
Data Analysis and Regulatory Compliance
For regulatory compliance, initial linear regression of standard curves must yield correlation coefficient (r) ≥ 0.98. After this requirement is met, background-corrected, log-transformed, non-linear fits often provide accurate results for endpoint LAL assays with dynamic ranges greater than 20x [7].
Include a sample at your release criteria concentration in standard curves to maximize confidence in determining whether unknown samples are above or below this threshold. This practice provides the highest level of confidence in pass/fail determinations [7].
Frequently Asked Questions (FAQs)
Q1: What is the key advantage of guanidinium-based membrane adsorbers over traditional quaternary ammonium (Q) ones for endotoxin removal?
The primary advantage is their superior performance in high-conductivity and complex buffer matrices. While traditional Q-based adsorbers are effective in low ionic strength conditions, their efficiency decreases as conductivity increases. Guanidinium-based hybrid membrane adsorbers have demonstrated the ability to reduce endotoxin to the limit of detection across a wide pH range (4.7–8.3) and at conductivities as high as 43 mS/cm, conditions under which Q-based adsorbers are significantly impacted [81].
Q2: For a late-stage drug substance UF/DF operation, what is a key risk mitigation strategy for endotoxin control?
A key risk mitigation strategy is the removal of endotoxins during buffer preparation, prior to the UF/DF unit operation. Introducing an anion exchange (AEX) membrane adsorber step during buffer preparation can effectively reduce endotoxin load, preventing potential concentration of these contaminants in the final drug substance [81].
Q3: Besides charge-based adsorption, what other mechanism can be exploited for endotoxin removal?
Recent approaches also target the O-antigen portion of the endotoxin molecule through hydrogen bonding. This part of the molecule is highly enriched in hydrogen donors and acceptors. Adsorbents designed to exploit this mechanism can offer selectivity unaffected by pH, conductivity, chelating agents, surfactants, and organic solvents [41].
Troubleshooting Guides
Issue: Inadequate Endotoxin Clearance in High-Conductivity Buffers
Problem: Endotoxin levels remain too high after filtration through an AEX membrane, especially when using diafiltration or other complex, higher-conductivity buffers.
Solution:
- Assess Buffer Composition: Identify the salts and other components contributing to high ionic strength. Consult the compatibility chart below.
- Switch Adsorber Chemistry: Consider replacing a standard Q-based membrane adsorber with a guanidinium-based hybrid adsorber, which has demonstrated efficacy in conductivities up to 43 mS/cm [81].
- Pre-Treat Sample: If using a Q-based adsorber, ensure the buffer is in a low-ionic-strength condition. Dilution or diafiltration into a low-conductivity buffer may be necessary prior to the endotoxin removal step.
Issue: Low Protein Recovery After Endotoxin Removal Step
Problem: The target recombinant protein is binding to the endotoxin removal membrane and is not recovered in the flow-through.
Solution:
- Check Operational Mode: For proteins that should not bind the AEX media (like many antibodies), ensure you are operating in flow-through or void-exclusion mode (VEAX). In VEAX, the product flows through the void volume between particles while endotoxins bind, eliminating the need for sample equilibration [41].
- Adjust pH and Conductivity: Modify the sample conditions to a pH where your protein of interest is neutral or positively charged, ensuring it will not bind to the anion exchanger. A DOE (Design of Experiments) approach can help identify optimal conditions [41].
- Use Dissociative Additives: For proteins that form stable associations with endotoxins, pre-treat the sample with dissociative additives (e.g., 1 M guanidine, arginine, urea). In VEAX, the liberated product is excluded in the void volume while the dissociated endotoxin binds to the exchanger [41].
Case Study: Comparative Analysis of AEX Membrane Adsorbers for UF/DF Buffer Preparation
Objective: To evaluate and compare the endotoxin removal capabilities of two commercial quaternary amine (Q) membranes and one guanidinium functionalized hybrid adsorber from buffers representing UF/DF start and diafiltration buffer matrices [81].
Experimental Protocol:
Materials:
- Membrane Adsorbers:
- Cytiva Mustang E (Q1): Polyethersulfone membrane with a quaternized amine coating.
- Sartorius Sartobind Q (Q2): Stabilized reinforced cellulose with Q ligands.
- 3M Polisher ST (G1): A hybrid adsorber with a Q-functionalized nonwoven and a guanidinium-modified polyamide membrane.
- Buffers: UF/DF start buffer and a more complex diafiltration buffer were used.
- Endotoxin: Buffers were spiked with known concentrations of endotoxin.
- Membrane Adsorbers:
Methodology:
- A bracketing design study was used.
- Spiked buffers were processed through the different membrane adsorbers.
- The filtrate was collected and analyzed for endotoxin levels using a standard assay (e.g., LAL gel-clot assay).
- The reduction in endotoxin was measured and compared to the limit of detection (<0.1 EU/mL).
- For the guanidinium-based membrane (G1), a high-throughput test was performed by processing a UF/DF start buffer at a flux of 3,600 LMH up to 10,000 L/m² to simulate extended use.
Results and Data Analysis: The table below summarizes the key performance data from the case study, highlighting the operational windows of the different adsorbers [81].
TABLE 1: Comparison of Membrane Adsorber Performance for Endotoxin Removal
| Membrane Adsorber | Active Ligand | Performance in UF/DF Start Buffer (Low Ionic Strength) | Performance in UF/DF Diafiltration Buffer (Complex, Higher Ionic Strength) | Effective Conductivity Range |
|---|---|---|---|---|
| Cytiva Mustang E (Q1) | Quaternary Ammonium (Q) | Effective removal to limit of detection (<0.1 EU/mL) | Performance impacted by additional buffer components | Effective up to 24 mS/cm |
| Sartorius Sartobind Q (Q2) | Quaternary Ammonium (Q) | Effective removal to limit of detection (<0.1 EU/mL) | Performance impacted by additional buffer components | Information Not Specified |
| 3M Polisher ST (G1) | Guanidinium (G) & Q | Effective removal to limit of detection (<0.1 EU/mL) | Effective removal to limit of detection (<0.1 EU/mL) | Effective up to 43 mS/cm |
Conclusion: The guanidinium-based hybrid membrane adsorber (G1) provided a significantly wider operational window compared to the traditional Q-based membranes. It was the only technology tested that could reduce endotoxin to the limit of detection in both buffer matrices and under high-conductivity conditions, making it a robust risk-mitigation tool for late-stage UF/DF operations [81].
Experimental Workflow: Endotoxin Removal via Membrane Adsorbers
The following diagram illustrates the logical workflow for designing an experiment to evaluate or implement a membrane adsorber for endotoxin removal from buffers or protein solutions.
Mechanism of Guanidinium Action at the Molecular Interface
The efficacy of guanidinium ligands is rooted in their unique interfacial behavior. The diagram below illustrates the proposed mechanism of guanidinium cation adsorption to molecular interfaces, such as that of an endotoxin molecule.
This mechanism is supported by Deep-UV second harmonic generation spectroscopy, which has quantified the Gibbs free energy of adsorption (ΔG~ads~) for Gdm+ and found it to be larger than typical thermal energies, indicating a strong, thermodynamically favorable drive for the cation to reside at interfaces [82] [83]. This property makes it exceptionally effective at interacting with and binding endotoxins.
The Scientist's Toolkit: Key Research Reagent Solutions
TABLE 2: Essential Materials for Endotoxin Removal Experiments Featured in the Case Study
| Item Name | Function / Description | Example from Case Study |
|---|---|---|
| Guanidinium Hybrid Membrane Adsorber | Functionalized with guanidinium ligands; provides robust endotoxin removal across wide pH and conductivity ranges. | 3M Polisher ST (G1) [81] |
| Quaternary Ammonium (Q) Membrane Adsorber | Functionalized with quaternary amine groups; effective for endotoxin removal in low ionic strength conditions. | Cytiva Mustang E (Q1), Sartorius Sartobind Q (Q2) [81] |
| Limulus Amebocyte Lysate (LAL) Assay | Standard test for detecting and quantifying endotoxin levels in solutions. | Used to measure filtrate endotoxin concentration (e.g., <0.1 EU/mL) [81] [73] |
| Ultrafiltration/Diafiltration (UF/DF) Buffers | Process buffers used in the final steps of drug substance manufacturing; can be a source of endotoxin contamination. | UF/DF Start Buffer and Diafiltration Buffer used as test matrices [81] |
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) to assist researchers, scientists, and drug development professionals in reducing endotoxin contamination in recombinant protein research. Endotoxins, or lipopolysaccharides (LPS), are toxic components derived from the outer membrane of Gram-negative bacteria and can cause severe immune responses in patients, compromising the safety and efficacy of biological products [9]. A Quality by Design (QbD) approach emphasizes building quality into the product and process through prior understanding, rather than relying solely on end-product testing [84]. This guide outlines practical strategies for incorporating endotoxin control within a QbD framework.
Core QbD Principles for Endotoxin Control
Defining a Quality Target Product Profile (QTPP) and Critical Quality Attributes (CQAs)
The foundation of QbD is defining a Quality Target Product Profile (QTPP) which outlines the desired quality characteristics of the final drug product. From the QTPP, Critical Quality Attributes (CQAs) are identified. Endotoxin level is a classic CQA for injectable biologics, as it directly impacts patient safety [84]. The developability profile of a drug candidate rests on three pillars [84]:
- Manufacturability: Can the product be manufactured with the required purity and stability?
- Safety: Does the product avoid introducing dangerous side-effects, such as pyrogenic reactions from endotoxins?
- Pharmacology & Biological Activity: Does the product achieve the desired therapeutic outcome?
Risk Assessment and Contamination Control Strategy (CCS)
A contamination control strategy is a proactive, facility-wide plan derived from product and process understanding [85]. It involves identifying potential sources of endotoxin ingress and implementing controls to mitigate these risks. Key sources and controls include [86] [87] [85]:
- Water Systems: Maintain and regularly monitor Water-for-Injection (WFI) systems to prevent biofilm formation. Implement real-time endotoxin monitoring and validate sanitization cycles.
- Raw Materials: Source raw materials from validated suppliers and test for low endotoxin levels. Use low-endotoxin or endotoxin-free reagents.
- Personnel and Environment: Train personnel on proper gowning and aseptic techniques. Implement rigorous environmental monitoring in cleanrooms, including viable particle counts.
- Process Design: Utilize closed processing systems where possible and validate hold times for intermediates to prevent microbial growth.
The diagram below illustrates a systematic QbD-based workflow for risk assessment and control strategy development.
Troubleshooting Common Endotoxin Contamination Issues
| Problem | Possible Root Cause | Investigative Steps | Corrective & Preventive Actions |
|---|---|---|---|
| Consistently high endotoxin levels in final product | Inefficient purification step; stable endotoxin-protein complexes [40] | - Spiking study to test clearance capability of each purification step.- Analyze process buffers and raw materials for endotoxin. | - Optimize or introduce a dedicated endotoxin removal step (e.g., affinity chromatography) [19] [40].- Use dissociating agents (e.g., detergents) in sample prep [41]. |
| High endotoxin levels in cell culture harvest | Contaminated cell bank, raw materials, or bioreactor infection [87] | - Test cell banks and raw materials (sera, media) for bioburden/endotoxin.- Review aseptic techniques and sterility testing data. | - Implement stricter supplier qualification for raw materials.- Use low-endotoxin growth media and additives.- Enhance environmental monitoring. |
| Variable endotoxin recovery during LAL testing | Low Endotoxin Recovery (LER) phenomenon [88] | - Spike known endotoxin into product formulation and measure recovery over time. | - Adjust sample buffer conditions (pH, chelators).- Use alternative detection methods (e.g., recombinant Factor C assay) [85]. |
| Endotoxin spike not cleared by anion exchange | Improper sample conditions (pH, conductivity) [41] | - Measure sample pH and conductivity prior to loading.- Check protein pI and net charge under load conditions. | - Adjust sample pH/conductivity to ensure product and endotoxin have opposite charges.- Consider Void Exclusion Anion Exchange (VEAX) which is less sensitive to sample conditions [41]. |
| Endotoxin contamination of purified protein after storage | Non-endotoxin free containers or handling conditions [86] | - Test storage vials and buffers for endotoxin.- Review handling procedures and environment. | - Use certified endotoxin-free tubes, vials, and buffers.- Implement strict handling protocols for purified products. |
Frequently Asked Questions (FAQs)
Q1: What are the regulatory endotoxin limits for my biologic product? The general threshold for intravenous and subcutaneous drugs is 5 Endotoxin Units (EU) per kg per hour, while for intrathecal drugs, it is much lower at 0.2 EU/kg/hour [88]. For a drug product, this translates to a limit of K/M, where K=5 EU/kg (intravenous) and M=maximum human dose per kg in one hour. It is critical to consider the combined endotoxin load if administering multiple drugs concomitantly [88].
Q2: Why can't I just sterilize my protein to destroy endotoxins? Unlike viable bacteria, endotoxins are not inactivated by standard heat sterilization or autoclaving. The conditions required to destroy endotoxins (e.g., very high dry heat for extended periods) would denature and destroy your recombinant protein first [86] [40]. Therefore, the strategy must focus on prevention and removal, not destruction.
Q3: What is the most effective method for removing endotoxins from proteins? There is no single "best" method; the choice depends on your protein's properties. The table below compares common techniques. Often, a combination of methods integrated into the purification strategy is most effective [9] [41].
Q4: How does a QbD approach differ from traditional testing for endotoxin control? Traditional quality control often relies on Quality-by-Testing (QbT), where the focus is on testing the final product to reject non-conforming batches. In contrast, QbD is a systematic, proactive approach that builds endotoxin control into the process design through prior risk assessment, understanding of material attributes and process parameters, and continuous monitoring. This shifts the focus from detection to prevention [84] [85].
Q5: What is Low Endotoxin Recovery (LER) and how can I overcome it? LER describes the phenomenon where endotoxin spiked into certain biological formulations becomes undetectable by the LAL assay over time. This is often caused by the presence of chelating agents (e.g., EDTA) and surfactants (e.g., polysorbate) in the formulation [88]. To overcome LER, you can dilute the sample, use a different buffer for the assay, or employ an alternative detection method like the recombinant Factor C (rFC) assay, which may be less susceptible to LER [85].
Comparison of Endotoxin Removal Methods
| Method | Principle | Efficiency | Advantages | Limitations |
|---|---|---|---|---|
| Affinity Chromatography | Uses ligands (e.g., Polymyxin B, poly(ε-lysine)) that specifically bind endotoxin [19] [40]. | High (≥90-99% removal) [19] | High specificity; works under physiological conditions; can be used for sensitive proteins. | Resin can be expensive; may require optimization for different proteins; ligand can leach. |
| Ion Exchange Chromatography | Binds negatively charged endotoxins to a positively charged resin (anion exchanger) [9] [40]. | High (up to 5-log reduction) [40] | Well-established, scalable, integrates well with purification workflows. | Efficiency highly dependent on sample pH and conductivity; may not work if target protein is also negatively charged. |
| Void Exclusion Anion Exchange (VEAX) | Anion exchange that separates based on size and charge; does not require sample equilibration [41]. | High (2-4 log reduction) [41] | Tolerant of extreme sample conditions (pH, salt, denaturants); removes DNA/viruses simultaneously. | Limited sample volume per cycle (~40% of column volume); requires specific resin properties. |
| Two-Phase Separation (Triton X-114) | Uses detergent that partitions endotoxins into a detergent-rich phase upon temperature shift [9]. | Moderate to High (45-99%) [9] | Effective for dissociating stable endotoxin-protein complexes. | Requires removal of detergent residue; repeated heating/cooling may degrade sensitive proteins. |
| Ultrafiltration | Physical separation based on size; retains large endotoxin aggregates (>100 kDa) [9]. | Variable (28.9% to 99.8%) [9] | Simple, no binding involved. | Ineffective for smaller endotoxin monomers or fragments; efficiency depends on solution properties. |
Detailed Experimental Protocols
This method is particularly useful for breaking stable endotoxin-protein complexes.
Research Reagent Solutions:
| Item | Function |
|---|---|
| Triton X-114 | Non-ionic detergent that undergoes phase separation to partition endotoxins. |
| Endotoxin-free Water/Buffer | Prevents introduction of new endotoxin contamination. |
| Limulus Amebocyte Lysate (LAL) Assay Kit | For quantitative measurement of endotoxin levels before and after treatment. |
Methodology:
- Addition of Detergent: Add Triton X-114 to the protein sample to achieve a final concentration of 1% (v/v).
- Low-Temperature Incubation: Incubate the mixture at 4°C for 30 minutes with constant stirring to form a homogeneous solution.
- High-Temperature Phase Separation: Transfer the sample to a 37°C water bath and incubate for 10 minutes. The solution will become cloudy and separate into a detergent-rich phase (containing the endotoxin) and an aqueous phase (containing the protein).
- Centrifugation: Centrifuge at 20,000 × g for 10 minutes at 25°C to fully separate the two phases.
- Collection of Aqueous Phase: Carefully aspirate the upper aqueous phase, which contains your target protein. Avoid the lower detergent phase.
- Repeat Phase Separation (Optional): For further endotoxin reduction, subject the collected aqueous phase to 1–2 additional rounds of phase separation.
- Endotoxin Quantification: Measure endotoxin levels in the final aqueous phase using an LAL assay.
The workflow for this protocol is summarized below.
This is a quick, small-scale method ideal for purifying valuable protein samples in a research setting.
Research Reagent Solutions:
| Item | Function |
|---|---|
| High Capacity Endotoxin Removal Resin | Cellulose-based resin with a polycationic ligand that binds endotoxin. |
| Endotoxin-free Phosphate Buffered Saline (PBS) | Equilibration and wash buffer compatible with the resin. |
| 0.2N NaOH | For cleaning and regenerating the resin (sanitization). |
| 2M NaCl | Wash solution to remove non-specifically bound impurities. |
| LAL Assay Kit & BCA Protein Assay Kit | To measure endotoxin levels and protein recovery, respectively. |
Methodology:
- Column Preparation: Centrifuge the pre-packed spin column at 500 × g for 1 minute to remove the storage buffer.
- Column Cleaning (Optional but recommended): Wash the column with 0.2N NaOH and incubate overnight for depyrogenation. Then, wash with 2M NaCl followed by endotoxin-free water.
- Equilibration: Equilibrate the resin with three column volumes of endotoxin-free PBS (or your protein-compatible buffer).
- Sample Application: Load your protein sample (in a pH-neutral buffer like PBS) onto the column.
- Incubation: Incubate the column at room temperature (22°C) for 1 hour with gentle end-over-end mixing to allow endotoxin binding.
- Elution: Centrifuge the column at 500 × g for 1 minute to collect the purified flow-through protein sample.
- Analysis: Determine the endotoxin level in the flow-through using the LAL assay and measure protein recovery using a BCA protein assay.
Conclusion
Effective endotoxin control in recombinant protein production requires an integrated strategy spanning prevention, removal, and rigorous validation. Foundational understanding of contamination sources informs proactive controls, while methodological advances in membrane adsorbers, novel affinity ligands, and optimized chromatography provide powerful removal capabilities. Troubleshooting common issues like LER and optimizing process parameters are essential for robust performance, and validation with sensitive detection methods ensures compliance with evolving regulatory expectations. Future directions will focus on innovative technologies such as plant-produced binding proteins, enhanced single-use systems, and automated monitoring platforms that collectively promise to raise safety standards while streamlining biomanufacturing processes for next-generation biologics.
References
- 1. Lipopolysaccharide [https://en.wikipedia.org/wiki/Lipopolysaccharide]
- 2. Biochemistry, Lipopolysaccharide - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK554414/]
- 3. Pyrogens, Still a Danger [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-technical-guides/pyrogens-still-danger]
- 4. Controlling Endotoxin Contamination in Bioprocessing [https://www.genscript.com/protein-news/controlling-endotoxin-contamination-in-bioprocessing.html]
- 5. ProPure™ for life science research [https://www.news-medical.net/whitepaper/20251016/How-ProPuree284a2-is-redefining-precision-in-life-science-research.aspx]
- 6. Protocol for the removal of bound endotoxin from tau ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603731/]
- 7. Guide to Bacterial Endotoxin / LAL Testing - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/endotoxins-101/]
- 8. Do I need a validation prior to routine testing? [https://www.nelsonlabs.com/do-i-need-a-validation-prior-to-routine-testing/]
- 9. Endotoxin Removal Methods, Steps, and More [https://www.sinobiological.com/resource/protein-review/endotoxin-removal]
- 10. Plant produced endotoxin binding recombinant proteins ... [https://www.nature.com/articles/s41598-022-20776-6]
- 11. Septic Shock - Medscape Reference [https://emedicine.medscape.com/article/168402-overview]
- 12. Rapid Removal of Endotoxins & Pyrogens | EndotoxinOUT [https://www.gbiosciences.com/Protein-Research/Purification-Chromatography/Affinity-Purification-Resins/EndotoxinOUT?srsltid=AfmBOoqWyVxobza5szK0AEPymPwZFuWJ0k1xqsljyaWgHKL0w7c_5wN3]
- 13. Guidance for Industry: Pyrogen and Endotoxins Testing [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-pyrogen-and-endotoxins-testing-questions-and-answers]
- 14. Human Endotoxin (ET) Elisa Kit [https://www.afgsci.com/product/human-endotoxin-et-elisa-kit/]
- 15. Removal Of Bacterial Endotoxins [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/technology-and-research/plasmid-resource-center/removal-of-bacterial-endotoxins]
- 16. Common lab sources of Endotoxin and strategies for its ... [https://www.wakopyrostar.com/blog/kit-lal/post/common-lab-sources-of-endotoxin-and-strategies-for-its-detection-and-removal/]
- 17. Residual Endotoxin Contaminations in Recombinant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4257590/]
- 18. Bacterial Endotoxins/Pyrogens [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-technical-guides/bacterial-endotoxinspyrogens]
- 19. Eliminate Endotoxins from Protein and Antibody Samples [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/protein-biology-application-notes/eliminate-endotoxins-protein-antibody-samples.html]
- 20. Comparing Endotoxin Detection Methods [https://www.pharmtech.com/view/comparing-endotoxin-detection-methods]
- 21. The Rapid-Fire World of Endotoxin Testing [https://www.criver.com/eureka/the-rapid-fire-world-of-endotoxin-testing]
- 22. Overview of Endotoxin Testing Methods [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-purification-isolation/protein-purification/endotoxin-quantitation-removal/overview-of-endotoxin-testing-methods.html]
- 23. Efficient Endotoxin Testing Leveraging Recombinant Proteins [https://www.rapidmicrobiology.com/news/a-proven-framework-to-achieve-efficient-endotoxin-testing-leveraging-recombinant-proteins]
- 24. Comparison of bacterial endotoxin testing methods in ... [https://www.sciencedirect.com/science/article/pii/S1045105620300774]
- 25. Five Easy Ways to Keep Your Cell Cultures Endotoxin-Free [https://www.corning.com/worldwide/en/products/life-sciences/resources/stories/at-the-bench/five-easy-ways-to-keep-your-cell-cultures-endotoxin-free.html]
- 26. Top 5 tips for reducing endotoxin contamination in the lab [https://www.wakopyrostar.com/blog/kit-lal/post/top-5-tips-for-reducing-endotoxin-contamination-in-the-lab/]
- 27. Purity of Recombinant Proteins: Research Effects of Endotoxins - List Labs [https://listlabs.com/purity-recombinant-proteins/]
- 28. Affinity Chormatography Removes Endotoxins [https://www.biopharminternational.com/view/affinity-chormatography-removes-endotoxins]
- 29. Single step protocol to purify recombinant proteins with low ... [https://pubmed.ncbi.nlm.nih.gov/16290005/]
- 30. Validation of analytical methods in compliance with good ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3765465/]
- 31. Endotoxin depletion of recombinant protein preparations ... [https://www.sciencedirect.com/science/article/pii/S0003269714003534]
- 32. Bioburden Control: Testing, Definitions, and Best Practices [https://www.symmetric.events/blog-understanding-and-controlling-bioburden-definitions-testing-procedures-and-best-practices/?srsltid=AfmBOoooQZ3bpF4iMC9BMBf_MHtKs2xVWqD4C_6bEQjLDvWvUCmNnbl2]
- 33. Bioburden vs. Bacterial Endotoxin Testing [https://namsa.com/resources/blog/bioburden-vs-bacterial-endotoxin-testing-in-medical-devices/]
- 34. How to Prevent Endotoxin Contamination in Sterile ... [https://www.benchmarkproducts.com/2022/10/21/how-to-prevent-endotoxin-contamination-in-sterile-pharmaceutical-manufacturing/]
- 35. Somethin' Buggin' Ya? Get the Basics of Bioburden Testing [https://www.sartorius.com/en/knowledge/science-snippets/somethin-buggin-ya-get-the-basics-of-bioburden-testing-1444414]
- 36. Prefiltration & Bioburden Reduction [https://www.sartorius.com/en/products/process-filtration/prefiltration-bioburden-reduction]
- 37. Sterile Filtration and Bioburden Control for the Processing ... [https://www.criticalprocess.com/knowledge/sterile-filtration-and-bioburden-control-for-the-processing-of-biologics]
- 38. Removing endotoxin from biopharmaceutical solutions [https://www.pharmtech.com/view/removing-endotoxin-biopharmaceutical-solutions]
- 39. Removal of Endotoxin from Protein in Pharmaceutical ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/190810-Removal-of-Endotoxin-from-Protein-in-Pharmaceutical-Processes/]
- 40. Development and Qualification Factors for Endotoxin ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/589105-Development-and-Qualification-Factors-for-Endotoxin-Removal-from-Proteins-Using-Chromatographic-Columns/]
- 41. Recent Advances in Endotoxin Removal: An Upgrade to a ... [https://www.bioprocessintl.com/separation-purification/recent-advances-in-endotoxin-removal-an-upgrade-to-a-traditional-method-and-a-new-adsorption-chemistry]
- 42. Removal of endotoxin from recombinant protein preparations [https://pubmed.ncbi.nlm.nih.gov/9316739/]
- 43. Multimodal Anion Exchange Resin for Biotherapeutic ... [https://www.bioprocessintl.com/sponsored-content/evaluation-of-a-new-multimodal-anion-exchange-resin-for-emerging-biotherapeutic-process-challenges]
- 44. How to Choose Ion Exchange Resin? [https://ionresins.alfa-chemistry.com/how-to-choose-ion-exchange-resin.html]
- 45. Overview of Affinity Purification [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-affinity-purification.html]
- 46. LC Troubleshooting Essentials: A Guide to Common ... [https://www.chromatographyonline.com/view/lc-troubleshooting-essentials-a-guide-to-common-problems-and-solutions-for-peak-tailing-ghost-peaks-and-pressure-spikes]
- 47. Triton X-114 Sigma-Aldrich CAS No.9036-19-5 [https://www.sigmaaldrich.com/US/en/product/sial/x114?srsltid=AfmBOooHMPu7gmA9rwHxNH6E7tZShUh-X4YH0EEKr-bdd77XdGr6wa6Z]
- 48. Triton® X-114 Detergent [https://www.aatbio.com/resources/biological-detergents-properties-and-applications/triton-x-114]
- 49. A User's Guide for Phase Separation Assays with Purified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6215329/]
- 50. Recent development and application of membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9491666/]
- 51. Protein Purification Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/protein-purification-isolation-support-center/protein-purification-support/protein-purification-support-troubleshooting.html]
- 52. Diagnosing Chromatography Problems & Troubleshooting [https://www.ssi.shimadzu.com/service-support/faq/liquid-chromatography/knowledge-base/diagnosing-chromatography-problems-troubleshooting/index.html]
- 53. Validation of a Depyrogenation Tunnel [https://ispe.org/pharmaceutical-engineering/ispeak/validation-depyrogenation-tunnel]
- 54. Endotoxin & Depyrogenation Guide - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK613264/]
- 55. Examining Dry Heat Sterilizers and The Depyrogenation ... [https://www.azom.com/article.aspx?ArticleID=18734]
- 56. Low Endotoxin Recovery: A Comprehensive Overview for ... [https://www.biomerieux.com/corp/en/education/resource-hub/pharma-quality-control/scientific-library/low-endotoxin-recovery-comprehensive-overview.html]
- 57. Possible Mechanism of Low Endotoxin Recovery [https://www.americanpharmaceuticalreview.com/Featured-Articles/171005-Possible-Mechanism-of-Low-Endotoxin-Recovery/]
- 58. Biological Activity of Masked Endotoxin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5357793/]
- 59. Solving the Endotoxin Detection Challenge for Difficult Samples [https://www.biomerieux.com/us/en/education/resource-hub/scientific-library/pharma-microorganisms-library/revolutionize-your-endotoxin-testing/solving-the-endotoxin-detection-challenge.html]
- 60. Causes of Endotoxin Assay Failures and How to Avoid Them [https://www.rapidmicrobiology.com/news/common-causes-of-endotoxin-assay-failures-and-how-to-avoid-them]
- 61. Jundishapur Journal of Microbiology [https://brieflands.com/journals/jjm/articles/56329]
- 62. Efficient On‐Column Removal of Endotoxin from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590924/]
- 63. How to Implement Sustainable Endotoxin Testing [https://www.rapidmicrobiology.com/news/chapter-updated-how-to-implement-sustainable-endotoxin-testing]
- 64. A magnetic bifunctional endotoxin removal nano-agent for ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025042151]
- 65. Influence of pH control in the formation of inclusion bodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4177172/]
- 66. Detection and Quantification of Gram-Negative Bacterial ... [https://www.ncbi.nlm.nih.gov/books/NBK612347/]
- 67. Methods for the detection of bacterial endotoxins |PYROSTAR™ [https://www.wakopyrostar.com/blog/kit-lal/post/methods-for-the-detection-of-bacterial-endotoxins/]
- 68. Validation of Cleaning Processes (7/93) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/validation-cleaning-processes-793]
- 69. Preventing cross-contamination in multi-product facilities [https://www.pharmaceutical-technology.com/sponsored/preventing-cross-contamination-in-multi-product-facilities/]
- 70. Cleaning Validation for Biopharmaceutical Manufacturing ... [https://www.biopharminternational.com/view/cleaning-validation-biopharmaceutical-manufacturing-genentech-inc-part-1]
- 71. The Challenges of Multiproduct Facility Design [https://www.ipsdb.com/happenings/insights/the-challenges-of-multiproduct-facility-design]
- 72. Endotoxin removal and prevention for pre-clinical biologics ... [https://pubmed.ncbi.nlm.nih.gov/23081824/]
- 73. Removal of Endotoxin from Recombinant Protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0009912097000490]
- 74. Cleaning Validation: Protocol & Guidelines [https://safetyculture.com/topics/cleaning-validation]
- 75. How to Avoid Common Mistakes with LAL Assay |PTROSTAR [https://www.wakopyrostar.com/blog/post/how-to-avoid-common-mistakes-with-the-lal-assay/]
- 76. PYROGENT™ 250 Tests 0.125 EU/mL | Lonza [https://bioscience.lonza.com/lonza_bs/US/en/Endotoxin-Detection/p/000000000000186622/PYROGENT%E2%84%A2-Gel-Clot-LAL-Assay-(without-endotoxin)]
- 77. Turbidimetry Protocol & Troubleshooting - Creative Biolabs [https://www.creativebiolabs.net/turbidimetry.htm]
- 78. Common Technical Issues and Solutions in Bacterial ... [https://firegene.com/blogs/knowledge-center/common-technical-issues-and-solutions-in-bacterial-endotoxin-testing?srsltid=AfmBOoq5LqDCTLgugLKqwLZL7eGyn07_DWtuz7lvxJJgl9N0VZXBHqrZ]
- 79. Patient-Centric Quality Standards [https://www.sciencedirect.com/science/article/pii/S002235492400011X]
- 80. Patient-Centric Endotoxin Acceptance Criteria [https://www.bioprocessintl.com/bioanalytical-methods/establishing-patient-centric-endotoxin-acceptance-criteria-an-industry-opinion]
- 81. Comparative Analysis of Anion Exchange Membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226154/]
- 82. Strong adsorption of guanidinium cations to the air–water ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11745392/]
- 83. Adsorption of Guanidinium Cations to the Air-Water Interface [https://arxiv.org/html/2408.15423v1]
- 84. Early Implementation of QbD in Biopharmaceutical Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4449898/]
- 85. Facility-Driven Bacterial Endotoxin Control Strategies [https://investigationsquality.com/2025/02/19/facility-driven-bacterial-endotoxin-control-strategies/]
- 86. Endotoxin Contamination in Cleanrooms: Sources, Risks, and ... [https://cleanroom.contecinc.com/blog/endotoxin-contamination-in-cleanrooms]
- 87. Comprehensive Microbial Control Strategy [https://www.bioprocessintl.com/qa-qc/beyond-traditional-microbiology-testing-developing-a-comprehensive-strategy-for-microbial-control-and-detection]
- 88. Endotoxin levels in Biologics! [https://evidentic.com/endotoxin-levels-in-biologics/]