Optimizing Protein Concentration Measurement: A Guide to Enhanced Accuracy for Reliable Research and Development
Accurate protein quantification is a foundational pillar of research and drug development, yet it is challenged by the lack of a universal gold standard and numerous potential interferences.
Optimizing Protein Concentration Measurement: A Guide to Enhanced Accuracy for Reliable Research and Development
Abstract
Accurate protein quantification is a foundational pillar of research and drug development, yet it is challenged by the lack of a universal gold standard and numerous potential interferences. This article provides a comprehensive guide for researchers and scientists to navigate these challenges. It covers the core principles of protein assays, the strategic selection of methodologies for different applications, advanced troubleshooting and optimization techniques to overcome common pitfalls, and the rigorous validation required for regulatory compliance. By synthesizing current technologies and best practices, this resource aims to empower professionals to generate more precise, reproducible, and reliable protein data, thereby strengthening downstream analyses and conclusions.
The Foundation of Protein Quantification: Principles, Challenges, and the Quest for a Gold Standard
Why There Is No Universal Gold Standard for Protein Quantification
Protein quantification is a fundamental requirement in biological research and biopharmaceutical development, crucial for everything from drug discovery to release testing of final drug products [1]. Despite its importance, a single, universal "gold standard" method for accurately quantifying all proteins in every situation does not exist. This article explores the technical reasons behind this challenge and provides a structured guide to help researchers select and validate the most appropriate method for their specific needs.
FAQ: Understanding the Core Challenge
Why is there no single method that works for all proteins?
The immense structural diversity of proteins is the primary reason no single quantification method works universally. This variety leads to significant differences in physicochemical properties and microheterogeneity, which hinders universal quantification [1]. Proteins can differ in:
- Amino Acid Composition: Colorimetric assays (e.g., BCA, Bradford) rely on reactions with specific amino acids. Proteins with low proportions of these amino acids will yield inaccurate concentration estimates [2] [3].
- Size and Complexity: Large transmembrane proteins, for example, pose unique challenges as they are embedded in lipid membranes, making them less accessible to dyes and reagents [3].
- Post-Translational Modifications: Modifications like phosphorylation or glycosylation can alter a protein's structure and affect how it interacts with assay reagents or antibodies [4].
- Sample Matrix: Buffer components, detergents, reducing agents, and other molecules in the sample can interfere with many assay chemistries, leading to over- or under-estimation of concentration [1] [2].
What are the main limitations of common protein quantification methods?
The table below summarizes the pros and cons of widely used techniques, highlighting why their utility is context-dependent.
Table 1: Comparison of Common Protein Quantification Assays
| Assay Method | Principle | Pros | Cons | Best For |
|---|---|---|---|---|
| BCA Assay [2] | Colorimetric; reduction of Cu²⁺ by protein in an alkaline environment. | Compatible with many detergents; wide dynamic range; reasonably high throughput. | Susceptible to interference from reducing agents and metal chelators; relies on specific amino acids (Tyr, Trp, Cys). | General lab use with compatible buffers; determining total protein content in partially purified samples. |
| Bradford Assay [2] | Colorimetric; shift in absorbance of Coomassie dye upon binding to protein. | Rapid, one-step protocol; not affected by reducing agents. | Highly susceptible to interference from detergents (SDS, Triton) and buffer components (Tris, EDTA); relies on specific amino acids (Arg, Lys, Tyr). | Quick estimates of total protein in simple, detergent-free solutions. |
| UV Absorbance (A280) [2] | Measures absorbance of ultraviolet light by aromatic amino acids. | Quick and easy; no reagents or incubation; requires very low sample volume. | High interference from nucleic acids and common buffer components; low sensitivity; relies on aromatic amino acids. | Purified protein samples where the extinction coefficient is known and contaminants are absent. |
| ELISA [5] [2] | Immunoassay using antibody-antigen binding for specific detection. | High sensitivity and specificity; high throughput; works in complex samples. | Time-consuming optimization; longer assay time; higher cost; requires specific antibodies; provides semi-quantitative data unless carefully validated. | Quantifying a specific target protein in a complex mixture like serum or cell lysate. |
| Western Blot [5] [6] | Immunodetection after protein separation by electrophoresis. | High specificity; provides information on protein size and modifications; confirms identity. | Semi-quantitative; low throughput; time-consuming; technically complex; less sensitive than ELISA. | Confirming a protein's identity, checking for modifications, and semi-quantitative analysis when sample is limited. |
Troubleshooting Guides
How do I choose the right protein quantification assay?
Selecting the correct assay requires a systematic consideration of your specific protein, sample, and experimental context. The following decision workflow can guide your choice.
My assay results are inconsistent. What could be the cause?
Inconsistent results often stem from sample preparation issues or interference.
Problem: Interfering Substances in Buffer.
- Solution: Review your buffer composition against the assay's known interferents (see Table 1). Dilute the sample if possible, or use a cleanup method like precipitation. Consider switching to a more compatible assay (e.g., from Bradford to BCA if detergents are present) [2].
Problem: Protein Composition Affects Signal.
- Solution: Be aware that colorimetric assays are sensitive to amino acid composition. If your protein is rich or poor in certain amino acids, the concentration will be skewed. Use a standard protein that closely matches your target protein's composition for the calibration curve, or transition to an antibody-based method like ELISA for specific quantification [2] [3].
Problem: Protein Degradation or Instability.
- Solution: Labile proteins and proteases can cause degradation during sample handling. Keep samples on ice, use protease inhibitor cocktails, and minimize freeze-thaw cycles. For problematic samples, deactivate proteases by denaturation (e.g., with urea) if the assay can tolerate it [1].
Detailed Experimental Protocol: Indirect ELISA for Transmembrane Protein Quantification
This protocol is adapted from a study comparing quantification methods for Na, K-ATPase (NKA), a transmembrane protein, where conventional assays overestimated concentration compared to a targeted ELISA [3]. It demonstrates a method to overcome challenges with complex proteins.
Materials and Reagents
Table 2: Research Reagent Solutions for Indirect ELISA
| Item | Function / Description |
|---|---|
| 96-Well Microplate | Solid substrate for binding proteins and antibodies [5]. |
| Coating Buffer | (e.g., Carbonate-Bicarbonate buffer, pH 9.6) Optimizes adsorption of the antigen to the plate. |
| Blocking Buffer | (e.g., 1-5% BSA in PBS-T) Covers uncovered plastic surface to prevent non-specific antibody binding [5]. |
| Target Protein & Standard | The protein to be quantified. A purified standard of known concentration is required for the calibration curve. |
| Primary Antibody | An antibody with high specificity for the target protein [3]. |
| Enzyme-Linked Secondary Antibody | (e.g., HRP-conjugated) Binds to the primary antibody. The enzyme catalyzes the color-producing reaction. |
| Wash Buffer | (e.g., PBS with Tween 20 - PBS-T) Removes unbound antibodies and reagents to reduce background. |
| Enzyme Substrate | (e.g., TMB for HRP) A chromogenic compound that produces a measurable color change when cleaved by the enzyme [5]. |
| Stop Solution | (e.g., Acid) Halts the enzyme-substrate reaction at a defined time. |
| Microplate Reader | Instrument to measure the absorbance of the colored product in each well. |
Step-by-Step Methodology
- Coating: Dilute your protein samples and standards in a suitable coating buffer. Add a known volume (e.g., 100 µL) to each well of a 96-well microplate. Incubate the plate overnight at 4°C or for 1-2 hours at 37°C to allow the protein to adsorb to the well surface.
- Washing: Empty the plate and wash each well 2-3 times with wash buffer (e.g., PBS-Tween) to remove any unbound protein.
- Blocking: Add a blocking buffer (e.g., 1-5% BSA) to each well to cover all uncovered binding sites on the plastic. Incubate for 1-2 hours at room temperature. Wash the plate again as in step 2.
- Primary Antibody Incubation: Add the primary antibody, diluted in blocking buffer, to each well. Incubate for 1-2 hours at room temperature. Wash thoroughly to remove any unbound primary antibody.
- Secondary Antibody Incubation: Add the enzyme-conjugated secondary antibody, diluted in blocking buffer, to each well. Incubate for 1-2 hours at room temperature. Wash thoroughly again.
- Detection: Add the appropriate enzyme substrate to each well. Incubate in the dark for a defined period (typically 15-30 minutes) to allow color development.
- Stop Reaction and Read: Add the stop solution to each well to halt the reaction. Immediately measure the absorbance of the solution in each well using a microplate reader at the appropriate wavelength (e.g., 450 nm for TMB).
- Data Analysis: Generate a standard curve by plotting the absorbance of the standards against their known concentrations. Use the curve to interpolate the concentration of your unknown samples [5] [3].
Validating Your Protein Quantification Assay
For critical applications like drug development, assay validation is essential. Regulatory guidelines (e.g., ICH) require validation of parameters such as [1]:
- Accuracy: How close the measured value is to the true value.
- Precision: The closeness of agreement between a series of measurements (repeatability and intermediate precision).
- Specificity: The ability to assess the analyte unequivocally in the presence of other components.
- Linearity and Range: The interval over which the method provides results with direct proportionality to analyte concentration.
- Detection/Quantification Limit: The lowest amount of analyte that can be detected or quantified with acceptable accuracy and precision.
A risk-based strategy, such as Failure Mode and Effects Analysis (FMEA), can be an efficient approach to identify and control critical parameters in your quantification method [1].
Accurate protein quantification is a cornerstone of research in biochemistry, molecular biology, and drug development. The choice of assay directly impacts the reliability and reproducibility of experimental results, from Western blotting to enzyme kinetics studies. This guide details the core principles, methodologies, and troubleshooting for the four major protein quantification techniques—Bradford, BCA, Lowry, and UV Absorbance—to help optimize measurement accuracy in your research.
Core Principles and Mechanisms
Bradford Assay
The Bradford assay is a rapid, colorimetric method based on the binding of Coomassie Brilliant Blue G-250 dye to proteins. In an acidic environment, the dye shifts from a red-brown form (absorbance maximum at 465 nm) to a blue form (absorbance maximum at 610 nm) upon binding primarily to basic (arginine, lysine, and histidine) and aromatic amino acid residues in proteins [7] [8]. The absorbance of the resulting protein-dye complex is measured at 595 nm, and its intensity is proportional to the protein concentration [9]. The assay is sensitive for proteins larger than 3,000-5,000 Daltons [7] [10].
BCA (Bicinchoninic Acid) Assay
The BCA assay is a two-step reaction involving the reduction of Cu²⁺ to Cu¹⁺ by peptide bonds in an alkaline environment (the biuret reaction). The Cu¹⁺ ions then chelate with two molecules of bicinchoninic acid (BCA) to form a purple-colored complex [11]. The absorbance of this complex is measured at 562 nm and is proportional to the protein concentration. The reduction is also enhanced by the side chains of cysteine, cystine, tyrosine, and tryptophan residues [12].
Lowry Assay
The Lowry assay combines the biuret reaction (where peptide bonds reduce Cu²⁺ to Cu¹⁺ under alkaline conditions) with the subsequent reduction of the Folin-Ciocalteu reagent (phosphomolybdate/phosphotungstic acid) by the copper-treated protein [13] [14]. This second reduction step, primarily catalyzed by tyrosine, tryptophan, and cysteine residues, produces a deep blue-green color, measured at 650-750 nm [13]. This combination makes it more sensitive than the biuret reaction alone.
UV Absorbance at 280 nm
This direct method leverages the innate ultraviolet absorbance of aromatic amino acids, primarily tryptophan and tyrosine, in the protein backbone. The absorbance at 280 nm is measured and related to concentration using the Beer-Lambert law, with the protein's specific extinction coefficient [15]. Note that light scattering from particulates or aggregates can lead to inaccuracies [15].
Comparative Analysis of Protein Assays
The table below provides a quantitative comparison of the four major protein assays to guide method selection.
| Feature | Bradford Assay | BCA Assay | Lowry Assay | UV Absorbance |
|---|---|---|---|---|
| Principle | Dye-binding (Coomassie Blue) | Copper reduction & BCA chelation | Copper reduction & Folin-Ciocalteu | Aromatic amino acid absorbance |
| Detection Wavelength | 595 nm [7] [8] | 562 nm [11] | 650–750 nm [13] [14] | 280 nm [15] |
| Typical Sensitivity Range | 1–1,500 µg/mL [7] | 20–2,000 µg/mL [11] | 5–100 µg/mL [13] | Varies by protein |
| Key Compatible Substances | Buffers, metal ions, reducing agents, chelators [7] | Detergents, reducing agents (low conc.) [11] | - | N/A (sample-dependent) |
| Key Interfering Substances | Detergents [7] [8] | High conc. reducing agents & chelators [12] [11] | Detergents, reducing agents, carbohydrates, EDTA [13] | Nucleic acids, turbidity, buffers with UV absorbance |
| Assay Time | ~10 minutes [7] | 30 min (37°C) – 2 hr (RT) [11] | ~40 minutes [13] [14] | Immediate |
| Protein-to-Protein Variability | High (binds basic/aromatic aa) [7] | Moderate (enhanced by Cys, Tyr, Trp) [11] | Moderate (dependent on Tyr, Trp) [13] | High (dependent on Trp/Tyr content) |
| Cost & Complexity | Low, simple [8] | Moderate [14] | Moderate [14] | Low, no reagents |
Troubleshooting Guides and FAQs
Bradford Assay
Q: My Bradford assay samples show low or no absorbance. What could be wrong?
- Cause: The protein sample may be too dilute, or its molecular weight may be below the 3,000-5,000 Dalton detection limit [10].
- Solution: Concentrate the sample or switch to a more sensitive assay like the BCA for small proteins/peptides [10].
- Cause: The Bradford reagent may be old, improperly stored, or used while too cold [10].
- Solution: Use fresh reagent that has been brought to room temperature before use [10].
Q: A precipitate formed upon adding the Bradford reagent. How can I fix this?
- Cause: Detergents in the protein buffer (e.g., Triton X-100) are a common cause of precipitation [7] [10].
- Solution: Dialyze the sample or dilute it to a point where the detergent no longer interferes. Consider using a detergent-compatible Bradford assay kit [7] [10].
BCA Assay
Q: The color development in my BCA assay is inconsistent.
- Cause: Fluctuations in incubation temperature can directly impact the rate of color development [11].
- Solution: Ensure a consistent and accurate incubation temperature (e.g., 37°C) and protect the plate from temperature gradients [11].
- Cause: Inaccurate pipetting of the working reagent or samples [12].
- Solution: Use calibrated pipettes and reverse pipetting for viscous reagents to improve accuracy.
Q: My BCA standard curve is poor, or I get a "Standards Incorrect" error on my instrument.
- Cause: The kit may have expired, been stored incorrectly, or the BSA standard may be degraded [12].
- Solution: Always prepare fresh calibration standards and replace the kit if components are expired or contaminated [12].
Lowry Assay
Q: The Lowry assay gives inaccurate readings for my protein sample.
- Cause: The sample buffer contains interfering substances like reducing agents (DTT, β-mercaptoethanol), detergents (SDS), or strong alkaline buffers [13] [14].
- Solution: Dialyze or desalt the sample into a compatible buffer. Alternatively, precipitate the protein to remove interfering substances and re-dissolve it [12] [14].
Q: Why do different proteins give different responses in the Lowry assay?
- Cause: The Folin-Ciocalteu reaction depends on the content of tyrosine, tryptophan, and cysteine residues, which varies between proteins [13].
- Solution: For maximum accuracy, use a purified sample of the target protein itself to prepare the standard curve, rather than BSA [12].
UV Absorbance
Q: My protein concentration measured by A280 seems artificially high.
- Cause: Significant interference from nucleic acids, which have a strong absorbance peak at 260 nm [15].
- Solution: Use a correction formula (e.g.,
Protein Concentration (mg/mL) = 1.55*A280 - 0.76*A260) or purify the protein further. - Cause: Light scattering from particulates or protein aggregates in the solution [15].
- Solution: Clarify the sample by centrifugation or filtration before measurement.
Q: The spectrophotometer gives unstable or drifting baseline readings.
- Cause: Aging lamp, insufficient warm-up time, or debris in the light path or cuvette [16].
- Solution: Allow the instrument to warm up for 15-30 minutes, calibrate it regularly, and use clean, scratch-free cuvettes [16].
Detailed Experimental Protocols
Protocol 1: Bradford Assay (Microplate Format)
This protocol is adapted for high-throughput analysis using a microplate reader [7] [8].
Research Reagent Solutions:
| Item | Function |
|---|---|
| Coomassie Dye Reagent | Binds to protein, causing a color shift for detection [8]. |
| Bovine Serum Albumin (BSA) Standard | Provides known protein concentrations to generate a standard curve [8]. |
| Compatible Buffer (e.g., PBS) | Used to dilute the protein standard and unknown samples [8]. |
Procedure:
- Prepare Standard Curve: Serially dilute BSA standard in PBS to create a range of concentrations (e.g., 0, 0.1, 0.2, 0.5, 1.0 mg/mL) [8].
- Prepare Samples: Dilute unknown protein samples in the same buffer as the standards.
- Add Reagents: Pipette 20-150 µL of each standard and unknown sample into a microplate well. Add 1 mL of Bradford reagent to each well and mix thoroughly [8].
- Incubate: Incubate the plate at room temperature for 5-10 minutes [7] [8].
- Measure Absorbance: Read the absorbance at 595 nm using a microplate reader.
- Analyze Data: Plot the standard curve (Absorbance vs. BSA concentration) and use the linear regression equation to calculate the concentration of the unknown samples [8].
Protocol 2: Lowry Assay (Test Tube Format)
This is the classic two-step protocol for the Lowry assay [13] [14].
Research Reagent Solutions:
| Item | Function |
|---|---|
| Lowry Reagent A (Alkaline Copper) | Creates alkaline conditions for the Biuret reaction (Cu²⁺ reduction) [14]. |
| Lowry Reagent B (Folin-Ciocalteu) | Is reduced by the copper-treated protein to produce the final blue color [13]. |
| BSA Standard | Provides known protein concentrations for the standard curve [14]. |
Procedure:
- Prepare Standard Curve: Prepare BSA standards in the range of 0-100 µg/mL [14].
- Add Reagent A: To 1 mL of each standard and unknown sample, add 1 mL of Lowry Reagent A. Mix and incubate for 10 minutes at room temperature [13] [14].
- Add Reagent B: Add 0.1 mL of Lowry Reagent B, mix rapidly and thoroughly immediately after addition. Incubate for 30 minutes in the dark [13] [14].
- Measure Absorbance: Read the absorbance at 750 nm [14].
- Analyze Data: Generate a standard curve and interpolate the unknown sample concentrations.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Kit | Primary Function | Key Considerations for Selection |
|---|---|---|
| Bradford Plus Kit with Pre-diluted Standards | Fast, convenient protein quantification with reduced pipetting steps [7]. | Ideal for high-throughput labs; reduces standard preparation errors [7]. |
| Detergent-Compatible Bradford Assay | Quantifies protein in samples containing up to 1% detergents (Triton X-100, NP-40) [7]. | Essential for protein extracts from membrane preparations [7]. |
| BCA Protein Assay Kit | Sensitive, detergent-tolerant quantification via copper reduction [11]. | Preferred over Bradford for samples with detergents or when using plastic cuvettes [11]. |
| Pierce 660 nm Protein Assay | Protein quantification using a dye-metal complex; compatible with most detergents and reducers [7]. | Excellent alternative to Bradford with better linearity and wider detergent compatibility [7]. |
| Folin-Ciocalteu Reagent | Key component for the colorimetric detection step in the Lowry assay [13]. | Light-sensitive and has a limited shelf life once diluted [13]. |
| Ultra-Pure BSA Standard | Provides a highly accurate and consistent protein standard for calibration curves. | Critical for assay accuracy; ensures standard curve reliability across experiments [8]. |
Understanding Key Interfering Substances for Each Assay Type
FAQs: Navigating Common Interference Issues
1. My immunoassay is showing a falsely elevated (or depressed) result for a patient sample, but I suspect this doesn't match the clinical picture. What could be the cause?
This is a classic sign of interference in immunoassays. The issue often stems from endogenous substances in the patient's sample, such as:
- Heterophile antibodies or human anti-animal antibodies that can bind to assay antibodies, interfering with the reaction [17].
- Cross-reacting substances, including structurally similar drugs or their metabolites, which the assay antibody mistakenly recognizes [17].
- Rheumatoid factors (autoantibodies) that can cause similar interference [17].
- Endogenous binding proteins (e.g., hormone binding globulins) that may alter the measurable concentration of the analyte [17].
2. My Bradford assay shows unexpectedly high background or low absorbance. What are the usual suspects?
The Bradford assay is highly sensitive to the composition of your sample buffer. Common interfering substances and their effects are detailed in the table below. Frequently, the culprits are:
- Detergents in your protein buffer, which often cause precipitates or high background [10].
- High alkaline concentrations, which can raise the pH beyond the assay's limits, turning the sample dark blue [10].
- The sample containing a low molecular weight protein below the assay's detection limit (~3,000-5,000 Daltons) [10].
3. I am setting up a digital PCR assay and see positive signals in my No Template Control (NTC). Is this always contamination?
Not necessarily. To determine the cause, examine the mean relative fluorescence unit (RFU) of the positive control samples.
- If the positives in your NTCs have the same fluorescence as your true samples, it is likely contamination [18].
- If the positives are of much lower amplitude, more random, or diffused, it is likely an assay artifact [18]. Proper threshold setting, informed by the NTC's negative population, is crucial to avoid this issue [18].
4. For my Immunoprecipitation (IP) experiment, I get a low or no signal. What should I investigate first?
Begin by troubleshooting your experimental conditions:
- Check your lysis buffer: Stringent lysis conditions (e.g., using RIPA buffer containing ionic detergents like sodium deoxycholate) can disrupt protein-protein interactions in co-IP experiments. Use a milder cell lysis buffer instead [19].
- Confirm protein expression: Verify that your target protein is expressed at detectable levels in your cell line or tissue [19].
- Include essential controls: Always run an input lysate control to confirm the presence of your target protein and the functionality of your antibody [19].
Troubleshooting Guides: Key Interfering Substances by Assay
Protein Quantification Assays
Table 1: Common Interfering Substances in Protein Quantification Assays
| Assay Type | Key Interfering Substances | Maximum Tolerable Concentration (Approx.) | Observed Effect | Recommended Solution |
|---|---|---|---|---|
| Bradford Assay | Detergents (SDS, Triton X-100) [10] | Varies by detergent (e.g., 0.01% SDS) [10] | Precipitation, high background [10] | Dilute sample, dialyze, or use alternative assay [10] |
| Alkaline Buffers [10] | - | Sample turns dark blue [10] | Dilute or dialyze sample [10] | |
| BCA Assay | Reducing Agents (e.g., DTT, β-Mercaptoethanol) [12] | ≤1 mM DTT [1] | Reduction of Cu²⁺, falsely high absorbance [12] | Use BCA Reducing Agent Compatible Assay or dialyze sample [12] |
| Chelators (e.g., EDTA) [12] | ≤10 mM EDTA [1] | Chelation of Cu²⁺, falsely low absorbance [12] | Dilute sample to lower EDTA concentration [12] | |
| Micro BCA Assay | Reducing Agents & Chelators [12] | Similar to BCA | Same as BCA assay | Dilute, dialyze, or precipitate protein [12] |
| 660 nm Assay | Ionic Detergents [12] | - | Altered color response, inaccurate readings [12] | Use a compatible assay (e.g., BCA) or remove detergent [12] |
| Modified Lowry Assay | Detergents, Reducing Agents, Chelators [12] | - | Altered color development | Remove interfering substances via dialysis or precipitation [12] |
Immunoassays (e.g., ELISA, AlphaLISA)
Table 2: Common Interfering Substances in Immunoassays
| Interfering Substance | Assay Type Impacted | Observed Effect | Recommended Solution |
|---|---|---|---|
| Heterophile Antibodies [17] | Sandwich Immunoassays | Falsely elevated or falsely low results [17] | Use blocking agents, alternate assay, or sample pre-treatment [17] |
| Human Anti-Animal Antibodies [17] | Immunoassays using animal antibodies | Falsely elevated or depressed values [17] | Use species-specific blocking reagents or employ alternative methods [17] |
| Cross-reacting Molecules (e.g., metabolites, drugs) [17] | Drug, Hormone, and Tumor Marker assays | Over- or underestimation of analyte [17] | Use a more specific assay (e.g., LC-MS/MS) [17] |
| Lysis Buffer Incompatibility | AlphaLISA SureFire | Reduced or abolished signal [20] | Use kit-specific lysis buffer; RIPA buffer is often incompatible unless diluted [20] |
| High Biotin Levels (in media/serum) [20] | Assays using streptavidin-bead chemistry | High background or suppressed signal [20] | Use biotin-free assay kits or dilute sample [20] |
| High DMSO Concentration [20] | Cell-based assays (e.g., AlphaLISA) | Can affect cell health and signaling | Keep concentrations ≤2% where possible [20] |
Experimental Protocols for Identifying and Overcoming Interference
Protocol 1: Systematic Approach to Detect Immunoassay Interference
When a laboratory result is clinically discordant, follow these steps to investigate potential interference [17]:
- Clinical Flagging: The physician communicates the clinical suspicion to the laboratory. This partnership is essential for identifying problematic results [17].
- Re-testing: Repeat the analysis on the same platform.
- Alternate Method Analysis: Re-measure the analyte using a different immunoassay platform or, ideally, a method based on a different principle (e.g., chromatography).
- Linearity and Dilution Test: Perform serial dilutions of the patient sample with a non-immune serum or assay buffer. A non-linear dilution profile is a strong indicator of interference.
- Blocking Experiments: Pre-incubate the sample with a blocking reagent designed to neutralize heterophile or human anti-animal antibodies (e.g., heterophile blocking tubes). Recovery of the result post-blocking confirms this type of interference [17].
- Ultrafiltration or Precipitation: For small analyte interference, these physical separation techniques can be useful.
Protocol 2: Testing for Substance Interference in Colorimetric Protein Assays
If you suspect your sample buffer is interfering with a Bradford, BCA, or similar assay, use this method to confirm [10]:
- Prepare Two Standard Curves:
- Curve A: Prepare your protein standard (e.g., BSA) dilutions in ultrapure water or a compatible buffer.
- Curve B: Prepare identical protein standard dilutions in your sample's buffer.
- Perform the Assay: Run both standard curves according to your standard protocol.
- Analyze the Data: Plot protein concentration versus absorbance for both curves.
- Interpretation: If the slopes of the two curves are significantly different, the sample buffer is interfering with the assay. If the slopes match, the buffer is not causing interference [10].
- Mitigation: If interference is confirmed, you can:
- Dilute the Sample: If the protein concentration is high enough, dilute the sample to reduce the interferent below its threshold.
- Dialyze or Desalt: Transfer the protein into a compatible buffer.
- Precipitate and Re-dissolve: Use TCA/acetone precipitation to pellet the protein, then dissolve the pellet in a compatible buffer [12].
Visual Guide: Mechanisms of Immunoassay Interference
The following diagram illustrates the primary mechanisms through which substances can interfere with sandwich immunoassays, a common format for protein detection.
The Scientist's Toolkit: Key Reagents for Interference Management
Table 3: Essential Reagents and Materials for Troubleshooting Interference
| Reagent / Material | Function in Troubleshooting | Example Use Case |
|---|---|---|
| Heterophile Blocking Reagents [17] | Neutralizes interfering heterophile and human anti-animal antibodies in patient samples. | Added to serum samples prior to immunoassay analysis to confirm and eliminate antibody-mediated interference. |
| Protein A / G Beads [19] | Binds antibodies for immunoprecipitation; choice depends on antibody host species for optimal binding. | Protein A for rabbit IgG, Protein G for mouse IgG in IP and co-IP experiments to ensure efficient pull-down. |
| Compatibile Lysis Buffers [19] [20] | Effectively extracts target protein without disrupting protein complexes or assay chemistry. | Using a mild cell lysis buffer (#9803) for co-IP instead of a denaturing RIPA buffer to preserve protein interactions. |
| Protease/Phosphatase Inhibitor Cocktails [19] | Prevents degradation and post-translational modification changes of the target protein during sample preparation. | Added to cell lysis buffers to maintain protein phosphorylation states for phospho-specific assays. |
| Biotin-Free Assay Kits [20] | Eliminates interference from endogenous biotin present in samples like serum or cell culture media. | Used in bead-based assays (e.g., AlphaLISA) when high biotin media (e.g., FBS) causes high background. |
| Reference Standards [1] | Calibrates the assay; should closely match the sample protein in composition and matrix. | Using a well-characterized, stable reference standard that is quantified by a primary method for accurate relative quantification. |
The Critical Role of Protein Quantification in Drug Development Pipelines
Protein quantification is a foundational step in the biopharmaceutical pipeline, from early drug discovery to final product release. Accurate measurement is critical for ensuring drug efficacy, safety, and consistent dosing. This technical support center addresses common challenges and provides solutions to optimize the accuracy of your protein concentration measurements.
Protein Quantification Method Selection Guide
Choosing the appropriate quantification method is the first critical step in ensuring data accuracy. The table below compares the most commonly used techniques to help you select the right assay for your application [1].
| Method | Principle | Detection Range | Key Advantages | Key Limitations | Best for Drug Development Stage |
|---|---|---|---|---|---|
| Bradford Assay | Coomassie dye binding to basic/aromatic residues [10] | ~1-1500 μg/mL [1] | Rapid, simple, compatible with many buffers [10] | Interference from detergents; variable response to different proteins [1] | Discovery (high-speed screening) [1] |
| BCA Assay | Cu²⁺ reduction in alkaline solution (biuret reaction) and BCA chelation [12] | ~0.0005-2000 μg/mL [1] | Good tolerance to many buffer substances; more uniform protein response [1] | Interference from reducing agents and chelators [12] | Discovery & Development (good balance of speed and accuracy) [1] |
| UV Absorbance | Absorption of light at 280 nm by aromatic amino acids | Varies by protein | Non-destructive; direct measurement without standards | Interference from nucleic acids, turbidity, and other UV-absorbing compounds [1] | All stages (quick estimate, requires pure sample) |
| Amino Acid Analysis | Acid hydrolysis and derivatization of amino acids [1] | N/A | Highly accurate and reproducible; considered an absolute method [1] | Complex, slow, requires specialized equipment [1] | Late-stage Development & QC (reference method) |
| ELISA | Antigen-antibody binding with enzymatic detection [5] | High sensitivity (e.g., sub-pg/mL for nELISA) [21] | High specificity and sensitivity; excellent for complex mixtures [5] [22] | Mainly for specific proteins, not total protein; can have false positives/negatives [5] | Development & QC (specific protein/impurity quantification) [1] |
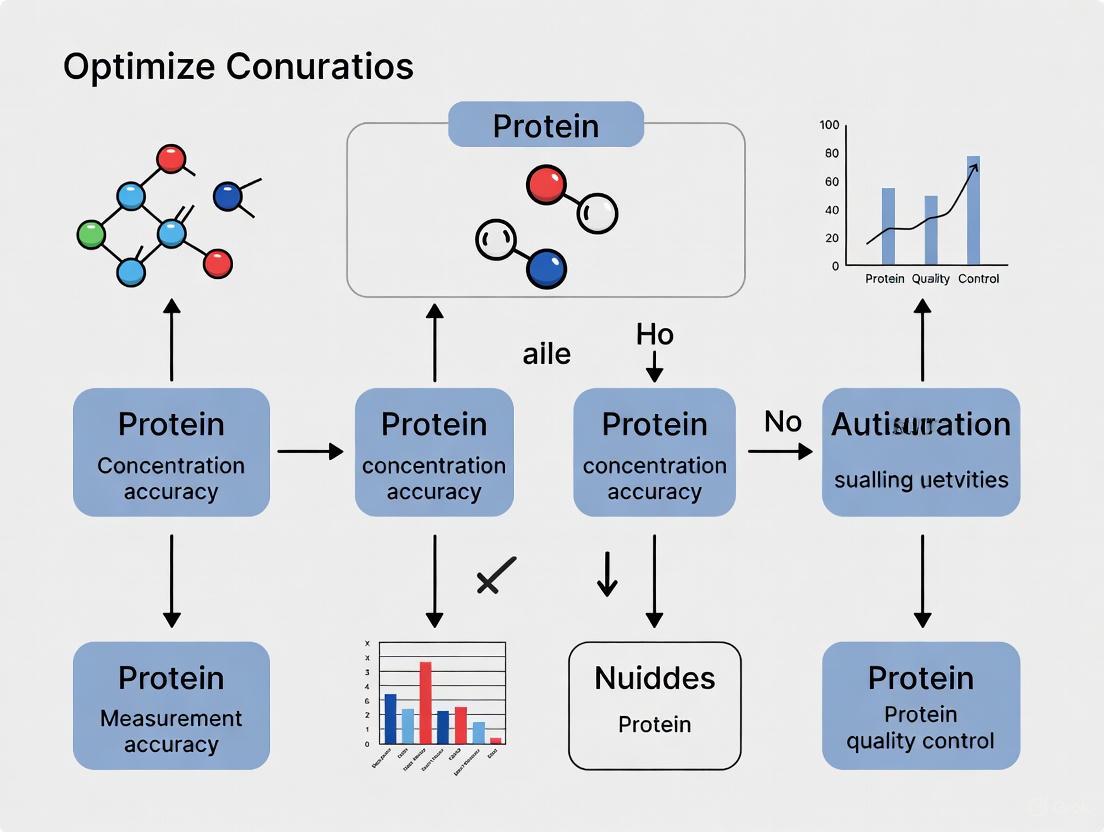
Method Selection Workflow
The following diagram outlines a logical workflow for selecting the most appropriate protein quantification method based on your experimental goals and sample type.
Troubleshooting Common Protein Assay Problems
Even with the correct method chosen, various issues can arise during experimentation. Here are solutions to frequently encountered problems.
| Problem | Possible Cause | Solution |
|---|---|---|
| Low Absorbance | Protein MW < 3-5 kDa | Use an alternative assay (e.g., BCA) for smaller proteins or peptides. |
| Interfering substances | Dilute the sample. Ensure standards are prepared in the same buffer. Dialyze if necessary. | |
| Absorbance Too High | Protein concentration too high | Dilute the sample and repeat the assay. |
| Precipitates Formed | Detergents in protein buffer | Dialyze or dilute the sample to reduce detergent concentration. |
| Dark Blue Color | High alkaline concentration | Dilute or dialyze the sample to bring pH within a compatible range. |
| Inconsistent Standards | Old or improperly stored dye | Replace outdated Bradford reagent (typical shelf life ~12 months). |
| Incorrect wavelength | Ensure absorbance is measured at 595 nm. |
| Problem | Possible Cause | Solution |
|---|---|---|
| Inconsistent Results | Varying incubation temperature | Ensure a consistent incubation temperature (typically 37°C) across all samples/standards. |
| Delays in reading plates | Read all samples at the same time post-incubation; use a timer. | |
| Over-/Under-estimation | Interfering substances (reducing agents, chelators) | Remove substances via dialysis, precipitation, or use a compatible assay kit. |
| Poor standard preparation | Use a fresh standard that resembles your sample protein, prepared in the same buffer. | |
| High Background | Contamination in buffer | Replace the kit or buffer. Use clean cuvettes/microplates. |
Frequently Asked Questions (FAQs)
| Factor | ELISA | Western Blot |
|---|---|---|
| Primary Use | Quantifying specific proteins (e.g., cytokines, biomarkers) in a sample [5]. | Confirming the presence, size, and identity of a specific protein in a complex mixture [5] [6]. |
| Throughput | High. Ideal for screening many samples quickly in a 96-well plate format [5] [22]. | Low. Typically analyzes 10-15 samples per gel, making it slower for large studies [22]. |
| Data Output | Quantitative. Provides precise concentration values [5]. | Semi-Quantitative. Provides relative abundance and molecular weight information [22]. |
| Specificity | High, but can be prone to false positives/negatives if not optimized [5]. | Very high, as it confirms protein identity by molecular weight, and is often used to confirm ELISA results [5] [6]. |
| Information Gained | Presence and concentration of a target. | Presence, size, protein modifications (e.g., phosphorylation), and cleavage events [6] [22]. |
Buffer incompatibility is a common issue. Here is a strategic approach to solve it:
- Dilution: The simplest method. Dilute your sample several-fold in a compatible buffer to reduce the concentration of the interfering substance to a non-inhibitory level. This is only feasible if your starting protein concentration is high enough [12] [10].
- Dialysis or Desalting: Physically remove the interfering substances by transferring the sample into a compatible buffer using dialysis, desalting columns, or buffer exchange kits [12].
- Protein Precipitation: Precipitate your protein using acetone or trichloroacetic acid (TCA). The pellet, once washed, can be re-dissolved in an assay-compatible buffer [12].
- Assay Selection: Choose a more compatible assay. For example, the BCA assay is generally more tolerant of reducing agents than the Bradford assay, which is highly sensitive to detergents [12] [10] [1].
- Pipetting Errors: This is a frequent culprit, especially with small or viscous volumes. Verify your pipetting technique and calibrate your pipettes regularly.
- Sample Homogeneity: Ensure your samples are thoroughly mixed before aliquoting. Protein can adhere to tube walls, leading to uneven concentration.
- Temperature Fluctuations: The color development in assays like BCA is temperature-sensitive. Ensure consistent incubation temperature across all runs [23].
- Instrument Calibration: Regularly calibrate your spectrophotometer or microplate reader to ensure accurate absorbance measurements [23].
The field is moving towards higher multiplexing and sensitivity. A key innovation is the nELISA platform [21]. It combines a DNA-mediated, bead-based sandwich immunoassay with advanced multicolor bead barcoding. This design pre-assembles antibody pairs on target-specific barcoded beads, which spatially separates different assays and prevents reagent cross-reactivity—the main barrier to high-level multiplexing. This technology allows for profiling hundreds of proteins (e.g., a 191-plex inflammation panel) across thousands of samples with high sensitivity and specificity, making it a powerful tool for large-scale phenotypic screening in drug discovery [21].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function | Key Considerations |
|---|---|---|
| BSA (Bovine Serum Albumin) | The most common protein standard for generating calibration curves in colorimetric assays [10]. | If your target protein's amino acid composition differs greatly from BSA, consider using a different standard (e.g., IgG) for improved accuracy [12] [1]. |
| Compatible Assay Kits | Kits designed to tolerate specific interfering substances (e.g., BCA Reducing Agent Compatible Assay) [12]. | Select based on your sample buffer composition. Always check the manufacturer's compatibility table. |
| Microplates & Cuvettes | Vessels for holding samples during absorbance measurement. | Use glass or plastic cuvettes for Bradford assay, as the dye can react with quartz. Ensure all vessels are clean and scratch-free [10] [23]. |
| High-Quality Antibodies | Critical for immunoassays like ELISA and Western blot (capture and detection) [22]. | For Sandwich ELISA, ensure antibody pairs are raised in different species and bind to non-overlapping epitopes [22]. |
| Blocking Agents (e.g., BSA) | Used to coat unused binding sites on plates or membranes to prevent non-specific antibody binding [22]. | A 1% BSA solution is commonly used. Prepare fresh or store appropriately to prevent contamination. |
Experimental Workflow for Validated Protein Quantification
Adhering to a standardized workflow is crucial for generating reliable and reproducible data, especially in a regulated drug development environment. The following diagram outlines a generalized protocol for protein quantification and assay validation.
Navigating Regulatory Requirements and Pharmacopoeial Methods
In pharmaceutical development and clinical diagnostics, the accuracy of protein concentration measurements is paramount. Regulatory agencies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) mandate strict validation of bioanalytical methods to ensure the safety and efficacy of drugs and biological products [24]. Adherence to these guidelines and pharmacopoeial standards is not optional; it is a fundamental requirement for generating data that is accepted in regulatory submissions worldwide. This guide addresses common challenges and provides troubleshooting advice for maintaining compliance while optimizing the accuracy of protein quantification methods such as ELISA, BCA, and Bradford assays.
Frequently Asked Questions (FAQs) on Regulatory Compliance
Q1: What are the core validation parameters required for a regulatory-compliant protein assay?
According to FDA and EMA guidelines, validating a bioanalytical method like ELISA requires characterizing several key parameters [24]:
- Accuracy and Precision: Closeness of individual measurements to the true value (accuracy) and the reproducibility of the measurement (precision), both within (intra-assay) and between (inter-assay) runs.
- Specificity and Selectivity: The ability of the assay to unequivocally assess the target analyte in the presence of other components, such as impurities or matrix components.
- Linearity and Range: The ability of the assay to obtain results directly proportional to the analyte concentration within a given range.
- Sensitivity: The lowest amount of analyte that can be reliably detected, often defined as the Lower Limit of Detection (LLOD).
- Robustness: A measure of the assay's capacity to remain unaffected by small, deliberate variations in method parameters.
Q2: What are the consequences of using a poorly validated assay?
A poorly validated assay can lead to several critical errors, including the generation of false positive and false negative results [24]. Common issues like insufficient plate washing, excessive detection reagent, or cross-reactivity can yield a high background signal, compromising data accuracy. Furthermore, a lack of lot-to-lot consistency in reagents can also lead to erroneous results, potentially jeopardizing drug safety assessments and leading to costly delays in product development.
Q3: How do I choose between BCA and Bradford methods for my regulatory submission?
The choice depends on the specific sample composition and potential interferents. The table below compares the two methods:
| Parameter | BCA Assay [25] | Bradford Assay [25] [26] |
|---|---|---|
| Principle | Reduction of Cu²⁺ to Cu⁺ in alkaline medium, detected by BCA dye. | Shift in absorbance of Coomassie G-250 dye upon binding protein. |
| Compatible with Detergents | High (Tolerates up to 5% SDS, Triton X-100, Tween) | Low (SDS must be <1%; Triton X-100 <0.1%) |
| Compatible with Reducing Agents | Low (Interfered by DTT, β-mercaptoanol, TCEP, EDTA) | High (Tolerates DTT, β-mercaptoanol, TCEP, EDTA) |
| Protein-to-Protein Variation | Moderate (Influenced by cysteine, tyrosine, tryptophan) | High (Influenced by arginine and lysine content) |
| Key Advantage | Robust in the presence of detergents. | Fast, simple, and tolerant of reducing agents. |
Troubleshooting Guides for Common Experimental Issues
Issue 1: High Background or Non-Specific Signal in Immunoassays
A high background signal can mask true results and lead to inaccurate quantification.
| Possible Cause | Recommended Solution |
|---|---|
| Insufficient Blocking | Optimize the type, concentration, and incubation time of the blocking buffer (e.g., 5% BSA or non-fat dry milk) [24] [27]. |
| Antibody Concentration Too High | Titrate both primary and secondary antibodies to find the optimal dilution that maximizes signal-to-noise ratio [27]. |
| Incomplete Washing | Ensure thorough washing throughout the protocol to remove unbound reagents. Increase wash times or the number of wash cycles [24] [27]. |
| Cross-reactivity of Antibodies | Check antibody specification sheets for validated applications. Pre-absorbed antibodies may be necessary for complex samples [24]. |
Issue 2: No Signal or Weak Signal
The absence or weakness of an expected signal is a common frustration that can stem from multiple sources.
| Possible Cause | Recommended Solution |
|---|---|
| Antibody Incorrect or Inactive | Use a positive control to verify antibody activity. Ensure antibodies are stored correctly and not used beyond their expiration date [27]. |
| Insufficient Antigen/Protein | Increase the amount of protein loaded. Check for protein degradation by using fresh protease inhibitors during sample preparation [27]. |
| Inefficient Transfer (Western Blot) | Use Ponceau S staining or Coomassie staining of the gel post-transfer to confirm protein has moved to the membrane [27]. |
| Incompatible Buffer Components | For BCA, avoid chelators like EDTA and reducing agents. For Bradford, avoid high concentrations of detergents [25]. |
Issue 3: Poor Standard Curve Linearity
A non-linear or poorly fitting standard curve prevents accurate quantification of unknown samples.
| Possible Cause | Recommended Solution |
|---|---|
| Inaccurate Pipetting or Standard Preparation | Use calibrated pipettes and prepare fresh serial dilutions of the standard carefully [25]. |
| Assay Range Exceeded | Ensure the absorbance values of unknown samples fall within the range of the standard curve. Dilute samples as needed [24]. |
| Matrix Effects | Match the standard diluent to the sample matrix as closely as possible to ensure similar behavior [24]. |
Essential Experimental Protocols
This method is ideal for samples containing detergents.
- Prepare Standard Dilutions: Create a series of Bovine Serum Albumin (BSA) standards in a buffer matching your sample matrix, covering a range from 0 to 1000 µg/mL.
- Prepare BCA Working Reagent: Mix reagents A and B in a 50:1 ratio. This working reagent is stable at room temperature for 24 hours.
- Add Samples and Reagent: Pipette 20 µL of each standard and unknown sample into a microplate or test tube. Add 200 µL of BCA working reagent to each.
- Incubate and Measure: Incubate the plate or tubes at 37°C for 30 minutes. Cool to room temperature.
- Read Absorbance: Measure the absorbance at 562 nm using a plate reader or spectrophotometer.
- Calculate Concentrations: Subtract the average blank absorbance from all standards and samples. Plot the standard curve (Absorbance vs. Concentration) and use the linear equation to calculate the concentration of your unknowns.
This method is fast and tolerant of reducing agents.
- Prepare Standard Dilutions: Prepare BSA or γ-globulin standards as described for the BCA assay.
- Add Samples and Reagent: Pipette standards and unknowns into a microplate. Add Bradford reagent to each well.
- Incubate and Measure: Incubate at room temperature for 5-10 minutes. The color is stable for up to one hour.
- Read Absorbance: Measure the absorbance at 595 nm.
- Calculate Concentrations: Generate a standard curve and calculate unknown concentrations as described in the BCA protocol.
Workflow Visualization: Bioanalytical Method Validation
The following diagram outlines the logical workflow for establishing a compliant and robust protein quantification method.
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and their functions for setting up protein quantification assays.
| Item | Function | Key Considerations |
|---|---|---|
| BCA Assay Kit [25] | Colorimetric quantification of total protein based on the reduction of Cu²⁺. | Choose based on compatibility with detergents; avoid with reducing agents. |
| Bradford Assay Kit [25] [26] | Colorimetric quantification based on dye binding to arginine/lysine residues. | Ideal for quick results and samples with reducing agents; avoid with detergents. |
| Microplate Reader | Measures absorbance in 96-well or 384-well plates for high-throughput analysis. | Must have filters for appropriate wavelengths (e.g., 562nm for BCA, 595nm for Bradford). |
| BSA (Bovine Serum Albumin) | Serves as the standard reference protein for generating calibration curves. | Ensure high purity and prepare fresh dilutions for accurate standard curves. |
| Coated ELISA Plates [24] | Solid phase pre-coated with capture antibody for specific antigen detection. | Check lot-to-lot consistency to prevent variability and ensure assay reproducibility. |
| High-Affinity Antibodies [24] | Primary and secondary antibodies for specific target detection in immunoassays. | Must be validated for the specific application (e.g., Western blot, ELISA). Titrate for optimal signal. |
| Blocking Buffer (e.g., BSA, Non-fat Milk) [24] [27] | Prevents non-specific binding of antibodies to the plate or membrane, reducing background. | Type must be optimized; some antibodies may cross-react with proteins in milk. |
Strategic Method Selection and Application Across the Research Pipeline
Accurate protein quantification is a foundational step in biomedical research and drug development, directly impacting the validity of downstream analyses and experimental conclusions. The accuracy of these measurements is highly dependent on the specific combination of your protein sample and the buffer components it is in. This guide provides a structured framework to navigate the complex landscape of protein assays, helping you select the optimal method to ensure reliable and reproducible results for your specific experimental conditions.
Selecting the right quantification method is the first critical step. The table below summarizes the most common colorimetric and fluorescent protein assays, their principles, advantages, and key limitations [28].
| Assay Method | Fundamental Principle | Key Advantages | Major Disadvantages |
|---|---|---|---|
| UV Absorption | Measures absorbance of aromatic amino acids (Tyr, Trp) at 280 nm [28]. | Simple and quick; no reagents required [28]. | High error with protein mixtures; interfered by any UV-absorbing substances (e.g., nucleic acids) [28]. |
| Bradford (Dye-Binding) | Coomassie dye binds proteins under acidic conditions, causing a spectral shift [28] [29]. | Fast, easy, and compatible with reducing agents and metal chelators [28]. | Incompatible with detergents; high protein-to-protein variation [28] [29]. |
| BCA (Bicinchoninic Acid) | Copper ions (Cu²⁺) reduced by proteins in an alkaline medium (Biuret reaction); BCA chelates the reduced Cu⁺ [28]. | Compatible with most detergents; less protein-to-protein variation than Bradford [28]. | Incompatible with reducing agents (e.g., DTT) and copper-chelating agents [28] [30]. |
| Lowry | Copper-protein complex (Biuret) enhanced by the Folin-Ciocalteu reagent [28]. | Linear response curve; less protein-to-protein variation than dye-based assays [28]. | Incompatible with detergents, reducing agents, and chelators [30]. |
| Fluorescent Assays | Protein-binding fluorescent dyes (e.g., NanoOrange, Qubit assays) [28]. | Excellent sensitivity; timing is not critical; suitable for high-throughput automation [28]. | Requires a specialized instrument (fluorometer) [28]. |
The Decision Matrix: Matching Your Sample to the Assay
The presence of interfering substances in your sample buffer is the single greatest factor affecting accuracy. Use the following flowchart and compatibility table to guide your selection.
Figure 1: A workflow to guide the initial selection of a protein assay based on the presence of common interfering substances [28] [30].
Matrix of Common Interfering Substances [28] [30] [1]
| Interfering Substance | Bradford Assay | BCA Assay | Lowry Assay | Fluorescent Assays |
|---|---|---|---|---|
| Detergents (e.g., Triton X-100, SDS) | Not Compatible | Compatible | Not Compatible | Varies by assay; generally low tolerance for additional detergents [30] |
| Reducing Agents (e.g., DTT, β-mercaptoethanol) | Compatible | Not Compatible | Not Compatible | Generally Compatible [30] |
| Chelators (e.g., EDTA) | Compatible | Not Compatible | Not Compatible | Information Not Available |
| Salts, Solvents, Buffers | Mostly Compatible [28] | Mostly Compatible | Mostly Compatible | Mostly Compatible [30] |
FAQs and Troubleshooting Guides
Q1: My protein assay results are inconsistent. What are the most common causes?
- Incompatible Buffer Components: This is the most frequent issue. Cross-reference your buffer recipe with the compatibility table above [28] [30].
- Inaccurate Standard Curve: The standard curve must be prepared fresh each time the assay is performed, especially for non-linear assays like Bradford. Using expired or improperly stored standards will also lead to errors [28] [30].
- Protein-to-Protein Variation: Different proteins can yield different color responses. Bovine Serum Albumin (BSA) is a common standard, but if high accuracy is required, a purified version of your target protein is ideal [28] [29].
- Improper Pipetting: Small volumetric errors are magnified in microplate-scale assays. Use calibrated pipettes and good technique [30].
Q2: How can I overcome buffer incompatibility without changing my assay?
- Sample Dilution: Diluting your sample several-fold in a compatible buffer can reduce the concentration of the interfering substance below its threshold of interference. This is only feasible if your protein concentration is high enough to remain within the working range after dilution [30].
- Dialysis or Desalting: These techniques physically separate your protein from small interfering molecules (e.g., DTT, salts) by exchanging the buffer for one that is compatible with your chosen assay [28] [30].
- Protein Precipitation: Precipitate your protein using acetone or trichloroacetic acid (TCA), remove the supernatant containing the interferent, and then re-dissolve the protein pellet in a compatible buffer [30].
Q3: When should I use BSA versus IgG as my protein standard?
- Bovine Serum Albumin (BSA): This is the most widely used general-purpose standard. It is inexpensive, highly pure, and produces a consistent color response [28].
- Immunoglobulin G (IgG): Use IgG (or Bovine Gamma Globulin, BGG) as your standard when you are quantifying antibodies. IgG produces a color response curve more similar to other immunoglobulins, providing greater accuracy for these specific samples [28].
Q4: My sample volume is very small and the protein is dilute. What are my options?
For dilute samples, sensitivity becomes paramount. Micro BCA and fluorescent assays (e.g., NanoOrange, Qubit) offer excellent sensitivity and are well-suited for quantifying total protein in dilute samples, often requiring less sample volume [28].
Detailed Experimental Protocols
Protocol 1: BCA Assay (Microplate Procedure)
This copper-based assay is ideal for samples containing detergents but lacking reducing agents [28].
Research Reagent Solutions:
- BSA Standard: Prepare a series of BSA dilutions in the same buffer as your unknown samples.
- BCA Working Reagent (WR): Mix Reagent A (sodium carbonate, BCA) with Reagent B (copper sulfate) at a 50:1 ratio.
Methodology:
- Prepare Standard Curve: Pipette 0, 2.5, 5, 10, 15, and 20 µL of BSA standards in duplicate into a microplate. Bring the volume in each well to 20 µL with buffer.
- Add Unknown Samples: Pipette 20 µL of each unknown sample into wells.
- Add BCA Reagent: Add 200 µL of the BCA WR to each well. Seal the plate and mix thoroughly.
- Incubate: Incubate the plate at 37°C for 30 minutes or at room temperature for 2 hours. The higher temperature increases sensitivity.
- Measure Absorbance: Cool the plate to room temperature. Measure the absorbance at 562 nm on a plate reader.
- Calculate Concentration: Generate a standard curve from the blank-corrected averages of the standard replicates and use the linear equation to determine the concentration of your unknowns.
Protocol 2: Overcoming Interference via Protein Precipitation
This protocol is effective for removing small interfering molecules like DTT [30].
Research Reagent Solutions:
- Precipitation Reagent: 100% w/v Trichloroacetic Acid (TCA).
- Wash Solvent: Acetone, chilled to -20°C.
- Compatible Solubilization Buffer: A buffer known to be compatible with your chosen assay (e.g., PBS).
Methodology:
- Precipitate: Add 100% TCA to your protein sample to a final concentration of 10-20% TCA. Incubate on ice for 10-30 minutes. A protein pellet should form.
- Centrifuge: Centrifuge at >10,000 × g for 10 minutes to pellet the protein.
- Wash: Carefully decant the supernatant. Wash the pellet with ice-cold acetone to remove residual TCA and interferents. Centrifuge again and decant.
- Dry: Air-dry the pellet briefly to evaporate residual acetone.
- Re-dissolve: Solubilize the protein pellet in a compatible buffer using vortexing and gentle heating if necessary.
- Assay: Proceed with your chosen protein assay.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in Protein Quantification |
|---|---|
| Bovine Serum Albumin (BSA) | The most common protein standard for generating calibration curves [28]. |
| Bovine Gamma Globulin (BGG) | A more appropriate standard when quantifying antibody samples [28]. |
| Compatible Lysis Buffers | Buffers formulated without detergents or reducing agents for universal compatibility, or specific buffers matched to your assay choice. |
| Dialysis Cassettes/Desalting Columns | For buffer exchange to remove small interfering substances from protein samples [28] [30]. |
| Trichloroacetic Acid (TCA) / Acetone | For precipitating proteins to separate them from interfering substances in the solution [30]. |
| Microplates and Cuvettes | The vessel for performing the assay and measuring absorbance/fluorescence. |
| Spectrophotometer / Plate Reader | Instrument required to measure the colorimetric (absorbance) or fluorescent signal produced by the assay [28]. |
Advanced Considerations: Buffer Composition and Protein Stability
The buffer itself can profoundly influence your protein's state and thus the quantification result. When choosing a buffer, consider:
- Optimal pH: Work at a pH that maintains your protein's stability and activity. The buffer's pKa should be within one pH unit of your experimental pH for effective buffering capacity [31].
- Additive Effects: A single component may be below its interference threshold, but a combination of several substances in a complex sample buffer can collectively interfere with the assay [30].
- Protein Stability Screening: Different buffers can promote or prevent protein aggregation and denaturation. If possible, screen your protein's stability in different buffer conditions to ensure you are quantifying native, soluble protein [31].
Methodologies for Drug Discovery vs. Clinical Release Testing
Frequently Asked Questions (FAQs)
Q1: Why is the choice of protein quantification method different in the drug discovery phase compared to the clinical release testing phase?
The requirements for speed, precision, and regulatory compliance differ fundamentally between these stages [1].
- Drug Discovery: The primary goal is speed and sensitivity. Materials are often available in low quantities and purity. Methods need to be fast and flexible to screen many candidates. Common techniques include colorimetric assays (e.g., BCA, Lowry) and simple 1D gels [1].
- Clinical Release Testing: The primary goal is accuracy, robustness, and regulatory compliance. The method must be rigorously validated to ensure exact dosing for patient safety. Techniques described in pharmacopoeias, such as amino acid analysis, are preferred for easier regulatory acceptance [1].
Q2: What are the most common interfering substances in protein quantification assays, and how can I troubleshoot them?
Interference is a major cause of inaccurate quantification. The table below summarizes common issues and solutions [1] [32].
| Interfering Substance | Effect on Quantification | Troubleshooting Strategies |
|---|---|---|
| Detergents | Can disrupt dye binding in colorimetric assays, leading to inaccurate readings. | Use a detergent-compatible assay (e.g., amido-black). Dialyze or desalt the sample to remove detergents [1]. |
| Reducing Agents & Chaotropes | May interfere with the chemistry of certain assays. | Check the assay's tolerance levels for these agents. A robust assay like amido-black may be less susceptible [1]. |
| Nucleic Acids | Absorb light at similar wavelengths to proteins in UV absorbance methods, causing overestimation. | Switch to a fluorescence-based method (e.g., Qubit assay) that is minimally affected by nucleic acids [32]. Use a purification step to remove nucleic acids [32]. |
| Other Buffer Components | Salts, sugars, and lipids can affect assay chemistry. | Always include a buffer-only negative control to account for background interference [1]. Perform a serial dilution of your sample; if the results are non-linear, interference is likely. |
Q3: What does a "validated" protein quantification method for clinical release entail?
According to ICH guidelines, a validated quantitative method must demonstrate several key parameters [1]:
- Accuracy: How close the measured value is to the true value.
- Precision: The closeness of agreement between a series of measurements (including repeatability and intermediate precision).
- Specificity: The ability to assess the analyte unequivocally in the presence of other components.
- Linearity and Range: The interval over which the method provides results with direct proportionality to analyte concentration.
- Detection Limit (LOD) and Quantification Limit (LOQ): The lowest amount of protein that can be detected or quantified with acceptable accuracy and precision [1].
Q4: My protein is unstable. How can I ensure reliable quantification?
Protein degradation during sample preparation will make accurate quantification impossible [1].
- Immediate Processing: Keep samples on ice and process them quickly.
- Inhibit Proteases: Add protease inhibitor cocktails to your lysis or storage buffers.
- Controlled Denaturation: Deactivate proteases by denaturing the sample in urea or SDS, but only if your chosen quantification assay can tolerate these substances [1].
Methodology Comparison Tables
Table 1: Comparison of Protein Quantification Methods by Development Stage
This table compares the key characteristics of methods typically used in different phases of drug development [1] [33].
| Method | Primary Use Case | Key Advantages | Key Limitations | Regulatory Acceptance |
|---|---|---|---|---|
| Colorimetric Assays (BCA, Bradford) | Drug Discovery | Fast, cost-effective, works with a broad range of proteins, high-throughput compatible. | Susceptible to interference from detergents and reducing agents; measures total protein, not specific drug substance [1]. | Not typically used for final product release. |
| Amino Acid Analysis | Clinical Release Testing | Highly accurate and reproducible; considered an absolute quantification method [1]. | Technically complex, requires specialized equipment, time-consuming [1]. | High; easily accepted by regulatory authorities [1]. |
| Mass Spectrometry (e.g., AQUA) | Drug Discovery / Characterization | High specificity for the drug substance; can quantify specific isoforms and post-translational modifications [1]. | Expensive, requires expert operation, complex data analysis. | Growing acceptance, particularly for characterizing complex molecules. |
| ELISA | Impurity Testing / Potency Assays | Extremely high sensitivity and specificity for a particular protein or impurity [1]. | Antibody specificity must be thoroughly characterized; may not distinguish between active and inactive forms [1]. | Well-accepted for specific applications (e.g., host cell protein assays). |
| Fluorescence-Based (e.g., Qubit) | Drug Discovery (Sensitive Applications) | High sensitivity, minimal interference from nucleic acids, requires small sample volumes [32]. | Requires a dedicated fluorometer, more expensive per sample than colorimetric assays. | Not typically used for final product release. |
Table 2: Key Validation Parameters for Quantitative Assays in Clinical Release
This table defines the critical parameters that must be validated for a protein quantification method used in clinical release testing, based on ICH guidelines [1].
| Validation Parameter | Definition | Importance in Clinical Release |
|---|---|---|
| Accuracy | The closeness of agreement between the measured value and a true accepted reference value. | Ensures the drug product contains the exact, labeled dose for patient safety and efficacy [1]. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling. | Ensures the manufacturing process is consistent and controlled, batch after batch [1]. |
| Repeatability | Precision under the same operating conditions over a short time (intra-assay). | Demonstrates the reliability of the assay within a single run [1]. |
| Intermediate Precision | Precision within the same laboratory (different days, different analysts). | Demonstrates the assay's robustness to normal lab variations [1]. |
| Specificity | The ability to measure the analyte accurately in the presence of other components (excipients, impurities). | Ensures the measurement is of the drug protein and is not skewed by the formulation matrix [1]. |
| Linearity | The ability to obtain results directly proportional to the concentration of the analyte. | Confirms the assay works accurately across the required concentration range (e.g., dose variations) [1]. |
| Range | The interval between the upper and lower concentrations for which linearity, accuracy, and precision are demonstrated. | Defines the acceptable concentrations for which the assay is validated [1]. |
Experimental Workflow & Visualization
Workflow for Protein Quantification Method Selection
This diagram outlines a logical decision process for selecting and validating a protein quantification method based on the stage of drug development and specific needs.
Protein Quantification Assay Workflow
This diagram details the general workflow for performing a protein quantification, using a fluorescence-based assay as an example.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Protein Quantification
This table lists key reagents, kits, and instruments used in protein quantification, along with their primary function in an experiment.
| Reagent / Kit / Instrument | Primary Function in Protein Quantification |
|---|---|
| BCA (Bicinchoninic Acid) Assay Kit | A colorimetric method for determining total protein concentration based on the reduction of Cu²⁺ to Cu⁺ in an alkaline environment. |
| Bradford Assay Kit | A colorimetric method that uses Coomassie dye, which binds to proteins and shifts its absorbance maximum. |
| Qubit Protein Assay Kit | A highly sensitive fluorescence-based method that uses a dye selective for proteins, minimizing interference from contaminants [32]. |
| Amino Acid Analysis Service | Provides absolute quantification of protein concentration by hydrolyzing the protein and quantifying its constituent amino acids [1]. |
| Bovine Serum Albumin (BSA) | The most common protein used to prepare standard curves for calibrating colorimetric and fluorescent assays [32]. |
| Spectrophotometer / Plate Reader | An instrument that measures the absorbance of light by a sample, used for reading colorimetric assays like BCA and Bradford. |
| Fluorometer | An instrument that measures the intensity of fluorescent light emitted by a sample, required for assays like the Qubit system [32]. |
| HPLC System with UV Detector | Used for high-precision separation and quantification of proteins or peptides, often in a GMP environment for release testing [1] [33]. |
Frequently Asked Questions (FAQs)
Q1: Why is it critical to distinguish between quantifying the drug substance and total protein content?
A: The distinction is fundamental to drug safety and efficacy. Providing an exact and reproducible drug dose to a patient is critical [1]. If your goal is to measure the active therapeutic protein itself (the drug substance), you need a specific assay. If you need to measure the total protein content in a sample, which may include impurities, host cell proteins, or degraded products, you use a general assay. Using the wrong type of assay can lead to inaccurate dosing, miscalculation of impurity levels, and ultimately, unreliable data for regulatory submissions [1] [34].
Q2: What are the primary types of assays for specific versus general quantification?
A: The choice of assay depends entirely on your quantification goal. The table below summarizes the main categories:
| Quantification Goal | Description | Common Assay Technologies |
|---|---|---|
| Total Protein Content | Measures all proteins in a mixture, including the drug substance, host cell proteins, and impurities [1]. | Colorimetric assays (Bradford, Lowry, BCA) [28] [35], UV Absorbance at 280 nm [36] [35]. |
| Drug Substance (Specific Protein) | Quantifies only the active therapeutic protein, often in the presence of a complex matrix like a formulation or biological fluid [1] [36]. | Immunoassays (ELISA) [1] [3], Mass Spectrometry (LC-MS/MS) [1] [37] [36], Western Blots [1]. |
Q3: My sample is in a complex buffer. How do I choose a compatible assay?
A: Buffer components are a major source of interference. Selecting an assay tolerant of your sample's matrix is crucial for accuracy. The following table compares the compatibility of common total protein assays with various substances.
| Assay Method | Principle | Key Interfering Substances | Compatible Substances |
|---|---|---|---|
| Bradford Assay | Dye-binding to basic amino acids (Arg, Lys) [28] [36]. | Detergents (SDS, Triton X-100) [28] [36], strongly alkaline buffers [35]. | Reducing agents (DTT), metal-chelating agents, most salts and solvents [28]. |
| BCA Assay | Copper reduction by peptide bonds in alkaline conditions (biuret reaction) [28] [35]. | Reducing agents (DTT, β-mercaptoethanol) [28], metal chelators (EDTA, EGTA) [28]. | Detergents [28], most salts [35]. |
| Lowry Assay | Copper reduction followed by Folin-Ciocalteu reaction [36] [35]. | Reducing agents, carbohydrates, ammonium ions, Tris buffer [35]. | Most surfactants [28]. |
| UV Absorbance at 280 nm | Absorption by aromatic amino acids (Trp, Tyr, Phe) [36] [35]. | Any UV-absorbing substance, including nucleic acids, nucleotides, and other aromatic compounds [28] [36]. | Volatile buffers that do not absorb at 280 nm [35]. |
Q4: How can I troubleshoot a protein assay that is producing inconsistent results?
A: Inconsistent results often stem from improper sample handling, incorrect standard selection, or unaccounted-for interference. Follow this troubleshooting guide for common issues.
| Problem | Possible Causes | Potential Solutions |
|---|---|---|
| High Background/Inaccurate Reading | Interference from buffer components (detergents, reducing agents) [28]. | • Dialyze or desalt the sample to remove small interfering substances [28]. • Precipitate the protein and re-dissolve it in a compatible buffer [28]. • Switch to a more compatible assay (see Table 2). |
| Poor Standard Curve Linearity | • Improper standard preparation.• Protein-to-protein variation (especially in dye-binding assays) [28] [38]. | • Ensure the standard is prepared in the same buffer as the unknown samples [28]. • Use a purified version of your protein of interest as a standard, if possible. Otherwise, BSA or IgG are common choices [28]. |
| Low Sensitivity | Protein concentration is below the assay's detection limit [38]. | • Concentrate your sample. • Use a more sensitive assay (e.g., switch from Bradford to BCA or a fluorescent assay) [28]. • For very low concentrations, consider a standard addition method to improve accuracy [38]. |
| Overestimation of Target Protein | Using a total protein assay (e.g., BCA) on an impure sample to quantify a specific protein [3]. | • Use a specific assay like ELISA or LC-MS/MS for the target protein [3]. • Employ a purification step before quantification with a general assay. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials essential for performing accurate protein quantification, along with their primary functions.
| Item | Function & Importance |
|---|---|
| Bovine Serum Albumin (BSA) | A widely used reference protein for generating standard curves in colorimetric assays due to its high purity, stability, and low cost [28] [34]. |
| Compatible Lysis Buffers | Buffers for extracting proteins that are free of interfering substances (like strong reducing agents or detergents) specific to the chosen assay, ensuring accurate quantification [28]. |
| Microplate Reader | An instrument for measuring absorbance or fluorescence in plate-based assays, enabling high-throughput analysis of multiple samples simultaneously [28]. |
| Pierce BCA Protein Assay Kit | A commercial kit exemplifying the BCA method, providing pre-formulated reagents for precise, sensitive, and reproducible total protein quantification [38] [39]. |
| 96-Well Plates with Membrane Bottom | Specialized plates used in validated, robust assays for isolating protein-dye complexes, improving reproducibility by enabling reproducible washing steps [34]. |
| Tandem Mass Tags (TMT) | Isobaric labels used in advanced mass spectrometry (e.g., SCoPE-MS) for multiplexed, relative quantification of proteins across different samples, such as single cells [37]. |
| Primary & Secondary Antibodies | Essential reagents for specific quantification assays like ELISA and Western blot, providing the high specificity needed to detect and measure a target protein amidst a complex mixture [3]. |
| Dialysis Cassettes/Columns | Tools for buffer exchange, allowing for the removal of small, interfering substances (e.g., DTT, salts) from protein samples prior to quantification [28]. |
Experimental Protocols & Workflows
Workflow: Selecting and Validating a Protein Quantification Assay
The following diagram outlines a logical workflow for selecting, optimizing, and validating a protein quantification method, crucial for research and regulatory compliance.
Protocol: Direct Quantification of Protein in Liposomes using BCA Assay
This protocol, adapted from [39], is an example of a direct quantification method, which is more accurate than indirect methods that measure un-encapsulated protein.
1. Objective: To directly determine the encapsulation efficiency of a model protein (Ovalbumin, OVA) within liposomal formulations.
2. Materials:
- Pierce Micro BCA Protein Assay Kit
- Liposome samples (neutral, anionic, and cationic)
- Bovine Serum Albumin (BSA) standards
- 96-well plate
- Microplate reader capable of measuring absorbance at 562 nm
3. Methodology: - Standard Curve Preparation: Prepare a series of BSA standards in the same buffer used for the liposome formulations, covering a concentration range of 0-40 µg/mL. - Sample Preparation: Solubilize the liposome samples to release the encapsulated protein. This may involve the use of solubilizing agents that are compatible with the BCA assay. - Assay Procedure: 1. Pipette 150 µL of each standard and unknown sample into the wells of a 96-well plate. 2. Add 150 µL of the working reagent (prepared as per kit instructions) to each well. 3. Cover the plate and incubate at 35-37°C for 2 hours. 4. Measure the absorbance of each well at 562 nm using a microplate reader. - Data Analysis: 1. Generate a standard curve by plotting the average absorbance of the BSA standards against their known concentrations. 2. Use the linear equation from the standard curve to calculate the protein concentration in the unknown liposome samples. 3. Calculate the encapsulation efficiency based on the initial amount of protein used in the formulation.
4. Key Considerations: - The BCA assay can be interfered with by lipids. Using a standard addition method or validating against another technique (e.g., RP-HPLC) is recommended for critical work [39]. - Ensure the solubilization method completely disrupts the liposomes without inhibiting the colorimetric reaction.
Troubleshooting Guides
ELISA Troubleshooting FAQ
Problem: Weak or No Signal
- Q: My ELISA results show a very weak or no signal. What could be the cause?
- A: This is a common issue with several potential causes and solutions [40]:
- Reagents not at room temperature: Ensure all reagents are at room temperature before starting the assay. Allow them to sit on the bench for 15-20 minutes [40].
- Incorrect storage or expired reagents: Double-check that all components have been stored at the recommended conditions (typically 2–8°C) and have not passed their expiration date [40].
- Improper pipetting or dilutions: Verify your pipetting technique and double-check all calculations for reagent dilutions [40].
- Insufficient detector antibody: If developing your own ELISA, you may need to optimize the concentration of the detector antibody. For commercial kits, follow the protocol exactly [40].
- Scratched wells: Use caution when pipetting or washing to avoid scratching the well surface, which can interfere with the assay [40].
Problem: High Background
- Q: The signal in my ELISA is too high, leading to elevated background across all wells. How can I fix this?
- A: High background is often related to washing or incubation steps [40]:
- Insufficient washing: Ensure you are following the washing procedure meticulously. After washing, invert the plate onto absorbent tissue and tap forcefully to remove residual fluid. Increasing the duration of soak steps during washing may also help [40].
- Contamination: Always use a fresh plate sealer during incubations to prevent cross-contamination between wells [40].
- Over-incubation: Adhere strictly to the recommended incubation times. Longer incubations can increase non-specific binding [40].
- Light exposure: Keep the substrate solution protected from light until use, as premature exposure can lead to high background [40].
Problem: Poor Replicate Data
- Q: The results from my replicate wells are inconsistent. What should I check?
- A: Poor reproducibility often stems from technical inconsistencies [40]:
- Washing inconsistency: Automated plate washers should be calibrated to ensure even washing across all wells. Manual washing should be performed consistently in timing and technique [40].
- Plate sealing: Use a fresh sealer each time the plate is covered to prevent evaporation and well-to-well contamination, which can cause variation between replicates [40].
- Coating issues (if coating your own plates): Ensure you are using an appropriate ELISA plate (not a tissue culture plate) and that the coating antibody is properly diluted and incubated [40].
Mass Spectrometry (AQUA) Troubleshooting FAQ
Problem: Low Reproducibility in Biomarker Studies
- Q: My mass spectrometry-based biomarker discovery results lack reproducibility between runs. What are the best practices to improve this?
- A: Reproducibility is critical in MS studies. Key considerations include [41]:
- Experimental Design: Ensure proper cohort selection with sufficient statistical power. Implement strict sample blinding and randomization to avoid bias.
- Sample Preparation: Standardize sample collection, processing, and storage protocols across all samples. Incorporate quality control (QC) samples to monitor instrument performance throughout the run.
- Data Quality Control: Perform rigorous data processing and statistical analysis. Use appropriate algorithms to normalize data and account for technical variation.
Problem: Inaccurate Quantification with AQUA
- Q: I am using AQUA (Absolute QUAntification) peptides, but my quantification seems inaccurate. What are potential sources of error?
- A: While specific AQUA protocols are advanced, general MS quantification challenges include [41]:
- Sample Load Variability: Ensure consistent protein/peptide loading across samples. Use internal standards, like AQUA peptides themselves, to correct for any variations in sample preparation and instrument response.
- Chromatographic Performance: Monitor the liquid chromatography (LC) system for stable retention times and peak shapes. Degradation in LC performance can significantly impact quantification accuracy.
- Instrument Calibration: Regularly calibrate the mass spectrometer according to the manufacturer's specifications to ensure mass accuracy and sensitivity.
Amino Acid Analysis Troubleshooting FAQ
- Q: My amino acid analysis results are inconsistent. What are common pitfalls?
- A: Amino acid analysis can be affected by several factors. While detailed protocols vary, general principles for accuracy include:
- Sample Hydrolysis: Complete and consistent protein hydrolysis is crucial. Standardize temperature, time, and the acid-to-protein ratio during hydrolysis to minimize errors. Incomplete hydrolysis leads to low values, while excessive hydrolysis can destroy certain amino acids.
- Handling of Labile Amino Acids: Certain amino acids (e.g., cysteine, methionine, tryptophan) are susceptible to degradation during hydrolysis. Use protective agents or perform performic acid oxidation before hydrolysis to stabilize them for accurate measurement.
- Derivatization Efficiency: If using a derivatization method, ensure the reaction is complete and reproducible. Inconsistent derivatization will directly lead to inaccurate quantification.
Experimental Protocols & Methodologies
Detailed ELISA Protocol (Indirect Method)
The following protocol outlines the steps for an indirect ELISA, commonly used to detect the presence of antibodies in a sample [42].
- Coating: A known antigen is diluted in a coating buffer (e.g., phosphate-buffered saline or PBS) and added to the wells of a 96-well microplate. The plate is incubated to allow the antigen to adsorb to the plastic surface [42].
- Blocking: After incubation, the solution is discarded, and the wells are washed with a wash buffer (e.g., PBS with Tween) to remove unbound antigen. A blocking buffer (e.g., containing bovine serum albumin or casein) is added to cover any remaining protein-binding sites on the plastic, preventing non-specific binding in later steps [42].
- Sample Addition: The biological sample (e.g., serum, plasma) suspected to contain the antibody is diluted and added to the wells. The plate is incubated again, allowing specific antibodies to bind to the immobilized antigen [42].
- Conjugate Addition: After washing away unbound antibodies, an enzyme-conjugated secondary antibody (the conjugate) is added. This antibody is specific to the primary antibody (e.g., anti-human IgG). The plate is incubated once more [42].
- Substrate Addition: The plate is washed thoroughly to remove unbound conjugate. A substrate solution specific to the enzyme (e.g., TMB for Horseradish Peroxidase/HRP) is added. Enzyme-bound wells will catalyze a reaction, producing a visible color change [42].
- Stop Solution and Reading: The enzyme-substrate reaction is stopped after a defined period (usually 30-60 minutes) by adding an acidic or basic solution (e.g., H₂SO₄ or NaOH). The intensity of the color in each well is measured spectrophotometrically with an ELISA reader at an appropriate wavelength (commonly 450 nm for TMB) [42].
General Workflow for Mass Spectrometry-Based Protein Quantification (e.g., AQUA)
This workflow describes the key stages in a targeted mass spectrometry approach like AQUA for absolute protein quantification.
- Sample Preparation: Proteins are extracted from the biological matrix (e.g., cell lysate, tissue, plasma). The protein mixture is then digested enzymatically (typically with trypsin) to generate a peptide mixture [41].
- Spike-in of Stable Isotope-Labeled Standards: Synthetic, stable isotope-labeled versions of target peptides (AQUA peptides) are added to the sample digest in known amounts. These peptides are chemically identical to the native peptides but have a different mass, allowing the mass spectrometer to distinguish them [41].
- Liquid Chromatography (LC): The peptide mixture is separated by liquid chromatography, which reduces sample complexity and improves detection sensitivity by introducing peptides to the mass spectrometer over time [41].
- Mass Spectrometry Analysis: The eluting peptides are ionized and analyzed by the mass spectrometer. In targeted methods like Selected Reaction Monitoring (SRM) or Parallel Reaction Monitoring (PRM), the instrument is set to specifically monitor the signals of the native and heavy AQUA peptides [41].
- Data Analysis and Quantification: The peak areas or heights for the native peptide and its corresponding AQUA standard are extracted. Since the amount of the AQUA peptide is known, the absolute amount of the native peptide (and thus the original protein) can be calculated directly from the ratio of their signal intensities [41].
Research Reagent Solutions
The following table details essential materials and reagents used in the featured techniques.
| Item | Function/Application | Key Considerations |
|---|---|---|
| 96-well Microplate | Solid-phase matrix for immobilizing antigens or antibodies in ELISA [42]. | Use plates made of polystyrene, polyvinyl, or polypropylene designed for high protein binding [42]. |
| Coating Antibody/Antigen | The capture molecule that is adsorbed to the plate surface to bind the target analyte [42]. | Must be highly pure and specific. Diluted in an appropriate buffer like PBS for coating [40] [42]. |
| Enzyme-Conjugate | An antibody linked to an enzyme (e.g., HRP, AP); binds to the target to enable detection [42]. | The conjugate must be specific (e.g., anti-species IgG). Concentration requires optimization for in-house assays [40] [42]. |
| Chromogenic Substrate | Reacts with the enzyme to produce a measurable color change [42]. | Common substrates include TMB (turns yellow) for HRP. Protect from light. Stop solution required [42]. |
| AQUA Peptides | Synthetic, stable isotope-labeled internal standards for absolute protein quantification by MS [41]. | Must be chemically pure and sequence-identical to the target proteolytic peptide. Spiked-in at a known concentration [41]. |
| Trypsin | Protease used to digest proteins into peptides for mass spectrometry analysis [41]. | Use sequencing-grade trypsin for reproducible and specific cleavage after lysine and arginine residues [41]. |
| LC-MS Grade Solvents | Used for mobile phases in liquid chromatography and sample preparation [41]. | High purity is critical to minimize background noise and ion suppression in the mass spectrometer [41]. |
Common ELISA Problems and Solutions
Table 1: A summary of frequent issues encountered during ELISA development and their recommended solutions [40].
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Weak/No Signal | Reagents not at room temperature | Allow all reagents to equilibrate for 15-20 minutes before the assay [40]. |
| Incorrect storage or expired reagents | Verify storage conditions (often 2-8°C) and check expiration dates [40]. | |
| Insufficient washing | Follow washing procedure meticulously; tap plate forcefully to remove residual fluid [40]. | |
| High Background | Insufficient washing | Increase wash steps or duration; ensure complete drainage between washes [40]. |
| Over-incubation | Adhere strictly to recommended incubation times [40]. | |
| Substrate exposed to light | Store and use substrate in the dark [40]. | |
| Poor Replicate Data | Inconsistent pipetting | Check and calibrate pipettes; ensure proper pipetting technique [40]. |
| Evaporation | Use a fresh plate sealer during all incubations [40]. | |
| Edge Effects | Uneven temperature across plate | Avoid stacking plates; place in the center of the incubator and use a plate sealer [40]. |
Key Market Trends in Protein Detection
Table 2: Analysis of the protein detection and quantification market, highlighting key segments and growth drivers [33].
| Market Segment | Leading Category (2024) | Key Growth Drivers |
|---|---|---|
| By Product | Kits and Reagents/Consumables | High, continuous demand for antibodies, assay kits, and buffers for routine protein analysis like ELISA and Western blotting [33]. |
| By Technology | Colorimetric Assays | Simplicity, cost-effectiveness, and wide applicability, especially in high-throughput formats [33]. |
| By Application | Drug Discovery and Development | Critical role in target identification, biomarker validation, and quality control of biopharmaceuticals [33]. |
| By End User | Biotechnology and Pharmaceutical Companies | Intensive R&D activities for drug discovery, development, and production of protein-based therapeutics [33]. |
| Overall Market | CAGR (2025-2033): 7.5% | Rising demand for personalized medicine, increasing proteomics research, and expansion in biomarker identification [33]. |
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center addresses common challenges in high-throughput screening (HTS) and multiplexed assays, with a specific focus on optimizing protein concentration measurement accuracy. The guides below provide solutions for researchers, scientists, and drug development professionals.
Frequently Asked Questions (FAQs)
1. Our HTS campaign is generating an unusually high rate of false positives. What are the common causes and solutions?
False positives in HTS can significantly derail research progress. The most common causes and their solutions are outlined in the table below.
Table 1: Troubleshooting False Positives in HTS
| Cause of False Positive | Underlying Issue | Recommended Solution |
|---|---|---|
| Assay Interference [43] | Chemical reactivity or compound autofluorescence interfering with the detection signal. | Implement counter-screen assays or use orthogonal detection methods (e.g., switch from fluorescence to mass spectrometry) [43]. |
| Compound-Related Issues [43] | Colloidal aggregation or metal impurities in the compound library. | Use chelating agents or detergent-based assays to disrupt aggregates. Apply computational filters (e.g., pan-assay interference compounds, or PAINS, filters) to pre-screen compound libraries [43]. |
| Data Quality Issues [43] | Measurement uncertainty or systematic errors from equipment. | Implement robust statistical quality control (QC) methods for outlier detection and normalize data using internal controls (e.g., Z'-factor calculation) [43]. |
2. What is the most accurate method for quantifying protein concentration in a complex buffer solution?
No single method is a universal "gold standard" due to the diverse physicochemical properties of different proteins and their buffers. The optimal choice depends on your specific context [1].
Table 2: Selecting a Protein Quantification Assay
| Assay Method | Key Principle | Tolerance for Buffer Components | Best for Protein Concentration Research Because... |
|---|---|---|---|
| Amido Black [1] | Protein binds to a dye, which is then measured. | High tolerance for detergents, salts, and reducing agents. | Its robustness in complex matrices (e.g., drug formulations) makes it reliable for difficult samples, though it is less common [1]. |
| Amino Acid Analysis (AAA) [1] | Hydrolyzes protein and quantifies individual amino acids. | Generally high, but buffer must be analyzed as a negative control. | It provides highly reproducible and absolute quantification, making it excellent for release testing of clinical materials [1]. |
| BCA / Lowry [1] | Colorimetric reaction based on protein-copper chelation. | Varies; can be disrupted by specific buffer components. | It offers high sensitivity and is well-suited for the low quantities and purities typical in early drug discovery [1]. |
| ELISA [1] | Antibody-based antigen detection. | High, as the antibody provides specificity. | It quantifies the drug substance specifically, even in a mixture of other proteins (e.g., host cell proteins), which is crucial for accurate dosing [1]. |
3. How can AI be integrated into our existing HTS workflow to improve efficiency?
Integrating AI with HTS creates a synergistic, iterative discovery cycle [44]. The workflow below illustrates this closed-loop process.
Diagram 1: AI-HTS Integrated Workflow
This integrated approach has been shown to reduce hit-to-lead cycle times by up to 65% and identify novel chemotypes with nanomolar potency [44].
4. We are considering Ultra-HTS (uHTS). What are the key technological challenges we should anticipate?
While uHTS (screening >300,000 compounds per day) offers immense throughput, it introduces specific challenges compared to standard HTS [43].
Table 3: HTS vs. uHTS Key Challenges
| Attribute | HTS | uHTS | Technical Challenge in uHTS |
|---|---|---|---|
| Throughput | ~100,000 assays/day [43] | >300,000 assays/day [43] | Requires advanced microfluidics and high-density microwell plates (1-2 µL volumes) [43]. |
| Liquid Handling | Complex, but manageable with automation. | Extremely complex. | Precise fluid handling at nanoliter scales is a significant impediment to widespread uptake [43]. |
| Multiplexing Capability | Limited. | Highly desired. | Standard HTS biosensors are often restricted to one analyte. There is a need for miniaturized, multiplexed sensor systems for continuous monitoring of multiple parameters (e.g., pH, O₂) [43]. |
| Data Management | High volume. | Massive volume. | Requires sophisticated cheminformatics platforms (e.g., LIMS) and potentially AI to process the immense datasets generated [43]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and materials essential for successful HTS and accurate protein quantification experiments.
Table 4: Essential Research Reagent Solutions
| Item | Function & Application in HTS/Protein Work |
|---|---|
| Validated Protein Quantification Assays | Kits (e.g., BCA, Lowry) for determining total protein content. Critical for normalizing assays and ensuring consistent drug dosing in development [1]. |
| Primary Reference Standards | Highly characterized standards (e.g., from NIST) used to calibrate in-house reference standards. Essential for ensuring the accuracy and reproducibility of quantitative methods [1]. |
| Validated Antibodies (for ELISA) | Antibodies with confirmed specificity for the target protein. Necessary for developing specific, sensitive, and quantitative assays for a drug substance in a complex mixture [1]. |
| HTS-Optimized Assay Kits | Robust, miniaturized, and validated assay kits for specific targets (e.g., kinases, phosphatases). Enable rapid screening in 384- or 1536-well formats with high reproducibility [43]. |
| AI/ML Data Analysis Platforms | Software that uses machine learning models to triage HTS output, rank compounds by probability of success, and identify pan-assay interferents, thereby reducing false positives [43]. |
Advanced Troubleshooting and Practical Optimization of Protein Assays
FAQs: Troubleshooting Protein Assays
This section addresses frequently encountered issues in protein quantification assays, such as the Bradford and BCA assays, providing targeted solutions to improve data accuracy.
Q1: Why do my protein samples show low absorbance in a Bradford assay?
Low absorbance can stem from several factors related to your sample or reagents [10].
- Cause: Protein Size. The Bradford assay has a detection limit for proteins below 3,000-5,000 Daltons [10].
- Solution: For small proteins or peptides, use an alternative quantification method like the BCA assay [10].
- Cause: Interfering Substances. Substances in your sample buffer, such as detergents, can inhibit the color change reaction [12] [10].
- Cause: Reagent Quality. The Bradford reagent may be old, expired, or stored incorrectly [10].
- Solution: Use fresh reagent that has been stored at 4°C and ensure it is brought to room temperature before use [10].
Q2: What causes high background in my experiment, and how can I reduce it?
High background is a common issue across techniques like Western blotting, immunohistochemistry (IHC), and ELISA. The underlying cause is often non-specific binding, which can be mitigated through several strategies [45] [46] [47].
- Cause: Inadequate Blocking. The membrane or tissue was not sufficiently blocked to prevent non-specific antibody binding.
- Cause: High Antibody Concentration. Using too high a concentration of primary or secondary antibody accelerates non-specific binding [45] [48].
- Cause: Inadequate Washing. Unbound antibodies remain on the membrane or tissue.
- Cause: Active Endogenous Enzymes. In IHC, endogenous peroxidases or phosphatases can react with the substrate.
- Solution: Prior to immunostaining, block endogenous enzymes with inhibitors like hydrogen peroxide (for HRP) or levamisol (for alkaline phosphatase) [45].
Q3: Why are there precipitates in my Bradford assay sample?
Precipitates typically indicate a reaction between the assay reagent and components in your sample [10].
- Cause: Detergents. High concentrations of detergents in the protein buffer can cause precipitation [10].
- Solution: Dialyze the sample to remove the detergents, or dilute the sample to a point where the detergent concentration no longer interferes [10].
Quantitative Data Tables
Table 1: Protein Assay Compatibility with Common Substances
The following table summarizes the maximum compatible concentrations of various substances in different protein assays. A substance is considered compatible if it causes an error in protein estimation of ≤10% [12].
| Substance | BCA & Micro BCA Assay | Pierce Bradford Assay | Modified Lowry Assay |
|---|---|---|---|
| Reducing Agents (e.g., DTT) | Not compatible [12] | Compatible (see manufacturer's table) [12] | Not compatible [12] |
| Chelators (e.g., EDTA) | Not compatible [12] | Compatible (see manufacturer's table) [12] | Not compatible [12] |
| Ionic Detergents (e.g., SDS) | Compatible (see manufacturer's table) [12] | Not compatible [12] | Not compatible [12] |
| Non-Ionic Detergents (e.g., Triton X-100) | Compatible (see manufacturer's table) [12] | Compatible (see manufacturer's table) [12] | Compatible (see manufacturer's table) [12] |
| Strong Acids/Bases | Not compatible [12] | Varies; alkalinity can cause dark blue color [12] [10] | Varies [12] |
Table 2: Troubleshooting Low Absorbance & High Background
This table provides a quick-reference guide for diagnosing and resolving common assay problems.
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low Absorbance | Protein too small for assay | Switch to a more sensitive assay (e.g., BCA for small proteins) [10]. |
| Interfering substances in sample | Dilute, dialyze, or desalt the sample [12] [10]. | |
| Incorrect wavelength | Verify measurement at the correct wavelength (e.g., 595 nm for Bradford) [10]. | |
| High Background | Insufficient blocking | Optimize blocking buffer concentration and incubation time [45] [46] [48]. |
| Antibody concentration too high | Titrate both primary and secondary antibodies [45] [48]. | |
| Inadequate washing | Increase wash duration, volume, and detergent concentration [45] [48]. | |
| Precipitates | Detergents in sample buffer | Dialyze or dilute the sample to reduce detergent concentration [10]. |
Experimental Workflows
Workflow 1: Systematic Troubleshooting for Protein Assay Anomalies
The diagram below outlines a logical pathway for diagnosing and addressing common protein assay issues.
Research Reagent Solutions
This table details key reagents used to prevent and resolve the issues discussed in this guide.
| Reagent | Function in Troubleshooting | Example Application |
|---|---|---|
| BCA Assay Kit | Accurate quantification of small proteins/peptides where Bradford assay fails [10]. | Replacing Bradford assay for proteins < 5 kDa [10]. |
| BSA (Bovine Serum Albumin) | A universal blocking agent and protein standard; ideal for blocking when detecting phosphoproteins [48]. | Preparing standard curves; used in blocking buffers for Western blots [48]. |
| Normal Serum | Blocking agent used in IHC to reduce non-specific binding of secondary antibodies [45]. | Blocking tissue sections prior to primary antibody incubation [45]. |
| Hydrogen Peroxide | Blocks endogenous peroxidase activity in tissues to reduce high background in IHC [45]. | Pre-treatment of tissue sections before HRP-conjugated antibody is applied [45]. |
| Tween 20 | A non-ionic detergent added to wash buffers to reduce non-specific binding and lower background [48]. | Adding to TBST buffer (e.g., 0.05%-0.1%) for washing Western blot membranes [48]. |
| Dialysis Kit | Removes small molecule interfering substances (e.g., detergents, reducing agents) from protein samples [12] [10]. | Desalting or buffer exchange to prepare samples for a Bradford assay [12]. |
Accurate protein concentration measurement is a cornerstone of reproducible research and robust drug development. The sensitivity of these assays is not inherent to the kit alone; it is highly dependent on the meticulous optimization of physical parameters and reagent components. This guide provides targeted troubleshooting and FAQs to help researchers systematically enhance assay performance by adjusting reagent ratios and well volumes, thereby improving the accuracy and reliability of protein quantification.
Core Concepts of Assay Optimization
The sensitivity of an assay is a measure of its ability to reliably distinguish a target signal from background noise. Key statistical parameters define this quality:
- Z'-Factor: A statistical metric for assessing the quality of high-throughput screens. A Z' > 0.5 indicates an excellent assay, while a value below 0.4 suggests required optimization [49].
- Signal-to-Background (S/B) Ratio: Ensures clear differentiation between positive and negative controls [49].
- Coefficient of Variation (CV %): Low CV values (<10%) indicate consistent performance across wells [49].
Optimization involves systematically tuning variables to improve these parameters, directly impacting the cost, speed, and success of your research.
Systematic Optimization Approaches
Optimizing Well Volumes and Plate Geometry
The physical dimensions of your assay platform fundamentally influence liquid handling accuracy.
Standard 96-Well Plate Specifications and Applications [50]:
| Plate / Well Type | Typical Capacity (µL) | Common Working Volume (µL) | Ideal Application |
|---|---|---|---|
| U-Bottom | ~270 µL | 50-200 µL | Cell culture, storage (minimizes residual liquid) |
| F-Bottom | ~350 µL | 50-200 µL | Standard assays (ELISA, absorbance) |
| Deep-Well | Up to 2 mL | Varies | Sample storage, reagent preparation |
| Strip Plates | 350-400 µL | 50-200 µL | Staggered workflows, flexible processing |
Key Considerations:
- Meniscus Level: Consistent volumes across wells ensure uniform meniscus levels, which is critical for reducing evaporation-related errors and ensuring data accuracy [50].
- Well Shape: Round-bottom wells minimize residual liquid and are ideal for mixing or storage, while flat-bottom wells provide uniform optical clarity for absorbance readings [50].
- Miniaturization: Reducing assay volumes (e.g., from 50µL to 10µL) saves reagents but requires careful validation to ensure no loss of Z'-factor or signal uniformity [49].
Fine-Tuning Reagent Ratios and Concentrations
The concentration and ratio of your assay components dictate the biochemical window for detection.
Key Parameters to Optimize [49]:
- Enzyme and Substrate Concentration: Perform a matrix experiment (enzyme titration × substrate titration) to find the combination that yields a clear signal response with linear kinetics. Aim for a low substrate turnover (5-10%) during detection to avoid depletion [49].
- Antibody Concentration: Titrate both capture and detection antibodies to find the optimal working concentration that maximizes specific signal while minimizing background [51].
- Signal Reagents: The concentration of components like streptavidin-HRP should be checked and titrated to prevent excessively high signals that can obscure data [52].
Critical Steps: Washing and Detection
Plate Washing Optimization [53]: Inadequate washing is a primary cause of high background. Parameters must be balanced to remove unbound molecules without stripping specifically bound ones.
| Parameter | Typical Setting | Optimization Impact |
|---|---|---|
| Wash Volume | 200-300 µL | Too little: high background. Too much: risk of losing signal. |
| Number of Cycles | 3 cycles | Too few: high background. Too many: reduced signal strength. |
| Soak Time | 0-30 seconds | Adding a soak step between washes can improve stringency. |
| Aspiration | Precise calibration | Critical for minimizing residual volume; floating aspiration heads are more forgiving. |
Detector Gain Setting [54]: For fluorescence and luminescence assays, the microplate reader's gain (signal amplification) is crucial.
- Too High: Causes detector saturation, clipping data at the high end.
- Too Low: Dim signals become indistinguishable from background noise, raising the limit of detection.
- Best Practice: Use the reader's automatic gain adjustment on the well with the brightest expected signal, targeting 90% of the detector's maximum range [54].
Troubleshooting Guides
Troubleshooting Common Assay Problems
| Problem & Symptom | Possible Root Cause | Corrective Action |
|---|---|---|
| High Background Signal | Insufficient washing [52] [53]. | Increase wash cycles/volume; add a soak step [52] [53]. |
| Ineffective blocking [51]. | Try a different blocking buffer (e.g., BSA, serum) [51]. | |
| Detection reagent concentration too high [51]. | Titrate detection antibody/streptavidin-HRP to optimal dilution [51]. | |
| Low or No Signal | Key reagent omitted or inactivated [52]. | Verify all reagent additions; ensure avidin-HRP is added [52]. |
| Enzyme activity inhibited (e.g., by sodium azide) [51]. | Use azide-free buffers for all steps prior to detection [51]. | |
| Target concentration below detection limit [52]. | Concentrate sample or decrease dilution factor [52]. | |
| High Variation (Poor Duplicates) | Pipetting inconsistency [51]. | Calibrate pipettes; ensure tips are sealed; mix samples thoroughly [51]. |
| Edge effects (evaporation in perimeter wells) [49]. | Use humidity control; avoid using outer wells; use plate sealers [49] [52]. | |
| Inadequate washing or well drying [52]. | Ensure uniform washing; do not let wells dry out during incubations [52]. | |
| Poor Z'-Factor (< 0.5) | Low signal-to-background ratio [49]. | Titrate reagents to improve dynamic range; reduce background noise [49]. |
| High well-to-well variability [49]. | Check pipette calibration; use automation; control for evaporation [49]. |
Frequently Asked Questions (FAQs)
1. Can I modify the manufacturer's ELISA protocol to increase sensitivity? Yes, protocols can often be modified. You can adjust sample volume, incubation times, and use sequential reagent addition schemes to enhance sensitivity. However, any modification must be thoroughly qualified to ensure it achieves acceptable accuracy, specificity, and precision for your specific application [55].
2. How much can I reduce my assay volume to save reagents? Miniaturization is possible but requires validation. When reducing volumes (e.g., from 50µL to 10µL in a 384-well plate), you must retest signal uniformity and Z'-factor to ensure no performance loss has occurred. The key is maintaining a consistent meniscus level and ensuring homogeneous mixing [49] [50].
3. What is the single most important step for reducing high background? Thorough and consistent washing is paramount. Ensure you are using the recommended wash volume and number of cycles. After washing, invert the plate and tap it forcefully onto absorbent tissue to remove any residual fluid. Automating this process with a plate washer can greatly improve reproducibility [52] [53].
4. Why should I measure "active concentration" instead of total protein? Traditional methods (e.g., A280, BCA) measure total protein but cannot distinguish the functionally active portion from misfolded or denatured protein. Calibration-free concentration analysis (CFCA) using SPR technology specifically quantifies the active protein, which is critical for understanding true reagent potency and reducing lot-to-lot variability [56].
5. How do I know if my microplate reader settings are optimal? For fluorescence and luminescence, the gain setting is critical. If your highest standard is maxing out the detector, the gain is too high. If your blank and low standards are indistinguishable, the gain is too low. Perform a gain adjustment on your brightest sample to set the optimal amplification [54].
Experimental Workflow and Relationships
The following diagram illustrates the logical workflow and key parameter relationships for systematic assay optimization.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function & Role in Optimization |
|---|---|
| Universal Detection Assays (e.g., Transcreener) | Detects universal nucleotides (ADP, GDP); simplifies optimization across diverse enzyme targets by reducing variables from coupled enzyme systems [49]. |
| Low-Bind Pipette Tips | Minimizes adsorption of precious proteins and enzymes to plastic surfaces, ensuring accurate reagent delivery and reducing sample loss [50]. |
| Calibration-Free Concentration Analysis (CFCA) | An SPR-based method that quantifies the active concentration of a protein reagent, not just the total protein, crucial for normalizing activity and reducing lot-to-lot variability [56]. |
| Assay Quality Controls | In-house controls (low, medium, high) prepared in your sample matrix are the most sensitive tool for monitoring run-to-run and lot-to-lot assay performance [55]. |
| Automated Plate Washer | Provides consistent, reproducible washing across all wells, which is critical for minimizing background and well-to-well variation [53]. |
Troubleshooting Guides
How do I know if my buffer is interfering with my protein concentration assay?
Buffer interference is a common problem that causes inaccurate protein quantification. The table below summarizes the key signs of interference for different assay types.
Table 1: Common Signs of Buffer Interference in Protein Assays
| Assay Type | Signs of Interference |
|---|---|
| Bradford Assay | Sample color turns dark blue unexpectedly; precipitate forms; low or high absorbance readings compared to standards [10]. |
| BCA Assay | Unusually high or low color development; poor standard curve fit; results are inconsistent with sample dilution [2]. |
| UV-Vis at A280 | Absorbance reading is excessively high even after buffer blanking; non-linear dilution response, suggesting contamination from absorbing substances [2]. |
| General | Poor spike-and-recovery results; significant discrepancy in concentration values when using different assay methods [1]. |
What are the most common buffer components that cause interference?
Many standard buffer additives can disrupt protein-dye interactions or produce signals that mask the true protein concentration.
Table 2: Common Interfering Substances and Their Effects
| Interfering Substance | Effect on Bradford Assay | Effect on BCA Assay | Effect on UV A280 |
|---|---|---|---|
| Detergents (SDS, Triton X-100, Tween) | Strong interference; can cause precipitation [10] [2]. | Compatible at low concentrations [2]. | Strong interference [2]. |
| Reducing Agents (DTT, β-mercaptoethanol) | Generally compatible [2]. | Interferes by reducing Cu²⁺ [2]. | Interferes [2]. |
| Salts (Ammonium Sulphate) | High concentrations can interfere [10]. | High concentrations can interfere; ammonia is a strong interferent [2]. | Generally low interference. |
| Biological Buffers (Tris, EDTA) | Interferes, especially at high concentrations [2]. | Compatible at low concentrations [2]. | Interferes [2]. |
| Sugars | High concentrations can raise alkalinity, causing interference [10]. | Information not specified in results. | Information not specified in results. |
My Bradford assay shows high background. Is this a buffer problem?
High background, or non-specific binding, can indeed stem from buffer-related issues, but other factors are also common. To troubleshoot, ensure your washing technique during ELISA-based protocols is thorough to prevent reagent carryover, and confirm you are using the correct wash solution without added detergents that can increase background [57]. Buffer components in your sample can sometimes contribute to high background, and dilution of the sample may help reduce this interference [57]. Finally, rule out contamination of your assay reagents or substrate from concentrated protein sources or environmental factors in the lab [57].
Frequently Asked Questions (FAQs)
When should I choose dilution over dialysis or precipitation?
The choice depends on your protein concentration, the nature and concentration of the interferent, and your required throughput.
- Choose Dilution When: Your protein concentration is high enough to withstand dilution below the interferent's threshold, and the interferent is a known, dilutable substance like a salt or detergent [10] [57]. This is the simplest and fastest method.
- Choose Dialysis or Desalting When: The interfering small molecules need to be completely removed, and your sample volume is manageable. This is ideal for buffer exchange or desalting before sensitive downstream applications [58].
- Choose Precipitation When: The interferent is incompatible with other methods (e.g., detergents), your protein is at a very low concentration, or you need to concentrate your sample simultaneously [58].
I am dealing with a cellulase-containing sample. Can I use standard dialysis?
No, you should avoid standard cellulose-based dialysis tubing. Cellulase enzymes will digest the cellulose membrane, creating perforations and leading to a complete loss of your sample [59]. Instead, use alternative methods such as gel filtration (desalting) chromatography with polyacrylamide-based resins (e.g., Biogel-P) [59] or diafiltration devices that use non-cellulosic membranes [58].
How do I validate that my interference problem has been solved?
After applying a cleanup protocol, perform a spike-and-recovery experiment to validate your results [57].
- Spike: Take a portion of your cleaned sample and add a known concentration of a standard protein (e.g., BSA).
- Measure: Measure the protein concentration of the spiked sample.
- Calculate Recovery: Calculate the percentage recovery:
(Measured concentration - Original cleaned sample concentration) / (Concentration of spike added) * 100%. - Interpret: A recovery of 95-105% is generally considered excellent and indicates that the interference has been successfully removed [57]. Consistently low or high recoveries suggest residual interference or issues with the cleanup method itself.
Experimental Protocols
Protocol 1: Rapid Desalting and Buffer Exchange Using Spin Columns
This protocol uses size exclusion chromatography to separate proteins from small molecules, ideal for removing salts, detergents, and other small interferents [58].
Workflow: Rapid Desalting via Spin Column
Materials:
- Spin Desalting Column: Choose a column with appropriate MWCO and bed volume for your sample (e.g., Zeba Spin Columns, GE PD-10) [58].
- Target Buffer: The buffer you want to exchange your sample into (e.g., PBS).
- Microcentrifuge.
Step-by-Step Method:
- Preparation: Pre-equilibrate the spin column by centrifuging it with the target buffer or water, as per the manufacturer's instructions. This removes the storage solution [58].
- Application: Carefully load your protein sample onto the center of the compacted resin bed. Do not disturb the bed.
- Elution: Place the column in a clean collection tube and centrifuge at the recommended speed and time. The macromolecules pass through quickly, while small molecules are retained in the resin pores [58].
- Recovery: The flow-through contains your protein in the new, interference-free buffer. Proceed with protein quantification.
Protocol 2: Protein Precipitation for Interferent Removal
Precipitation effectively separates proteins from contaminants like detergents and lipids by using agents such as TCA or acetone to pellet the protein [58].
Workflow: Protein Precipitation
Materials:
- Precipitation Reagent: Trichloroacetic acid (TCA) or chilled acetone.
- Solvent for Washing: Chilled acetone or ethanol.
- Compatible Resuspension Buffer: A buffer known not to interfere with your downstream assay.
Step-by-Step Method:
- Precipitation: Add a volume of chilled 100% TCA to your protein sample for a final concentration of 10-20%. Vortex and incubate on ice for 30 minutes. A protein precipitate will form.
- Pelletting: Centrifuge at high speed (e.g., >12,000 × g) for 10-15 minutes at 4°C. The protein will form a tight pellet.
- Washing: Carefully decant the supernatant. Wash the pellet with 1 mL of chilled acetone or ethanol to remove residual TCA and contaminants. Centrifuge again and decant.
- Drying and Resolubilization: Air-dry the pellet for 5-10 minutes to evaporate residual solvent. Do not over-dry, as this will make resolubilization difficult. Resuspend the protein pellet in an appropriate, assay-compatible buffer [58].
Protocol 3: Dialysis for Large-Volume Buffer Exchange
Dialysis separates small molecules from macromolecules by selective diffusion across a semi-permeable membrane, suitable for large sample volumes or gentle buffer exchange over several hours [58].
Workflow: Standard Dialysis
Materials:
- Dialysis Membrane or Cassette: Choose a Molecular Weight Cut-Off (MWCO) 2-3 times smaller than your protein's molecular weight [58].
- Dialysate Buffer: A large volume (200-500 times the sample volume) of the target buffer [58].
Step-by-Step Method:
- Membrane Preparation: If using regenerated cellulose tubing, prepare it by boiling and rinsing according to the manufacturer's instructions.
- Loading: Seal one end of the tubing or cassette, pipette your protein sample into it, and seal the other end.
- Dialysis: Immerse the sealed dialysis device in a large volume of dialysate buffer. Stir gently on a magnetic stirrer in a cold room (4°C) for several hours or overnight.
- Buffer Exchange: Replace the dialysate buffer with fresh buffer at least once or twice to ensure complete removal of small-molecule contaminants.
- Recovery: Carefully recover the dialyzed sample from the membrane for analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Overcoming Buffer Interference
| Item | Function | Key Considerations |
|---|---|---|
| Spin Desalting Columns (e.g., Zeba, PD-10) | Rapid buffer exchange and desalting. High protein recovery, minimal dilution. Ideal for small volumes (μL to mL) [58]. | Check resin capacity and MWCO. Pre-equilibrate with target buffer. |
| Dialysis Cassettes (e.g., Slide-A-Lyzer) | Gentle buffer exchange for larger volumes via semi-permeable membrane [58]. | Choose correct MWCO. Avoid with cellulase-containing samples [59]. Use large dialysate volumes. |
| Protein Concentrators | Concentrate dilute samples and perform diafiltration via centrifugation [58]. | Select appropriate MWCO and sample volume capacity. |
| Precipitation Kits (e.g., Compat-Able) | Remove interfering substances via TCA/acetone precipitation. Kits provide standardized, consistent reagents [58]. | Can be time-consuming. Some proteins may not resolubilize efficiently. |
| Assay-Specific Diluent | A standardized matrix for diluting samples to minimize matrix effects during analysis [57]. | Using a mismatched diluent can cause significant errors in quantification. |
Decision Workflow for Selecting an Interference Mitigation Strategy
The following diagram provides a logical pathway to select the most appropriate protocol based on your sample characteristics and experimental goals.
Workflow: Selecting an Interference Mitigation Method
The Standard Addition Method for Accurate Low-Concentration Measurement
The Standard Addition Method (SAM) is a robust quantitative analysis technique used to determine the concentration of an analyte in a complex sample. Its primary strength lies in its ability to compensate for matrix effects, where other substances in the sample interfere with the measurement of the target analyte, leading to inaccurate results [60] [61] [62].
Unlike conventional calibration curves prepared in a pure solvent, the standard addition method involves adding known quantities of the analyte to the sample itself. This ensures that all measured solutions contain the same matrix, thereby canceling out the effect of interferences on the analytical signal [60]. This guide details the implementation, troubleshooting, and application of SAM, with a specific focus on challenges in protein research and drug development.
How Standard Addition Works: Core Principle
The fundamental principle of SAM is based on the idea that the matrix affects all solutions equally. By adding varying, known amounts of the standard to aliquots of the sample, the resulting calibration curve is constructed within the sample's native matrix [61] [62].
The data is processed through linear regression. The key to finding the original unknown concentration is to determine the x-intercept of the regression line. The line is extrapolated to where it crosses the x-axis (i.e., where the signal, y, is zero). The absolute value of this x-intercept gives the concentration of the unknown analyte in the original sample [60]. The confidence interval for the x-intercept provides the confidence interval for the unknown concentration [60].
The following diagram illustrates the workflow and key logical relationships in the Standard Addition Method.
Experimental Protocol: A Step-by-Step Guide
This protocol outlines the general procedure for implementing the Standard Addition Method, which can be adapted for various analytical techniques.
Materials and Reagents
- Sample: The unknown solution containing the analyte of interest.
- Standard Solution: A certified reference material or a solution of the pure analyte at a accurately known concentration.
- Matrix-matched blank (if available): The sample matrix without the analyte, useful for verifying method performance.
- Appropriate solvents and buffers: For dilution and ensuring compatibility with the analytical instrument.
Procedure
- Sample Aliquoting: Precisely divide a known volume or mass of the sample into at least four or five separate vials. Using more aliquots improves the statistical reliability of the linear regression [62].
- Standard Spiking: To all but one of the aliquots, add known and varying volumes of the standard solution. One aliquot should be left unspiked (this is the "zero" addition point). Ensure the added volumes are small enough to not significantly dilute the sample matrix.
- Dilution to Volume: If necessary, dilute all aliquots to the same final volume with an appropriate solvent to ensure all samples have identical physical properties during analysis.
- Instrumental Analysis: Measure the analytical signal (e.g., absorbance, intensity, peak area) for each prepared aliquot using your chosen instrument (e.g., UV-Vis, ICP, HPLC).
- Data Analysis: Plot the measured signal (y-axis) against the concentration (or absolute amount) of the standard added (x-axis). Perform a linear regression analysis. The concentration of the unknown is the absolute value of the x-intercept, as described in the previous section [60].
Troubleshooting Guide: Common Issues and Solutions
| Problem | Possible Cause | Solution |
|---|---|---|
| Non-linear calibration plot | Saturation of the detector or analytical technique at high concentrations. | Use a wider range of standard additions and ensure measurements are within the instrument's linear dynamic range. |
| Chemical interactions in the matrix at higher concentrations. | Dilute the sample and standard additions to minimize complex matrix interactions. | |
| High variability in data points (poor R² value) | Inconsistent sample preparation or pipetting errors. | Use calibrated pipettes and meticulous technique. Increase the number of replicate aliquots. |
| Instrument instability. | Ensure the instrument is properly calibrated and stable before analysis. | |
| Negative x-intercept calculated | Incorrect assignment of the x-axis values. | Verify that the x-axis represents the concentration/amount of standard added, not the total concentration in the solution. |
| Presence of the analyte in the reagents or solvent used for dilution. | Run a method blank to check for contamination. Use high-purity solvents and reagents. | |
| Insufficient sample volume for multiple aliquots | Standard protocol requires significant sample. | Use a simplified two-point standard addition (unspiked and one spiked sample) if validated for the method [62]. |
Frequently Asked Questions (FAQs)
Q1: When should I use the Standard Addition Method over a conventional calibration curve? A: Use SAM when you cannot obtain a blank matrix, when the sample matrix is complex and causes significant interference (matrix effects), or when you need the highest possible accuracy for a specific sample [60] [62]. This is common in analyzing biological fluids, food products, and environmental samples.
Q2: Can I spike the standard after sample extraction to save time? A: Possibly. If you can demonstrate during method validation that spiking the extract (post-processing) gives equivalent results to spiking before extraction, it can significantly reduce workload [62]. However, spiking before extraction is generally more reliable as it accounts for matrix effects on the extraction efficiency itself.
Q3: What is the minimum number of spiked aliquots needed? A: While a single unspiked and a single spiked aliquot can be used, it is statistically more reliable to use multiple additions (e.g., 4-5) to establish a proper linear regression [62]. A two-point approach should be thoroughly validated to prove accuracy and precision.
Q4: How does Standard Addition relate to protein quantification specifically? A: In protein research, matrix effects from buffers, detergents, or other biomolecules can skew results from methods like UV-Vis (A280), Bradford, or BCA assays [63]. SAM can correct for these interferences. Furthermore, methods like Calibration-Free Concentration Analysis (CFCA) represent a specialized, label-free form of standard addition using SPR biosensors to measure active protein concentration, overcoming issues of lot-to-lot variability in recombinant proteins [56] [64].
Research Reagent Solutions for Protein Measurement
The following table details key reagents and materials used in the field of accurate protein quantification, including both traditional and advanced methods.
| Item | Function & Application |
|---|---|
| Certified Reference Material (CRM) | A high-purity substance with a certified concentration, used as the primary standard in SAM and other methods to ensure traceability and accuracy [65]. |
| Bicinchoninic Acid (BCA) Assay Reagents | A colorimetric method for total protein quantification based on the reduction of Cu²⁺ to Cu⁺ by peptide bonds; compatible with detergents but interfered with by reducing agents [63]. |
| Coomassie Brilliant Blue Dye (Bradford Assay) | A dye that binds to arginine and aromatic residues, causing a color change for total protein estimation; quick and easy but sensitive to protein sequence and detergents [63]. |
| Surface Plasmon Resonance (SPR) Chip | A sensor surface (often gold) used in instruments for CFCA. It enables label-free, real-time measurement of binding interactions to determine active protein concentration [56] [64]. |
| Electrospray Differential Mobility Analyzer (ES-DMA) | An instrument used in a potential primary method for protein quantification, measuring the hydrodynamic volume of proteins in solution, which can be correlated to concentration [65]. |
Comparison of Protein Quantification Methods
Choosing the right quantification method is critical for research reproducibility. The table below summarizes common techniques and their suitability for different scenarios.
| Method | What It Measures | Key Advantages | Key Limitations & Interferences |
|---|---|---|---|
| UV-Vis (A280) | Total protein via aromatic residues (Tyr, Trp) | Quick, no special reagents needed, non-destructive. | Interference from nucleic acids, buffers; requires known extinction coefficient [63]. |
| Bradford Assay | Total protein via dye binding (Arg, aromatics) | Fast, stable signal, not affected by reducing agents. | Variable response between proteins; interfered with by detergents [63]. |
| BCA Assay | Total protein via Cu⁺ reduction (peptide bonds) | More uniform response than Bradford, compatible with detergents. | Interference from reducing agents (e.g., DTT), requires incubation [63]. |
| Kjeldahl Method | Total nitrogen content | Highly precise and reproducible for total protein in foods/soils. | Measures non-protein N, requires large sample, destructive and tedious [63]. |
| Standard Addition (SAM) | Analyte concentration in complex matrices | Corrects for matrix effects, high accuracy for specific samples. | More labor-intensive, requires more sample than direct calibration [60] [62]. |
| Calibration-Free Concentration Analysis (CFCA) | Active protein concentration via SPR | Measures only functional protein, reduces lot-to-lot variability, no calibration curve needed. | Requires specialized SPR instrumentation, knowledge of diffusion coefficient [56] [64]. |
Best Practices for Pipetting, Standard Preparation, and Instrument Use
This technical support center provides targeted troubleshooting guides and FAQs to help researchers optimize the accuracy of protein concentration measurements. The following sections address specific issues encountered during experiments, from pipetting and sample preparation to instrument calibration.
Pipetting Technique and Troubleshooting
Frequently Asked Questions
Q1: My pipetted volumes are inconsistent, especially with small volumes. What is the most critical factor to check?
A1: Inconsistent volumes are often due to technique or equipment issues. First, ensure you are using a pipette whose volume range is appropriate for your target volume; accuracy decreases dramatically when operating near the pipette's minimum volume [66]. Second, master the two-stop pipetting technique: press the plunger to the first stop when aspirating, and to the second stop when dispensing to ensure the entire volume is expelled [66]. Finally, use high-quality tips that form a perfect seal with your pipette barrel to prevent air leaks [67].
Q2: How does sample temperature affect pipetting accuracy, and how can I mitigate this?
A2: Temperature differences between your pipette, tips, and liquids cause the air cushion inside an air-displacement pipette to expand or contract, leading to significant volume inaccuracies [67] [68] [69]. A best practice is to allow all liquids and equipment to equilibrate to the ambient temperature of your lab before starting [68]. Furthermore, for critical measurements, incorporate a pre-wetting step—aspirating and dispensing the liquid at least three times before the actual transfer—to saturate the air cushion and reduce evaporation [68] [69].
Q3: What is the best pipetting method for viscous samples like protein concentrates or glycerol solutions?
A3: For viscous liquids, the standard forward pipetting mode often leads to under-delivery. Instead, use the reverse pipetting technique [68] [69]. In this mode, you depress the plunger to the second stop first, aspirate the liquid, and then dispense by pressing only to the first stop. This leaves an excess volume in the tip, which is accounted for and ensures the accurate dispensing of the desired volume [67]. Using wide-bore or low-retention tips can also aid in the smooth transfer of viscous samples [67].
Common Pipetting Errors and Solutions
Table 1: Summary of common pipetting errors and their solutions.
| Error | Impact on Accuracy | Preventive Solution |
|---|---|---|
| Ignoring temperature [67] | Volume variations due to air cushion expansion/contraction. | Pre-wet tips; equilibrate all reagents and equipment to room temperature. |
| Incorrect pipetting angle [67] | Alters the hydrostatic pressure, changing the aspirated volume. | Hold the pipette vertically (within 20 degrees of vertical) when aspirating. |
| Loose or leaky tips [66] | Leaking and inaccurate aspiration/dispensing. | Press tip firmly until a distinct "click" is heard; use manufacturer-recommended tips. |
| Using the wrong pipette size [66] | Drastically reduced precision. | Use a pipette where your target volume is 35-100% of its maximum capacity [67]. |
| Disregarding liquid properties [67] | Inaccurate transfer of viscous or volatile liquids. | Use reverse pipetting for viscous liquids; work quickly and use pre-wetting for volatile liquids. |
Standard Preparation and Protein Quantification
Frequently Asked Questions
Q4: What are the key considerations when choosing a protein quantification assay?
A4: Selecting the right assay is crucial for accurate concentration measurement. Your choice should be guided by three main aspects [1]:
- Stage of Drug Development: In early discovery, high-sensitivity methods like BCA or amino acid analysis are common. For release testing, robust, pharmacopoeia-described assays (e.g., specified in USP or EP) are preferred for regulatory acceptance [1].
- Quantification Goal: Determine if you need the total protein content (use colorimetric assays like Lowry or BCA) or a specific drug substance (use specific assays like ELISA or mass spectrometry) [1].
- Protein and Matrix Properties: Consider your protein's unique properties (e.g., solubility, amino acid composition) and the sample matrix. Buffer components, detergents, or chaotropic agents can interfere with many assays, so a robust method like amido-black may be necessary [1].
Q5: How can I ensure my serial dilutions for a standard curve are accurate?
A5: Serial dilution errors can propagate, leading to an inaccurate standard curve. Key steps include:
- Use the Correct Pipette: Always use a pipette optimal for the volume you are transferring [66].
- Ensure Homogeneous Mixing: After each dilution step, mix the solution thoroughly via pipette mixing or plate shaking. An inadequately mixed solution will have a non-uniform concentration, making the subsequent transfer inaccurate [70].
- Verify Performance: For critical applications, implement a volume verification method to check the accuracy and precision of your liquid handler's serial dilution protocol [70].
Table 2: Key characteristics of widely used protein quantification assays. Adapted from [1].
| Assay | Quantification Type | Key Interfering Substances | Dynamic Range | Sensitivity (Detection Limit) |
|---|---|---|---|---|
| Amido-Black | Absolute | - | - | - |
| Amino Acid Analysis | Absolute | - | - | - |
| BCA | Relative | Reducing agents, chelating agents. | - | - |
| Lowry | Relative | Detergents, sugars, triglycerides. | - | - |
| UV Absorption | Absolute | Any contaminant that absorbs at ~280 nm. | - | - |
| ELISA | Relative (for the specific protein) | Substances that affect antibody binding. | - | - |
Experimental Workflow for Protein Solubility Screening
The diagram below outlines a high-throughput workflow for determining protein solubility, a critical parameter in protein research.
Instrument Use and Maintenance
Frequently Asked Questions
Q6: How often should I calibrate my pipettes, and what are signs that they need servicing?
A6: Pipettes should undergo regular calibration, typically once or twice a year, though intensive use may require more frequent checks [66] [69]. Signs that your pipette needs service include:
- Physical Damage: Visible damage to the pipette nose cone [69].
- Inconsistent Performance: Difficulty in adjusting the volume or a plunger that feels sticky [66].
- Failed Calibration Check: Failing an in-house gravimetric check (e.g., dispensing water and measuring mass) [71] [69]. Daily cleaning with 70% ethanol and vertical storage in a pipette holder can prevent contamination and corrosion [69].
Q7: Our automated liquid handler is running, but we are seeing an increase in false positives/negatives in our screening. Could liquid handling be the cause?
A7: Yes, inaccuracies in automated liquid handling are a common source of assay failure. Even slight over- or under-dispensing of critical reagents can lead to false results [70]. To troubleshoot:
- Verify Tip Fit and Quality: Always use vendor-approved tips, as cheaper alternatives may have variable wetting properties or poor fit, causing volume errors [70].
- Check Liquid Class Settings: Ensure parameters like aspirate/dispense speeds, tip immersion depth, and liquid sensing are correctly defined for your specific reagent [70].
- Inspect for Contamination: Droplets falling from tips during movement can cause cross-contamination. Adding a trailing air gap or optimizing tip ejection locations can help [70].
Essential Research Reagent Solutions
Table 3: Key materials and equipment for accurate liquid handling and protein quantification.
| Item | Function in Experiment | Key Consideration |
|---|---|---|
| Air Displacement Pipettes | Accurate transfer of aqueous solutions in the µL to mL range. | Not ideal for volatile or viscous liquids; sensitive to temperature and technique [69]. |
| Positive Displacement Pipettes | Transfer of volatile, viscous, or corrosive samples. | No air cushion, eliminating evaporation issues; more expensive but essential for problematic reagents [69]. |
| System-Specific Tips | Form a perfect seal with the pipette barrel. | Prevent leaking and dripping; ensure accuracy. Universal tips may not fit perfectly [67] [68]. |
| Filter Tips | Prevent aerosol contamination and protect the pipette from volatile liquids. | Essential for sensitive molecular biology applications (e.g., PCR) and when pipetting volatile solvents [71]. |
| Reference Standard | Calibrant for protein quantification assays. | Must be stable and its concentration accurately determined, ideally against a primary standard [1]. |
| Automated Liquid Handler | High-throughput, reproducible liquid transfers for screening and assays. | Reduces human error but requires careful calibration and method optimization to be accurate [71] [70]. |
Ensuring Data Integrity: Method Validation and Platform Comparison
For researchers and drug development professionals focused on optimizing protein concentration measurements, the validation of analytical methods is a critical pillar of data integrity and regulatory compliance. The International Council for Harmonisation (ICH) Q2(R2) guideline provides the foundational framework for this validation, outlining the key parameters that ensure your analytical procedures are fit for purpose [72]. This technical support center delves into four of these critical parameters—Accuracy, Precision, Specificity, and Linearity—within the context of protein analysis. You will find detailed troubleshooting guides and FAQs designed to address specific, real-world issues encountered in the lab, helping you generate reliable, defensible data for your research and regulatory submissions.
Core ICH Validation Parameters Explained
The following parameters are essential for demonstrating that your protein quantification method is reliable and reproducible.
Specificity: The ability of the method to assess unequivocally the analyte of interest in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [73]. For protein quantification, this means ensuring the signal measured comes only from the target protein and not from buffers, host cell proteins, or other interferents.
Accuracy: The closeness of agreement between the value which is accepted either as a conventional true value or an accepted reference value and the value found [1] [73]. This expresses how correct your protein concentration measurements are.
Precision: The closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [1] [73]. Precision is considered at three levels:
- Repeatability: Precision under the same operating conditions over a short interval of time (intra-assay precision).
- Intermediate Precision: Precision within the same laboratory, accounting for variations like different analysts, days, or equipment.
- Reproducibility: Precision between different laboratories.
Linearity: The ability of the method (within a given range) to obtain test results that are directly proportional to the concentration (amount) of analyte in the sample [73]. For protein assays, this confirms that the method provides a proportional response across a defined concentration range.
The relationship and role of these parameters in the method validation workflow are illustrated below.
Troubleshooting Guides
Low Accuracy in Protein Concentration Measurements
Problem: Your measured protein concentrations consistently deviate from the accepted reference value.
Investigation and Resolution:
| Step | Question to Ask | Action / Solution |
|---|---|---|
| 1 | Is the protein standard appropriate? | Use a well-characterized primary standard (e.g., from NIST). Ensure the standard protein matches your target protein's characteristics to minimize matrix effects [1]. |
| 2 | Are there substance interferences? | Identify buffer components (detergents, reducing agents) that interfere with your assay. Consider switching to a more compatible assay (e.g., from UV-Vis to BCA if detergents are present) [2]. |
| 3 | Is the sample homogeneous? | Ensure samples are properly mixed and clarified. Centrifuge to remove precipitates or aggregates that lead to uneven sampling. |
| 4 | Is the method itself biased? | Validate against a so-called "gold standard" method like amino acid analysis, acknowledging that no single method serves as a universal standard for all proteins [1]. |
Poor Precision and High Variability
Problem: Replicate measurements of the same protein sample show unacceptably high scatter.
Investigation and Resolution:
| Step | Question to Ask | Action / Solution |
|---|---|---|
| 1 | Is the sample pipetting accurate? | Calibrate pipettes regularly and use reverse pipetting for viscous solutions. Use consistent pipetting techniques across all users. |
| 2 | Is the incubation time/temperature consistent? | Control incubation times and temperatures strictly. Use a heated microplate mixer for assays like BCA that are temperature-sensitive [2]. |
| 3 | Are multiple analysts or instruments involved? | If high inter-assay variability is noted, establish and document intermediate precision by qualifying all instruments and standardizing SOPs across analysts [1] [73]. |
| 4 | Is the protein adsorbing to surfaces? | Use low-protein-binding tubes and plates. Include carrier proteins if appropriate, or use a defined sequence for sample processing. |
Specificity and Interference Issues
Problem: The quantification method is affected by other components in the sample matrix, leading to inflated concentration values.
Investigation and Resolution:
| Step | Question to Ask | Action / Solution |
|---|---|---|
| 1 | What is in your sample buffer? | Test a blank buffer to establish a baseline signal. Common interferents include Triton X-100, SDS, Tris, and EDTA [2]. |
| 2 | Does the assay respond to the wrong proteins? | If quantifying a specific protein (e.g., a drug substance) amidst impurities, use a specific method like ELISA or LC-MS instead of colorimetric total protein assays like Bradford or BCA [1]. |
| 3 | Are there degradation products? | Perform forced degradation studies (e.g., expose the protein to heat or light) and analyze the sample to confirm your method can distinguish the intact protein from its fragments [74]. |
The following diagram outlines the logical workflow for systematically diagnosing and resolving specificity issues.
Frequently Asked Questions (FAQs)
Q1: How do I choose the right protein quantification assay for my specific protein and stage of research?
The choice depends on three main aspects [1]:
- Stage of Drug Development: In early discovery, speed and sensitivity (e.g., BCA, Bradford) are key. For release testing of clinical materials, pharmacopoeial methods are preferred for regulatory acceptance.
- What Needs to Be Quantified: For total protein content, colorimetric assays (BCA, Bradford) are used. For a specific drug substance amidst impurities, specific assays like ELISA or mass spectrometry are necessary [1].
- Unique Protein Properties: Consider solubility, molecular weight, amino acid composition, and your buffer components. For example, the BCA assay is more tolerant of detergents, while the Bradford assay is not [2].
Q2: What are the typical acceptance criteria for linearity in a protein assay validation?
For assay methods (like potency testing), the ICH guidelines typically require a correlation coefficient (r) of at least 0.995 across a concentration range of 80-120% of the expected test concentration. For impurity methods, the range should be broader, from the quantitation limit (LOQ) to 120% of the specification level [73]. Always evaluate residual plots, not just the r value, to detect bias in the regression model.
Q3: My protein has an atypical amino acid composition (e.g., low tyrosine/tryptophan). How does this affect accuracy and which assay should I use?
This significantly affects accuracy. Colorimetric assays (UV-Vis at 280nm, BCA, Bradford) rely on specific amino acids for signal generation. Proteins low in aromatics (Tyr, Trp) will have their concentration underestimated by UV-Vis and BCA, while proteins low in basic residues (Lys, Arg) will be underestimated by the Bradford assay [2]. In such cases, amino acid analysis is a more accurate choice, as it hydrolyzes the protein and quantifies the individual amino acids, providing a highly reproducible result independent of the protein's structure [1].
Q4: When and how should I perform a robustness test for my protein quantification method?
Robustness should be tested during the method development phase, before full validation begins. It involves making small, deliberate variations to method parameters to ensure the method remains reliable under normal operating conditions. You should test [1] [73]:
- Environmental factors: Different incubation temperatures or times.
- Reagent modifications: Slight changes in pH of buffers, different reagent lots or suppliers.
- Equipment variations: Using different instruments or HPLC columns from the same model. A robust method will maintain consistent performance despite these variations.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents essential for conducting protein quantification and validation experiments.
| Item | Function & Application in Protein Quantification |
|---|---|
| Primary Reference Standard | A well-characterized protein standard (e.g., from NIST or EDQM) used to calibrate in-house secondary standards. It is crucial for establishing accuracy [1]. |
| BCA Assay Kit | A colorimetric, copper-based assay compatible with many detergents. Ideal for a wide dynamic range (20–2000 µg/mL) but requires aromatic amino acids [2]. |
| Bradford Assay Kit | A rapid, one-step colorimetric assay based on Coomassie dye. Not affected by reducing agents but is disrupted by common detergents [2]. |
| ELISA Kit | Provides high sensitivity and specificity for a target protein using antibody-antigen reactions. Essential for quantifying specific proteins in complex matrices like serum [1] [2]. |
| Amino Acid Analysis Service | Considered a highly accurate reference method. It hydrolyzes protein and quantifies constituent amino acids, minimizing dependence on protein structure [1]. |
| Qualified HPLC System with UV Detector | Used for specific, precise quantification, especially for purity and impurity analysis, following pharmacopoeial methods for regulatory submissions [1]. |
A Practical Guide to Risk-Based Validation and Robustness Testing
Welcome to the Technical Support Center for Protein Analytics. This guide provides troubleshooting and best practices for risk-based method validation, helping researchers in pharmaceuticals and biotechnology ensure accurate, reliable protein quantification—a foundational step in research and development [75].
Frequently Asked Questions (FAQs)
1. What is risk-based method validation and why is it important? Risk-based method validation is a systematic approach to building risk assessment and mitigation into test method development and lifecycle management. It is crucial because good data is a corporate asset; quality data reduces the risk of poor process performance and defective products reaching patients [75].
2. My protein assay results are inconsistent. What are the potential causes? Inconsistent results can stem from several sources [75] [3] [28]:
- Test Method Variation: The measurement method itself may lack precision.
- Sampling Variation: The procedure for sampling your protein material may introduce error.
- Inherent Process Variation: The biological or manufacturing process producing the protein may be variable. A nested sampling study can be used to identify the dominant source of variation [75].
3. My test method works but seems sensitive to small changes in the protocol. How can I improve it? This indicates a lack of robustness. You should conduct a robustness study using an experimental design (e.g., a Plackett-Burman design) to evaluate the effects of small, deliberate variations in method parameters (e.g., time, temperature, pH). Based on the results, you can refine the Standard Operating Procedure (SOP) to restrict variation in influential factors [75].
4. For transmembrane proteins, why do common quantification methods (e.g., Bradford) fail and what should I use instead? Conventional methods (Lowry, BCA, Bradford) significantly overestimate the concentration of transmembrane proteins like Na,K-ATPase because they detect all proteins in a sample and are influenced by amino acid composition and membrane integration [3]. An indirect ELISA is recommended for accurate quantification of specific transmembrane proteins, as it uses antibody binding for high specificity [3].
5. How can I ensure my protein quantification method remains reliable over time? Implement Continued Method Performance Verification (CMPV). This involves periodically analyzing "blind control" or reference samples from a common source alongside routine samples. Plot the results on control charts to monitor the long-term stability (reproducibility and repeatability) of your method [75].
6. How do I choose the right protein assay for my sample? Selection depends on sample composition and required performance. Key trade-offs exist between different methods [28]:
Table 1: Comparison of Common Protein Quantification Methods
| Method | Principle | Key Advantages | Key Disadvantages / Interferences |
|---|---|---|---|
| UV Absorption | Absorbance of aromatic amino acids at 280 nm [28] | Simple; no reagents required [28] | Error-prone with protein mixtures; any UV-absorbing substance interferes [28] |
| BCA Assay | Copper reduction by peptide bonds in alkaline conditions (biuret reaction) and colorimetric detection of cuprous cation by BCA [28] | Compatible with detergents; less protein-to-protein variation than Bradford [28] | Incompatible with reducing agents (e.g., DTT) and copper-chelating agents [28] |
| Bradford Assay | Coomassie dye binding, causing a shift in its absorbance maximum [28] | Fast, easy; compatible with reducing agents and metal chelators [28] | Incompatible with detergents; high protein-to-protein variation [28] |
| Indirect ELISA | Antibody-antigen binding with secondary enzyme-linked antibody detection [3] | High specificity for target protein; works well in complex mixtures and for transmembrane proteins [3] | Requires specific antibodies; more complex and time-consuming than colorimetric methods [3] |
Troubleshooting Guides
Issue: High Variation in Protein Measurement Results
Potential Causes and Mitigation Strategies: Perform a Gage Repeatability and Reproducibility (Gage R&R) study to quantify variation from the measurement system itself [75].
- Action: Have 2-4 analysts perform 2-4 repeat tests on 5-10 identical protein samples. Analyze the data to quantify repeatability and reproducibility [75].
- Solution: If the measurement system variation is too high, investigate and control the sources of variation (e.g., analyst technique, instrument calibration).
Investigate sampling variation [75].
- Action: Conduct a nested sampling study to attribute total variation to the manufacturing process, the sampling procedure, and the test method [75].
- Solution: If sampling is a major contributor, review and standardize the sampling procedure.
Evaluate method robustness [75].
- Action: If the method is sensitive to small operational changes, conduct a robustness study. Use a fractional-factorial design to test multiple factors (e.g., buffer ionic strength, incubation time, temperature) at two levels each [75].
- Solution: For factors with a significant effect, tighten the control limits in the SOP.
Issue: Overestimation of Target Transmembrane Protein Concentration
Recommended Protocol: Indirect ELISA for Transmembrane Protein Quantification [3]
This protocol provides a specific quantification method for proteins like Na,K-ATPase.
1. Key Research Reagent Solutions Table 2: Essential Materials for Indirect ELISA
| Item | Function |
|---|---|
| Purified Protein Standard | A purified version of the target protein (e.g., NKA) for generating a standard curve. A relative standard can be created from a lyophilized aliquot of the protein [3]. |
| Coating Buffer | A buffer to immobilize the protein sample on the microplate. |
| Blocking Buffer | A solution to cover all unused protein-binding sites to prevent nonspecific binding. |
| Primary Antibody | An antibody that specifically binds to the target transmembrane protein [3]. |
| Enzyme-Linked Secondary Antibody | An antibody that binds to the primary antibody, conjugated to an enzyme for detection. |
| Enzyme Substrate | A substrate that produces a measurable signal when cleaved by the enzyme. |
| Wash Buffer | A buffer to remove unbound reagents between steps. |
2. Experimental Workflow The following diagram outlines the sequential steps of the indirect ELISA protocol:
3. Detailed Methodologies
- Plate Coating: Dilute protein samples in a coating buffer. Add a known volume to the wells of a microplate and incubate overnight to allow adsorption [3].
- Blocking: Add a blocking buffer to all wells and incubate to cover any remaining protein-binding sites.
- Primary Antibody Incubation: Add a specific primary antibody against your target protein to the wells and incubate. Then, wash the plate thoroughly to remove unbound antibody [3].
- Secondary Antibody Incubation: Add an enzyme-linked secondary antibody that recognizes the primary antibody. Incubate and wash again to remove unbound secondary antibody [3].
- Detection: Add a substrate for the enzyme. The enzyme will catalyze a reaction that produces a colorimetric signal. Measure the signal intensity with a plate reader [3].
- Data Analysis: Generate a standard curve using the purified protein standard and use it to calculate the concentration of your unknown samples [3].
Issue: Method Performance Deteriorates Over Time
Implementing Continued Method Performance Verification (CMPV) [75]
- Action: Establish a system using blind control samples.
- Protocol:
- Create a large, homogeneous batch of a control protein sample and store it in aliquots.
- Periodically (e.g., once per week or month), submit one of these control samples for analysis as a "blind" sample alongside your routine experimental samples.
- The analyst should be unaware of the control sample's identity.
- Plot the results for the control sample on a control chart (e.g., an X-bar chart for sample averages and an R-chart for ranges of replicate tests).
- Analysis: The control chart will help you distinguish between common-cause variation (inherent to the method) and special-cause variation (indicating a problem). A trend or point outside the control limits signals that the method may be deteriorating and requires investigation [75].
Risk Management Framework for Method Validation
A proactive risk management strategy is essential. The table below outlines common risks and their mitigation tools throughout the method lifecycle [75].
Table 3: Risk Management for Test Methods
| Critical Risk | Risk Mitigation Tool | Typical Stage of Use |
|---|---|---|
| Risk of missing important method design factors | Experimentation strategy (screening followed by optimization designs) | Method Design (Stage 1) |
| Risk of poor quality measurements | Gage R&R Study | Method Validation (Stage 2) |
| Risk that the method is not robust to deviation from SOP | Robustness (Ruggedness) Study | Method Validation (Stage 2) |
| Risk of poor sampling performance | Nested Sampling Studies | Method Validation (Stage 2) or Routine Use (Stage 3) |
| Risk of test method performance deterioration over time | Continued Method Performance Verification (CMPV) with control charts | Routine Use (Stage 3) |
| Risk of lack of management attention | Inclusion of method performance data in management review | All Stages |
The following diagram illustrates the interconnected lifecycle of a test method and its associated risk mitigation activities:
Technology Foundations: Antibody vs. Aptamer Recognition
The fundamental distinction between Olink and SomaScan platforms lies in their molecular recognition mechanisms. Olink employs Proximity Extension Assay (PEA) technology, which uses pairs of antibodies each conjugated with unique DNA oligonucleotides. When both antibodies bind to their target protein, the DNA strands are brought into proximity, hybridize, and are extended to create a unique DNA barcode that is quantified via qPCR or next-generation sequencing (NGS). This dual-recognition requirement provides high specificity with minimal cross-reactivity [76].
SomaScan utilizes SOMAmer (Slow Off-Rate Modified Aptamer) technology, which employs synthetic, chemically-modified single-stranded DNA or RNA aptamers engineered to bind protein targets with high affinity and specificity. These SOMAmers are selected through an iterative SELEX process that favors slow dissociation rates. After binding, target proteins are captured, unbound SOMAmers are washed away, and the bound SOMAmers are quantified using DNA microarrays or sequencing [76].
Head-to-Head Biochemical Comparison
Table 1: Fundamental technology comparison between Olink and SomaScan platforms
| Feature | Olink (PEA) | SomaScan (SOMAmer) |
|---|---|---|
| Recognition Mode | Two independent antibodies binding distinct epitopes | Single nucleic acid ligand (SOMAmer) |
| Signal Gating | Requires dual binding → DNA extension | Single binding with washing and DNA readout |
| Specificity Control | High – mispaired antibody binding yields no signal | Medium to high – depends on aptamer specificity and stringency |
| Multiplex Capability | High (with DNA barcoding) | Very high (large aptamer pools) |
| Normalization | Relatively straightforward NPX pipelines | Requires complex normalization (dilution bins, hybridization correction) |
| Manufacturing | Antibodies require expression, purification, validation | Aptamers are chemically synthesizable, scalable |
| Suitability for Novel Targets | Needs validated antibody pairs | Potentially faster for novel targets (if aptamers can be selected) [76] |
Performance Comparison & Experimental Data
Sensitivity and Dynamic Range Assessment
Detection sensitivity and dynamic range are critical parameters for platform selection, particularly for measuring low-abundance biomarkers. SomaScan employs a serial dilution scheme to extend its measurable range, achieving approximately 10-log dynamic range (femtomolar to micromolar) across its full SOMAmer repertoire in human plasma/serum. This wide dynamic range helps the platform avoid sample pre-treatment or depletion steps that can introduce bias or molecule loss [76].
Olink's PEA technology detects low-abundance proteins by translating proximity binding events into amplifiable DNA signals. In practice, Olink panels typically achieve detection of cytokines, chemokines, and signaling molecules at picomolar to sub-picomolar levels, depending on the specific panel and protein. However, as panel size increases, the effective sensitivity and precision for lower-abundance analytes can decrease due to potential probe interference in highly multiplexed reactions [76].
Reproducibility and Stability Metrics
Recent comparative studies have quantified platform performance across multiple dimensions:
Table 2: Performance metrics from comparative studies of Olink and SomaScan platforms
| Performance Metric | Olink | SomaScan | Study Context |
|---|---|---|---|
| Technical Precision (Median CV) | 6.3% (intra-assay) [77] | 6.8% (inter-assay) [76] | 102 plasma samples, duplicate measurements |
| Delayed Processing Stability | 87% of assays stable (ICC/r ≥ 0.40) [78] | 72% of assays stable (ICC/r ≥ 0.40) [78] | Samples processed immediately vs. 24-48 hours post-collection |
| Within-Person Stability (1 year) | >90% of assays stable (ICC/r ≥ 0.40) [78] | >90% of assays stable (ICC/r ≥ 0.40) [78] | 80 plasma samples from 40 participants collected 1-year apart |
| Cross-Platform Correlation | Median correlation: 0.46 (range: -0.21 to 0.97) [76] | Only 14.7% of proteins showed high correlation (r > 0.75) [78] | 417 overlapping protein comparisons in ARIC Study |
| Data Completeness | 35% of proteins had missing values [77] | ~96.2% of analytes present above detection threshold [76] | 78-sample plasma benchmarking experiment |
Proteome Coverage and Biological Relevance
The platforms differ significantly in their target coverage strategies and biological applications. Olink's Explore HT platform covers approximately 5,400+ proteins with deliberate curation to emphasize actionable, druggable, circulating, or secreted proteins rather than blanket proteome coverage. The panels are organized into modular sets focusing on specific biological domains such as immune response, neurology, metabolism, and oncology [76].
SomaScan's current 11K platform measures approximately 10,776 proteins, providing broader proteome coverage without specific biological curation. This extensive coverage makes it suitable for discovery-phase research where the goal is to identify novel protein-disease associations without pre-specified biological hypotheses [76].
In a comparative evaluation of plasma proteome coverage, Olink demonstrated higher coverage of low-abundance signaling proteins, particularly cytokines and membrane proteins, while mass spectrometry (as a reference) showed better coverage of mid-to-high abundance proteins, including enzymes, metabolic proteins, and those involved in hemostasis and blood coagulation [77]. When combined, Olink and mass spectrometry technologies covered 63% of the reference human plasma proteome, demonstrating their complementary nature [77].
Experimental Protocols for Platform Comparison
Sample Collection and Handling Protocol
Proper sample collection and handling are critical for generating reliable proteomics data. Based on validation studies, the following protocol is recommended:
Blood Collection:
- Collect blood using consistent anticoagulants (EDTA or heparin)
- Document fasting status and time of collection
- Process samples immediately or under standardized delay conditions
- For plasma: centrifuge at 2,000-3,000 × g for 10-15 minutes at 4°C
- Aliquot samples to avoid freeze-thaw cycles
- Store at ≤-130°C in liquid nitrogen freezers until analysis [78]
Sample Quality Assessment:
- Record processing time from venipuncture to freezing
- Document shipping conditions (temperature, duration)
- Avoid hemolyzed samples
- Maintain consistent freeze-thaw cycles across compared samples
- Use standardized thawing procedures (ice bath, gentle mixing) [78]
Experimental Design for Platform Comparison
For rigorous platform comparison, implement a nested study design:
Blinded Replicates Experiment:
- Include 12 participants with duplicate samples
- Process using identical anticoagulants (6 EDTA, 6 heparin)
- Include 2 quality control (QC) pools in duplicates
- Blind all samples to laboratory personnel
- Calculate intraclass correlation coefficients (ICCs) for reproducibility [78]
Delayed Processing Experiment:
- Recruit 14 donors (7 EDTA, 7 heparin)
- Process samples immediately, 24-hours, and 48-hours post-collection
- Include 2 QC pool samples
- Use Spearman's correlation coefficients to assess stability
- Determine ICC values for each time delay condition [78]
Within-Person Reproducibility:
- Collect samples from 40 participants at two time points (1-year apart)
- Include 2 QC pool samples
- Assess long-term protein stability using ICC/r values
- Account for biological variation in addition to technical variation [78]
Quality Control and Normalization Procedures
Both platforms require specific quality control measures:
Olink Quality Control:
- Use built-in QC system with normalized protein expression (NPX) values
- Apply intra- and inter-plate normalization
- Flag samples with QC warnings based on extension control performance
- Exclude assays with detection rates below study-specific thresholds [79]
SomaScan Quality Control:
- Implement complex normalization accounting for dilution bins
- Apply hybridization correction for array-based readouts
- Use calibration standards to correct for technical variations
- Perform cross-reactivity assessments for aptamer specificity [76]
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Which platform provides more accurate protein quantification for low-abundance biomarkers?
Both platforms have different strengths for low-abundance proteins. Olink's PEA technology demonstrates strong sensitivity for cytokines, chemokines, and signaling molecules at picomolar to sub-picomolar levels, particularly in focused panels. SomaScan achieves broad dynamic range through serial dilution schemes, but individual SOMAmer performance varies. For low-abundance signaling proteins, Olink often provides better sensitivity, while SomaScan offers more comprehensive coverage across concentration ranges. Before study initiation, consult platform-specific documentation for detection rates of your target proteins [76] [78].
Q2: How comparable are protein measurements between Olink and SomaScan platforms?
Cross-platform correlations vary significantly by protein. In comparative studies, Spearman correlation coefficients range from -0.13 to 0.97 with a median correlation of approximately 0.46. Only 14.7-19% of proteins show high correlation (r ≥ 0.75), while 44.8% show poor correlation (r < 0.40). This variability means direct comparison of absolute measurements between platforms is challenging. For meta-analyses combining datasets from both platforms, focus on proteins with established high cross-platform correlations or use platform-specific thresholds [78] [80] [76].
Q3: How does delayed sample processing affect protein measurements?
Both platforms demonstrate reasonable stability with delayed processing, but performance differs. When comparing samples processed immediately versus 24-48 hours later, 87% of Olink assays remain stable (ICC/r ≥ 0.40) compared to 72% of SOMAscan assays. For studies involving sample shipping, Olink may provide more robust measurements under suboptimal processing conditions. However, both platforms show excellent within-person stability (>90% of assays) in samples collected one year apart, supporting their use in longitudinal studies [78].
Q4: What is the typical sample requirement for each platform?
Olink requires very low sample volumes, typically 1 μL of plasma or serum per panel, making it suitable for studies with limited sample availability. SomaScan requires larger sample volumes due to its serial dilution approach, typically 50-100 μL per sample for the full panel. Consider sample volume requirements when selecting a platform, particularly for retrospective studies with precious biobank samples [76].
Troubleshooting Common Experimental Issues
Problem: Poor reproducibility between technical replicates
Possible Causes and Solutions:
- Sample degradation: Ensure consistent sample handling and minimize freeze-thaw cycles
- Plate effects: Use randomized plate placement and include QC samples across plates
- Insufficient sample quality: Check sample hemolysis indices and exclude compromised samples
- Platform-specific issues: For Olink, check PEA extension control performance; for SomaScan, verify hybridization controls [78] [79]
Problem: Low detection rates for target proteins
Possible Causes and Solutions:
- Protein abundance below detection limit: Consult platform-specific protein detection lists and expected concentrations
- Suboptimal sample dilution: For SomaScan, verify appropriate dilution scheme for target abundance range
- Matrix interference: Test different sample types (plasma vs. serum) and document anticoagulant use
- Antibody/aptamer performance: Check platform documentation for specific assay performance characteristics [76] [78]
Problem: Discrepant results between platforms
Possible Causes and Solutions:
- Different epitope recognition: Antibodies and aptamers may target different protein regions or proteoforms
- Variability in cross-platform correlation: Focus on proteins with established high cross-platform concordance
- Different dynamic range limitations: Confirm measurements fall within optimal quantification range for each platform
- Platform-specific normalization: Apply recommended normalization procedures for each platform [80] [77]
Research Reagent Solutions & Materials
Table 3: Essential research reagents and materials for cross-platform proteomic studies
| Reagent/Material | Function | Platform Application |
|---|---|---|
| EDTA or Heparin Tubes | Blood collection anticoagulant | Both platforms; consistency critical |
| Quality Control Pools | Inter-assay normalization | Both platforms; use across experiments |
| Normalized Protein Expression (NPX) Calibrators | Olink data normalization | Olink specific |
| SOMAmer Dilution Series | Dynamic range extension | SomaScan specific |
| DNA Extension Controls | PEA reaction efficiency | Olink specific |
| Hybridization Controls | Aptamer detection verification | SomaScan specific |
| Protein Reference Standards | Cross-platform calibration | Both platforms; method verification |
| Plate Normalization Controls | Inter-plate technical variation | Both platforms |
Platform Selection Guidelines
Choose Olink when:
- Studying low-abundance signaling proteins (cytokines, chemokines)
- Sample volume is limited (1 μL per panel)
- Focused panels aligned with biological domains
- Maximum specificity via dual antibody recognition is critical
Choose SomaScan when:
- Discovery-phase research requiring broad proteome coverage
- Wide dynamic range (10 logs) is needed without sample pre-fractionation
- Large sample volumes are available
- Studying high-to-medium abundance proteins [76] [78] [77]
For optimal results in critical applications, consider using both platforms complementarily to leverage their respective strengths and verify key findings across different technological principles.
Selecting and Qualifying a Reference Standard for Reliable Quantification
Accurate protein quantification is a foundational requirement in biological research and biopharmaceutical development, directly impacting experimental reproducibility, dosage accuracy, and product efficacy. The reliability of any quantification method is inherently tied to the quality and appropriateness of the reference standard used. This guide addresses common challenges and provides troubleshooting advice for selecting and qualifying reference standards to optimize protein concentration measurement accuracy.
Frequently Asked Questions (FAQs)
1. What are the key criteria for selecting a protein reference standard?
An appropriate reference standard must meet several critical criteria [1]:
- Agreement with Sample: The reference standard should be in good agreement with the protein of interest regarding composition, modifications, and matrix substances.
- Well-Determined Concentration: The concentration of the standard must be determined as accurately as possible, potentially using a primary reference standard from a recognized body (e.g., NIST or EDQM) for calibration [1].
- Stability: The standard must be stable for a longer period than the sample under defined storage conditions [1].
2. Why might my protein quantification results be inaccurate even with a known standard?
Inaccuracies can arise from several sources related to the standard and the assay [12] [2]:
- Protein-to-Protein Variation: Different proteins can yield different color responses in assays (e.g., BCA, Bradford) due to variations in their aromatic amino acid composition. Using a standard that is different from your target protein can lead to systematic error [2] [81].
- Interfering Substances: Buffer components, detergents, reducing agents, or salts in your sample or standard solution can interfere with the assay chemistry [12] [2].
- Incorrect Standard Curve: Errors in serial dilution during standard curve preparation, use of an expired standard, or improper curve fitting will propagate errors to your sample calculations [12] [81].
3. How do I handle a situation where no purified target protein is available for a standard?
When a pure target protein is unavailable [1] [2]:
- Use a well-characterized commercial standard like Bovine Serum Albumin (BSA) or Immunoglobulin G (IgG), but be aware that the reported concentration will be relative to this generic standard and may not reflect the absolute concentration of your specific protein.
- For the highest accuracy in such cases, consider using an absolute method like amino acid analysis, which provides very reproducible results independent of protein sequence, though it requires accounting for buffer interference [1].
- Verify the chosen method's suitability for your specific protein and sample matrix, as required by guidelines like those in USP General Chapter <507> [82].
4. My sample buffer contains interfering substances. How can I still quantify my protein accurately?
Several strategies can overcome interference [12]:
- Dilution: Dilute the sample several-fold in a compatible buffer to reduce the concentration of the interfering substance below its interference threshold, provided the protein concentration remains within the assay's working range.
- Dialysis or Desalting: Dialyze or desalt the sample into a compatible buffer to remove interfering substances.
- Protein Precipitation: Precipitate the protein using acetone or trichloroacetic acid (TCA) to remove interfering substances in the supernatant, then re-dissolve the protein pellet in the assay working reagent.
Troubleshooting Common Problems
| Problem Description | Potential Cause | Recommended Solution |
|---|---|---|
| Low absorbance values in unknown samples | Buffer conditions (pH, etc.) are not optimal for the assay or protein [12]. | Repeat the assay using optimal buffer conditions and use them to prepare the standard curve. |
| High variation between replicate measurements | Inaccurate pipetting, especially of low volumes [12]. | Use reverse-pipetting techniques to prevent air bubbles and pipette volumes of at least 5 µL for better consistency. |
| Standard curve fails calibration | The standard has degraded or the kit has expired [12]. | Replace the standard and kit components. Ensure proper storage conditions. |
| Discrepancy between predicted and expected concentration | Spectral interference from buffer components in UV-Vis methods [2]. | Switch to a more specific method (e.g., ELISA) or use a method less prone to such interference (e.g., BCA). Ensure the standard and sample are in the same matrix. |
| "Standards Incorrect" error on instrument | High contamination in the buffer causing high background [12]. | Replace the assay kit and use fresh, clean buffers. |
Experimental Protocols
Protocol 1: Preparing a Standard Curve for a Colorimetric Assay (e.g., BCA or Bradford)
Principle: Sample protein concentrations are determined by comparing their assay responses to a dilution-series of standards of known concentration [81].
Materials:
- Protein Standard (e.g., BSA at 2 mg/mL)
- Compatible Diluent (typically the same buffer as your samples)
- Protein Assay Reagent
- Microplate or Test Tubes
- Spectrophotometer
Procedure:
- Prepare Standard Dilutions: In clean vials, perform a serial dilution of the stock standard to create a range of concentrations. The table below provides an example for a BCA assay [81]:
Table: Example BSA Standard Preparation for BCA Assay
Vial Volume of Diluent Volume and Source of BSA Final BSA Concentration A 0 µL 300 µL of stock 2000 µg/mL B 125 µL 375 µL of stock 1500 µg/mL C 325 µL 325 µL of stock 1000 µg/mL D 175 µL 175 µL of vial B dilution 750 µg/mL E 325 µL 325 µL of vial C dilution 500 µg/mL F 325 µL 325 µL of vial E dilution 250 µg/mL G 325 µL 325 µL of vial F dilution 125 µg/mL H 400 µL 100 µL of vial G dilution 25 µg/mL I 400 µL 0 0 µg/mL (Blank) - Assay Standards and Samples: Mix each standard and unknown sample with the assay reagent according to the kit protocol. Incubate under the specified conditions (time and temperature).
- Measure Absorbance: Use a spectrophotometer to measure the absorbance of each standard and sample.
- Generate Standard Curve: Plot the average absorbance of each standard against its known concentration. Fit a best-fit line (often linear or quadratic) to the data points.
- Determine Unknown Concentration: Interpolate the absorbance of the unknown samples onto the standard curve to calculate their concentrations [81]. Remember: the unit of measure for the unknown is the same as that used for the standards (e.g., µg/mL).
Protocol 2: Validating a Protein Quantification Assay
Principle: Before use in critical applications (e.g., IND submissions), a protein quantification assay must be validated to ensure it is robust, precise, and accurate. A risk-based strategy using Failure Mode and Effect Analysis (FMEA) is an efficient approach [1].
Materials:
- Qualified Reference Standard
- Samples in Relevant Matrix
- All assay reagents and equipment
Procedure:
- Risk Assessment: Assemble a team to conduct a risk analysis of every step in the assay protocol, from sample generation to data analysis. Categorize the potential influence of each step on the final result.
- Robustness Testing: Systematically study the parameters ranked as critical. For example, small changes to incubation time, reagent volume, or temperature should be introduced to assess their impact on the result.
- Implement Controls: Based on the robustness analysis, implement controls such as tightening tolerances in the SOP or qualifying critical system components like HPLC columns.
- Formal Validation: Once a robust assay is established, validate the following parameters as per ICH guidelines [1]:
- Accuracy: How close the measured value is to the accepted true value.
- Precision: The closeness of agreement between a series of measurements (repeatability and intermediate precision).
- Specificity: Ability to assess the analyte unequivocally in the presence of other components.
- Linearity and Range: The interval over which the method provides results directly proportional to analyte concentration.
- Detection Limit (LOD) & Quantification Limit (LOQ): The lowest amount of analyte that can be detected or quantified.
Workflow and Relationship Diagrams
Standard Qualification Workflow
Troubleshooting Logic for Inaccurate Results
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for Protein Quantification and Standard Qualification
| Item | Function & Importance |
|---|---|
| Primary Reference Standard (e.g., from NIST) | A certified standard with well-defined properties, used to calibrate secondary, in-house standards for traceability and ultimate accuracy [1]. |
| BSA for Protein Quantitation RS (e.g., USP #1076192) | A widely available reference standard suitable for use in colorimetric procedures as described in pharmacopeial chapters like USP <507> [82]. |
| IgG System Suitability RS (e.g., USP #1445550) | A reference standard used to ensure system performance in specific assays for monoclonal antibodies, such as size-exclusion chromatography (SEC) and capillary electrophoresis (CE-SDS) [82]. |
| Compatible Protein Assay Kits | Kits (BCA, Bradford, etc.) with characterized compatibility tables for common buffer substances, helping to minimize interference [12]. |
| Stable Diluent Buffer | A consistent, protein-compatible buffer for reconstituting and diluting standards and samples to maintain stability and pH. |
Troubleshooting Guides
FAQ: Addressing Common BCA Assay Validation Challenges
What are the most common substances that interfere with the BCA assay, and how can their effects be minimized?
Several substances commonly used in laboratory buffers can interfere with the BCA assay. The primary interferents include reducing agents (e.g., DTT, β-mercaptoethanol) and chelators (e.g., EDTA), which disrupt the copper reduction reaction fundamental to the assay [83] [12]. Other potential interferents are strong acids and bases and, for some kit variants, ionic detergents [12].
To minimize interference, consider the following strategies [12]:
- Dilution: Dilute the sample several-fold in a compatible buffer. This is the simplest method, provided the protein concentration remains within the assay's working range.
- Precipitation: Precipitate the protein using acetone or Trichloroacetic Acid (TCA). After removing the supernatant containing the interferent, redissolve the protein pellet in the assay working reagent.
- Dialysis or Desalting: Dialyze or desalt the sample into a buffer that is compatible with the BCA assay.
Our standard curve has a good R² value, but we observe inaccurate protein estimation in our cleaned medical device samples. What could be the cause?
This is a common challenge when residual proteins on devices have undergone thermal coagulation or denaturation, especially from exposure to high-temperature disinfection cycles (>60°C) [84]. Conventional alkaline extraction solutions (e.g., 1% SDS, pH 11.0) may not efficiently solubilize these strongly coagulated proteins, leading to low and variable recovery rates [84].
A proven solution is to use a modified recovery solution designed to handle thermally coagulated proteins. One effective formulation is 1% SDS, 10 mM Tris(2-carboxyethyl)phosphine (TCEP), and 10 mM HEPES at pH 7.0 [84]. This solution, used at room temperature, irreversibly breaks disulfide bonds and effectively solubilizes coagulated proteins, leading to recovery rates greater than 90% in validation studies [84].
How can I improve the sensitivity and accuracy of my BCA assay at low protein concentrations near the acceptance criteria (e.g., 6.4 µg/cm²)?
The low end of the standard curve is often where accuracy wanes. You can enhance sensitivity through these methodological improvements [38]:
- Optimize the Working Reagent Ratio: Increasing the sample-to-working reagent volume and adjusting the ratio (e.g., to 1:1.24) can improve the optical path length and signal.
- Increase Sample Volume: Using a larger sample volume in each well (e.g., 150 µL instead of 25 µL) increases the absolute amount of protein being measured.
- Employ the Standard Addition Method: This technique involves adding a known concentration of protein standard to your unknown sample. This moves the measurement into a more reliable, higher range of the standard curve. The value of the spiked amount is then subtracted to determine the original unknown concentration, minimizing matrix effects.
Table 1: Common BCA Assay Interferences and Solutions
| Interfering Substance | Effect on Assay | Recommended Solution |
|---|---|---|
| Reducing Agents (DTT, β-mercaptoethanol) | Reduces Cu²⁺ directly, causing false high readings | Dilute sample, use compatible assay kit, or precipitate protein [12] |
| Chelators (EDTA, EGTA) | Binds copper ions, preventing color development | Dilute sample, dialyze/desalt, or use a compatible assay [12] |
| Strong Acids/Bases | Disrupts the alkaline reaction medium | Neutralize or dilute sample [12] |
| Thermally Coagulated Protein | Incomplete solubilization leads to low recovery | Use a reducing, neutral-pH recovery solution (e.g., SDS-TCEP-HEPES) [84] |
Experimental Protocols for Key Validation Experiments
Protocol 1: Validating a Modified Recovery Solution for Thermally Coagulated Proteins
This protocol is based on the method published in Scientific Reports [84].
- Objective: To effectively recover and quantify residual proteins from medical device surfaces that have been exposed to high temperatures.
- Materials:
- Proposed Recovery Solution: 1% SDS, 10 mM TCEP, 10 mM HEPES (pH 7.0)
- Conventional Recovery Solution: 1% SDS (pH 11.0)
- Pseudo-blood-contaminated test samples (e.g., stainless steel plates)
- Micro-BCA Protein Assay Kit
- Spectrophotometer or microplate reader
- Methodology:
- Sample Preparation: Contaminate test surfaces with a known volume and concentration of protein test soil (e.g., defibrinated blood). Process these samples at various temperatures (e.g., 60°C, 80°C, 95°C) under both dry and humid conditions to simulate thermal coagulation.
- Protein Recovery: Immerse the processed test samples in either the proposed or conventional recovery solution. Ensure the solution volume is sufficient to cover the surface area.
- Extraction: Allow the samples to incubate in the recovery solution. The proposed solution works effectively with overnight incubation at 23°C or a shorter incubation with gentle agitation [84].
- Quantification: Quantify the recovered protein in the eluate using a micro-BCA method, following the kit manufacturer's instructions.
- Calculation: Calculate the protein recovery rate as (Recovered Protein / Initial Contaminating Protein) × 100. The acceptance criterion is typically a recovery efficiency greater than 70% [84].
Protocol 2: Improving Low-End Sensitivity via Working Reagent Optimization
This protocol is derived from research on improving protein assay methods [38].
- Objective: To increase the sensitivity and accuracy of the BCA assay at low protein concentrations (0.5-10 µg/mL).
- Materials:
- Micro BCA Protein Assay Kit
- Bovine Serum Albumin (BSA) standards
- 96-well plate
- Microplate reader
- Methodology:
- Standard and Sample Preparation: Prepare a dilution series of BSA standards covering a range from 0.5 µg/mL to 40 µg/mL.
- Prepare Working Reagent: Prepare the BCA working reagent as per the kit instructions (standard ratio, e.g., 50:1 Reagent A:B).
- Challenge Ratio Setup: In parallel, prepare a "challenge" working reagent with an optimized ratio. For example, pipette 150 µL of protein sample into each well and add 187 µL of working reagent, creating a sample-to-reagent volume ratio of approximately 1:1.24 [38].
- Incubation and Measurement: Cover the plate, incubate at 37°C for 60 minutes, and measure the absorbance at 562 nm.
- Data Analysis: Generate standard curves for both the standard and challenge protocols. Compare the linearity (R²), accuracy (closeness to nominal values), and precision (Relative Standard Deviation) in the low-concentration range. The optimized ratio should demonstrate improved performance metrics [38].
Table 2: Key Validation Parameters for a BCA Assay in Cleaning Efficacy
| Validation Parameter | Definition | Acceptance Criteria (Example) |
|---|---|---|
| Linearity & Range | The ability of the assay to produce results directly proportional to protein concentration within a given range [38]. | R² > 0.9900; acceptance criteria (e.g., 6.4 µg/cm²) must fall within the linear and accurate portion of the curve [38]. |
| Accuracy | The closeness of agreement between the calculated value and a reference value [1]. | Calculated value within ±15% of the nominal (theoretical) value [38]. |
| Precision (Repeatability) | The closeness of agreement under the same operating conditions over a short interval [1]. | Relative Standard Deviation (RSD) ≤ 15% for replicate measurements [38]. |
| Limit of Detection (LOD) | The lowest amount of analyte that can be detected [38]. | Typically ~2 µg/mL for standard BCA assays [38]. |
| Limit of Quantification (LOQ) | The lowest amount of analyte that can be reliably quantified with acceptable accuracy and precision [38]. | The lowest point on the standard curve that meets accuracy and precision criteria (e.g., ~2 µg/mL) [38]. |
Visualized Workflows and Pathways
BCA Assay Reaction Pathway
Experimental Selection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for BCA Assay Validation in Medical Device Cleaning
| Reagent / Material | Function | Application Note |
|---|---|---|
| BCA Protein Assay Kit | Provides optimized reagents for the colorimetric quantification of total protein [11]. | Available in "common" and "hypersensitive" types. Ensure compatibility with sample buffers [85]. |
| Bovine Serum Albumin (BSA) | The standard reference protein for creating the calibration curve [38]. | For complex test soils, validate that BSA is an appropriate reference by comparing with other proteins (e.g., mucin, lysozyme) [38]. |
| SDS-TCEP-HEPES Solution | A modified recovery solution for solubilizing thermally coagulated proteins from device surfaces [84]. | Effective at neutral pH and room temperature. TCEP irreversibly reduces disulfide bonds, improving recovery from high-temperature processed devices [84]. |
| Defibrinated Blood / Test Soil | Simulates clinical contamination for worst-case cleaning validation studies [84]. | Represents the complex protein matrix encountered in real-world use. |
| Microplate Reader | Instrument for measuring absorbance of the colorimetric complex at 562 nm [38]. | Allows for high-throughput analysis. Ensure proper path length correction if using different sample volumes [38]. |
Conclusion
Optimizing protein concentration measurement is not a one-size-fits-all endeavor but a strategic process that integrates foundational knowledge, meticulous method selection, proactive troubleshooting, and rigorous validation. The absence of a universal gold standard necessitates a deep understanding of each protein's unique properties and its specific matrix. By systematically applying the principles outlined—from choosing the correct assay to validating it against regulatory standards—researchers can significantly enhance the accuracy and reliability of their data. Future directions point towards greater automation, the integration of AI for data analysis and experimental design, and the continued refinement of high-throughput multiplexed platforms. These advancements will further empower precision medicine, accelerate drug discovery, and ensure the safety and efficacy of biotherapeutics, solidifying robust protein quantification as an indispensable component of biomedical progress.
References
- 1. Current Status of Protein Quantification Technologies [https://www.bioprocessintl.com/assays/current-status-of-protein-quantification-technologies]
- 2. Common Protein Concentration Assays: Pros & Cons [https://fluidic.com/insight/choosing-the-right-protein-concentration-assay-pros-and-cons-of-common-techniques/]
- 3. Evaluating the efficacy of protein quantification methods on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11614547/]
- 4. Advances in protein sequencing: Techniques, challenges ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993625002092]
- 5. ELISA vs Western Blot: When to Use Each Immunoassay ... [https://www.thermofisher.com/blog/life-in-the-lab/western-blot-or-elisa/]
- 6. When to use ELISA vs Western blot [https://azurebiosystems.com/blog/elisa-vs-western-blot/]
- 7. Bradford assay(考马斯亮蓝法)蛋白定量 [https://www.thermofisher.cn/cn/zh/home/life-science/protein-biology/protein-assays-analysis/protein-assays/bradford-assays.html]
- 8. Bradford protein assay [https://www.abcam.com/en-us/knowledge-center/western-blot/bradford-assay]
- 9. Bradford Assay for Determining Protein Concentration - PubMed [https://pubmed.ncbi.nlm.nih.gov/32238597/]
- 10. Bradford Assay Troubleshooting Guide Common Errors ... [https://go.zageno.com/blog/bradford-assay-troubleshooting]
- 11. BCA Protein Assay Kits Simplify Protein Measurements [https://racinecountyeye.com/2025/05/29/bca-protein-assay-kits-guide/]
- 12. Protein Assays and Quantitation Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/protein-assays-analysis-support-center/protein-assays-quantitation-support/protein-assays-quantitation-support-troubleshooting.html]
- 13. Lowry Protein Assay - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/lowry-protein-assay]
- 14. The Lowry Protein Assay: A Time-Tested Method for ... [https://www.metwarebio.com/lowry-protein-assay-guide/]
- 15. Correcting Ultraviolet-Visible Spectra for Baseline Artifacts [https://www.sciencedirect.com/science/article/pii/S0022354923003350]
- 16. Spectrophotometer Selection and Troubleshooting [https://sperdirect.com/blogs/news/spectrophotometer-selection-and-troubleshooting-a-practical-guide?srsltid=AfmBOopoece4xVzz4WgNSpAtTWROG27-Hdy2PpMngM1uxG_F_YzO2TMf]
- 17. in Immunoassay - PMC Interferences [https://pmc.ncbi.nlm.nih.gov/articles/PMC1904417/]
- 18. Top 10 FAQs on optimizing dPCR assays on the QIAcuity [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/science-matters/pcr-solutions/top-10-most-frequently-asked-questions-about-digital-pcr-assay-optimization-on-the-qiacuity]
- 19. Immunoprecipitation Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/ip-troubleshooting-guide?srsltid=AfmBOorqA_v7kPwlK0KF7j5JUA7yo-SRJFA6T9YOtECphws_k0L-cAb6]
- 20. FAQs and Guidelines for Successful AlphaLISA SureFire ... [https://www.revvity.com/ask/faqs-and-guidelines-successful-alphalisa-surefire-assay-setup]
- 21. nELISA: a high-throughput, high-plex platform enables ... [https://www.nature.com/articles/s41592-025-02861-6]
- 22. Western blotting vs. ELISA [https://www.abcam.com/en-us/knowledge-center/western-blot/elisa-vs-western-blot]
- 23. How to Avoid Common Pitfalls in BCA Assay Measurements [https://synapse.patsnap.com/article/how-to-avoid-common-pitfalls-in-bca-assay-measurements]
- 24. ELISA Assay Validation: Best Practices, Methods, and Key ... [https://www.nebiolab.com/elisa-assay-validation-guide/]
- 25. 2种常见蛋白定量方法——蛋白定量BCA法VS Bradford法 [https://www.bio-review.com/bca/]
- 26. Bradford法- Opentrons中国官网 [https://opentrons.com.cn/applications/bradford-assay/]
- 27. Western Blot常见问题分析 [https://www.affbiotech.com/article/2020/07/09/52.html]
- 28. Overview of Protein Assays Methods [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-protein-assays.html]
- 29. Selecting Protein Assays? These Are the Top Factors That ... [https://info.gbiosciences.com/blog/selecting-protein-assays-these-are-the-top-factors-that-can-impact-accuracy]
- 30. and Quantitation Support— Protein Assays Troubleshooting [https://www.thermofisher.com/pt/en/home/technical-resources/technical-reference-library/protein-assays-analysis-support-center/protein-assays-quantitation-support/protein-assays-quantitation-support-troubleshooting.html]
- 31. How to choose the right buffer for your protein [https://nanotempertech.com/blog/how-to-choose-the-right-buffer-for-your-protein/]
- 32. Optimizing Protein Quantification with Qubit Assay Kits - ISCA [https://www.iscaconsortium.org/optimizing-protein-quantification-with-qubit-assay-kits-ensuring-accurate-protein-measurements-for-structural-and-functional-studies/]
- 33. Protein Detection & Quantification Market Size [https://www.imarcgroup.com/protein-detection-quantification-market]
- 34. Validation of Protein Quantification Assays [https://www.genengnews.com/insights/validation-of-protein-quantification-assays/]
- 35. Approaches to Determinate Protein Concentration [https://www.cusabio.com/c-21049.html?srsltid=AfmBOoqNzkll2R2TIFKQnuIrxDvKE5URoOAN5qYibQCKfS9rn4Y6yLyr]
- 36. Quantitative analysis of therapeutic proteins in biological fluids [https://pmc.ncbi.nlm.nih.gov/articles/PMC10003146/]
- 37. Optimizing Accuracy and Depth of Protein Quantification in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7775882/]
- 38. Improving Protein Assay Methods to More Accurately Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10764063/]
- 39. Comparative Analysis of Protein Quantification Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6358724/]
- 40. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 41. Tutorial: best practices and considerations for mass ... [https://www.nature.com/articles/s41596-021-00566-6]
- 42. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 43. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 44. Generative Integrating with AI - High ... :: SSRN Throughput Screening [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5317101]
- 45. High background in immunohistochemistry [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-in-immunohistochemistry]
- 46. Troubleshooting and Optimizing a Western Blot [https://blog.addgene.org/troubleshooting-and-optimizing-a-western-blot]
- 47. Causes Of High Background In ELISA Tests and How to ... [https://www.caltagmedsystems.co.uk/information/causes-of-high-background-in-elisa-tests-and-how-to-solve-them/]
- 48. 7 Tips For Optimizing Your Western Blotting Experiments [https://www.ptglab.com/news/blog/7-tips-for-optimizing-your-western-blotting-experiments/?srsltid=AfmBOooQmk2NvZsc0Hjo-K5wKGAAtn8cwEUwD6GsspRIlmqHHA416X8g]
- 49. Optimizing Assay Performance for High-Throughput Screens - BellBrook Labs [https://bellbrooklabs.com/optimizing-assay-performance-for-hts/]
- 50. Optimizing 96 Well Plate Well Volume for Precision [https://ucallmlabs.com/optimizing-96-well-plate-well-volume-for-precision/]
- 51. 101 ELISA Troubleshooting Tips for Research in 2024 [https://www.assaygenie.com/101-elisa-troubleshooting-tips?srsltid=AfmBOoq2_v5GawJtfgCxebtZgjhngqLwD_kwqLMYDZFDx4C0BRGomzdY]
- 52. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 53. ELISA Plate Washing Optimization [https://www.bosterbio.com/protocol-and-troubleshooting/picokine-elisa-optimization/washing?srsltid=AfmBOoqnw72pS0xoyy2Zhm4LDuL03EQSTKiizThahk21Peyy-lkycN_n]
- 54. How to optimise the gain setting of my microplate reader? [https://www.bmglabtech.com/en/howto-notes/how-to-optimise-the-gain-setting-of-my-microplate-reader/]
- 55. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/faqs/?srsltid=AfmBOooIFD0pTOO71RlqwJYUcOhpp12Kaf7DmFhZpdqJstEIIEkSHQ0H]
- 56. The case for calibration-free concentration analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12203858/]
- 57. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/guidelines?srsltid=AfmBOoqELQBnbjMhTG9SsQsTSFN7hxaCjAiUzDbNbhRaO2e1j7AMvJy8]
- 58. Overview of dialysis, desalting, buffer exchange and ... [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-buffer-exchange.html]
- 59. When to Avoid Dialysis during Protein Purification? [https://www.heraldopenaccess.us/openaccess/when-to-avoid-dialysis-during-protein-purification]
- 60. The Standard Addition Method for determing concentrations. [https://www.graphpad.com/support/faq/the-standard-addition-method-for-determing-concentrations/]
- 61. A Guide to Standard Addition Testing for ICP Analysis [https://www.inorganicventures.com/blog/news/a-guide-to-standard-addition-testing-for-icp-analysis]
- 62. Standard Additions [https://www.sepscience.com/hplc-solutions-89-standard-additions-6922]
- 63. Top 5 Protein Quantification Assays [https://bitesizebio.com/23824/top-5-protein-quantification-assays/]
- 64. The case for calibration-free concentration analysis [https://pubmed.ncbi.nlm.nih.gov/40503728/]
- 65. Development of a potential primary method for protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914023005489]
- 66. 5 Common Liquid Handling Errors and How to Prevent Them [https://pipettetips.com/blogs/blog/5-common-liquid-handling-errors-and-how-to-prevent-them?srsltid=AfmBOoonue1g8vgobD_4Yr2iCRQhfe2bHP9sdwNhXhg_CPM--J_7lImL]
- 67. 8 common pipetting errors and how to avoid them | INTEGRA [https://www.integra-biosciences.com/united-states/en/stories/8-common-pipetting-errors-and-simple-solutions-address-them]
- 68. 10 Steps to Improve Pipetting Accuracy [https://www.thermofisher.com/us/en/home/life-science/lab-plasticware-supplies/lab-plasticware-supplies-learning-center/lab-plasticware-supplies-resource-library/fundamentals-of-pipetting/proper-pipetting-techniques/10-steps-to-improve-pipetting-accuracy.html]
- 69. 17 Ways to Stop Pipetting Errors From Ruining Your ... [https://bitesizebio.com/344/17-ways-to-stop-pipetting-errors-ruining-your-experiments/]
- 70. Automated Liquid Handlers as Sources of Error [https://www.aicompanies.com/education-training/knowledge-center/automated-liquid-handlers-as-sources-of-error/]
- 71. Error-Free and Optimized Liquid Handling with These ... [https://resources.govsci.com/error-free-liquid-handling/]
- 72. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 73. Key ICH Method Validation Parameters to Know [https://altabrisagroup.com/ich-method-validation-parameters/]
- 74. The ICH Just Released Its Overhauled Stability Guideline ... [https://insider.thefdagroup.com/p/ich-q1]
- 75. Risk-Based Test Method Development, Validation and Life ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/517625-Risk-Based-Test-Method-Development-Validation-and-Life-Cycle/]
- 76. Olink vs SomaScan: Sensitivity, Coverage, and Data Quality [https://olinkpanel.creative-proteomics.com/knowledge/olink-vs-somascan.html]
- 77. Comparative evaluation of Olink Explore 3072 and mass ... [https://www.nature.com/articles/s42004-025-01753-2]
- 78. comparing the Olink and SOMAscan platforms - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9923770/]
- 79. Documents [https://olink.com/knowledge/documents]
- 80. Comparison of Proteomic Assessment Methods in Multiple ... [https://olink.com/publication/comparison-of-proteomic-assessment-methods-in-multiple-cohort-studies]
- 81. Protein Assay Data Analysis [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/protein-assay-data-analysis.html]
- 82. New USP Standards for Proteins [https://qualitymatters.usp.org/new-usp-standards-characterization-therapeutic-proteins]
- 83. Protein Quantification Assay Optimization [https://www.bosterbio.com/protocol-and-troubleshooting/western-blotting-optimization/protein-quantification?srsltid=AfmBOopULx04k-MXXQ3GF14J4m4qcaTCmsdQ9rMeF0n2ywMbTQMewIIa]
- 84. Design and validation of a method for evaluating medical ... [https://www.nature.com/articles/s41598-024-72473-1]
- 85. BCA Protein Assay Kit 2025-2033 Overview [https://www.datainsightsmarket.com/reports/bca-protein-assay-kit-194519]