Clearance Mechanisms of Protein Aggregation in Alzheimer's Disease: Pathways, Therapeutic Targeting, and Future Directions
This article provides a comprehensive analysis of protein aggregation clearance pathways in Alzheimer's disease, targeting researchers and drug development professionals.
Clearance Mechanisms of Protein Aggregation in Alzheimer's Disease: Pathways, Therapeutic Targeting, and Future Directions
Abstract
This article provides a comprehensive analysis of protein aggregation clearance pathways in Alzheimer's disease, targeting researchers and drug development professionals. It explores the foundational biology of amyloid-β and tau clearance mechanisms, examines advanced methodological approaches for studying these pathways, discusses current challenges and optimization strategies in therapeutic development, and validates approaches through comparative analysis of existing and emerging therapies. The synthesis integrates current understanding from proteomic studies, cellular degradation systems, and recent clinical trial data to present a holistic view of the field and identify promising future research directions for disease-modifying treatments.
The Cellular Machinery: Understanding Fundamental Clearance Pathways in Alzheimer's Pathology
Protein aggregation is a defining pathological feature of numerous neurodegenerative diseases, with Alzheimer's disease (AD) being the most prevalent [1]. The aggregation of proteins such as amyloid-β (Aβ) and tau follows a progressive pathway from soluble monomers to insoluble fibrils and plaques [2] [3]. While historically considered inert end-products, emerging evidence underscores the heightened toxicity of soluble oligomeric species, which are now regarded as primary drivers of neurotoxicity and synaptic dysfunction [2] [1]. This whitepaper provides a comprehensive technical overview of the molecular mechanisms, experimental methodologies, and clearance pathways associated with Aβ and tau aggregation, with particular focus on their implications for therapeutic development in Alzheimer's disease research.
The pathological significance of protein aggregates extends beyond their structural presence to their prion-like propagation capabilities, facilitating spread across neural networks and exacerbating disease progression [1]. Understanding the spatial-temporal dynamics of these aggregates, particularly the early oligomeric forms, provides critical insights for developing targeted therapeutic strategies aimed at the initial stages of the pathological cascade [2] [4].
Amyloid-β (Aβ) Aggregation Pathway
Molecular Genesis and Oligomerization
The amyloid-β pathway begins with the enzymatic processing of amyloid precursor protein (APP), a transmembrane protein widely produced by brain neurons, vascular and blood cells [4]. Sequential proteolytic cleavage of APP by β-secretase (BACE1) at the ectodomain and γ-secretase at intramembranous sites generates Aβ peptides of varying lengths, with Aβ1-40 and Aβ1-42 being the most prominent [4]. The Aβ1-42 variant exhibits particularly strong aggregation propensity due to its enhanced hydrophobicity [4].
In the initial phase of aggregation, Aβ monomers undergo conformational changes to form soluble, oligomeric assemblies (AβOs). These oligomers are characterized by their amorphous structures rich in exposed hydrophobic regions, rendering them highly reactive and potentially the most hazardous type of aggregate [2] [1]. The formation of fibril-free AβO solutions demonstrated that while Aβ is essential for memory loss, the fibrillar Aβ in amyloid deposits is not the primary pathogenic agent [2]. Different species of AβOs have been identified, with ongoing research investigating which specific oligomeric forms represent the major pathogenic culprits [2].
Table 1: Key Characteristics of Amyloid-β Oligomers (AβOs)
| Property | Description | Experimental Evidence |
|---|---|---|
| Structure | Amorphous with exposed hydrophobic regions; β-sheet-rich | SDS-PAGE shows bands at ~4-24 kDa; conformation-specific antibodies [2] |
| Toxicity Mechanisms | Bind to synaptic receptors; induce Ca2+ overload; trigger oxidative stress | LTP inhibition in hippocampal slices; neuronal hyperactivity; synapse loss [2] |
| Cellular Localization | Extracellular and intracellular pools; association with surface membranes | Immunohistochemistry of AD brain; extracellular accumulation in CSF [2] |
| Pathological Consequences | Synaptic dysfunction, tau hyperphosphorylation, insulin resistance, inflammation | Animal models show memory impairment; rescue by AβO antibodies [2] |
Aβ Oligomer Toxicity Mechanisms
Soluble AβOs act as pathogenic gain-of-function ligands that target specific cells and synapses [2]. The binding of AβOs to neuronal surfaces triggers a cascade of pathogenic events including redistribution of critical synaptic proteins and hyperactivity in metabotropic and ionotropic glutamate receptors [2]. This leads to Ca2+ overload and instigates major facets of AD neuropathology, including tau hyperphosphorylation, insulin resistance, oxidative stress, and synapse loss [2].
Over a dozen candidate toxin receptors have been proposed for AβOs, with their binding triggering a redistribution of critical synaptic proteins [2]. The clinical relevance of AβOs has been established through their accumulation in AD brain and CSF, and their presence correlates with cognitive decline [2]. The vulnerability of specific neuronal populations to AβOs may explain why early-stage AD specifically targets memory circuits [2].
Figure 1: Amyloid-β Aggregation Pathway and Toxicity Mechanisms. The pathway progresses from APP processing through increasingly structured aggregates. The soluble Aβ oligomer (AβO) is highlighted as the primary toxic species that binds to synaptic receptors, triggering downstream pathological events.
Tau Aggregation Pathway
From Physiological Function to Pathological Aggregation
Tau is a predominantly neuronal, intrinsically disordered protein that is normally bound to microtubules, where it acts to modulate neuronal and axonal stability [3]. Under physiological conditions, tau promotes microtubule assembly and stability, and facilitates axonal transport [3]. In humans, six tau isoforms are expressed in the adult brain through alternative splicing of the MAPT gene, generating isoforms with either three (3R) or four (4R) microtubule-binding repeats [5].
The pathological transformation of tau begins with post-translational modifications, particularly hyperphosphorylation, which reduces tau's affinity for microtubules and promotes its aggregation [3] [5]. In the AD brain, tau protein is two to threefold hyperphosphorylated compared to the normal adult brain [5]. This hyperphosphorylation is driven by an imbalance between kinase and phosphatase activities [3].
Tau Oligomerization and Toxicity
Dissociated tau monomers undergo conformational changes leading to the formation of soluble tau oligomers (TauO), which are now recognized as the most toxic tau species [6] [3] [5]. These oligomers are highly heterogeneous and dynamic entities that exhibit prion-like properties, enabling their propagation between cells [3] [1]. Tau oligomers cause synaptic loss in wild-type human tau transgenic mice and impair cognitive, mitochondrial, and synaptic functions [6].
The toxicity of both brain-derived tau oligomers (BDTO) and recombinant TauO (rTauO) has been well demonstrated in vivo [6]. Injecting mice with BDTO in brain areas close to or inside the hippocampus causes prompt memory impairment [6]. TauO-injected mice display impairment of cognitive, mitochondrial, and synaptic abnormalities [6]. Importantly, soluble tau oligomers are now regarded as probably the most pathologically relevant species, with evidence indicating that they inhibit neural network activity independent of fibril formation [3] [5].
Table 2: Characteristics of Pathological Tau Species
| Tau Species | Structure | Toxicity | Detection Methods |
|---|---|---|---|
| Physiological Tau | Intrinsically disordered; binds microtubules | Non-toxic; regulates axonal transport | Western blot, immunohistochemistry |
| Hyperphosphorylated Tau | Reduced microtubule binding; aggregation-prone | Intermediate toxicity; disrupts cytoskeleton | Phospho-specific antibodies (AT8, AT100) |
| Tau Oligomers (TauO) | β-sheet-rich; soluble; heterogeneous | Highly toxic; synaptic dysfunction; propagates between cells | T22 antibody; T18 antibody; size exclusion chromatography |
| Neurofibrillary Tangles | Insoluble fibrils; paired helical filaments | Historically considered toxic but may be protective sequestration | Thioflavin-S; Gallyas silver staining; electron microscopy |
Figure 2: Tau Protein Aggregation Pathway and Pathological Consequences. The transformation from physiological tau to hyperphosphorylated tau initiates the aggregation cascade. Tau oligomers (TauO) represent the primary toxic species responsible for multiple cellular dysfunctions.
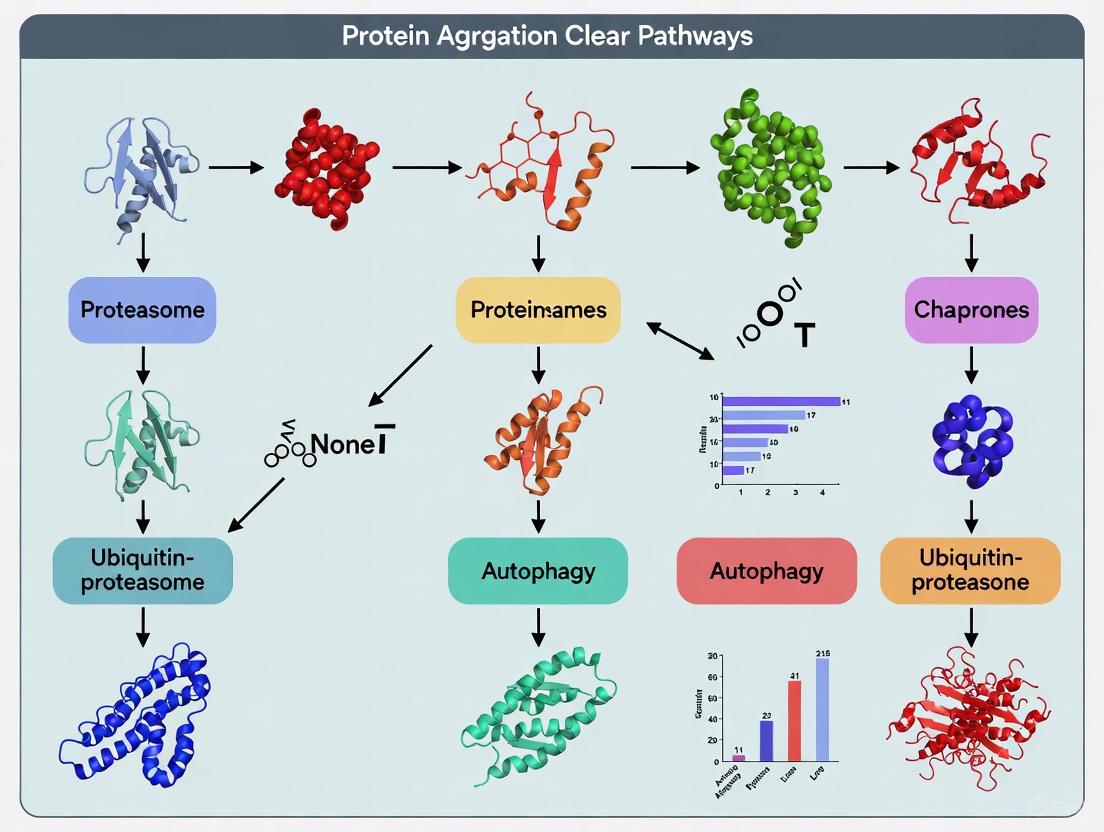
Protein Clearance Mechanisms in Alzheimer's Disease
Cellular Proteostasis Networks
The ability to maintain a functional proteome, or proteostasis, declines during the ageing process, contributing to the accumulation of damaged and misfolded proteins in neurodegenerative diseases [7]. The proteostasis network encompasses two major protein clearance systems: the ubiquitin-proteasome system (UPS) and the autophagy-lysosome pathway [8] [7]. These systems work in concert to degrade unwanted, damaged, misfolded, and aggregated proteins, thereby maintaining cellular homeostasis [8].
The UPS is the primary selective proteolytic system in eukaryotic cells, regulating numerous biological processes including development, signal transduction, and inflammation [8]. In this system, proteins are targeted for degradation by ubiquitination—a sequential cascade involving E1 (activating), E2 (conjugating), and E3 (ligase) enzymes that attach ubiquitin molecules to substrate proteins [8]. Polyubiquitinated proteins are then recognized and degraded by the 26S proteasome, a multi-catalytic protease complex [8].
Autophagy-Lysosome Pathway
The autophagy-lysosome pathway represents the second major proteolytic system, with particular relevance for the clearance of protein aggregates that cannot be degraded by the proteasome [8] [7]. Autophagy can be classified into three main types: macroautophagy, microautophagy, and chaperone-mediated autophagy (CMA) [8]. Macroautophagy involves the formation of double-membrane vesicles called autophagosomes that engulf cytoplasmic cargo and deliver it to lysosomes for degradation [8] [7]. Approximately 35 autophagy-related genes (ATG) participate in this process, organizing into complexes that regulate each step of autophagy [7].
Chaperone-mediated autophagy (CMA) is a more selective process whereby specific cytoplasmic proteins containing a KFERQ consensus motif are recognized by the chaperone Hsc70 and transported to lysosomes via the LAMP-2A receptor for degradation [8]. Both the UPS and autophagy-lysosome pathways decline during ageing, and this failure contributes significantly to the pathogenesis of Alzheimer's disease [7].
Table 3: Protein Clearance Mechanisms in Neurodegeneration
| Clearance System | Components | Substrate Specificity | Role in AD |
|---|---|---|---|
| Ubiquitin-Proteasome System (UPS) | E1-E3 enzymes, 26S proteasome | Primarily short-lived and soluble proteins | Impaired in AD; cannot degrade oligomers/aggregates |
| Macroautophagy | ATG proteins, autophagosomes, lysosomes | Bulk cytoplasm, organelles, protein aggregates | Critical for aggregate clearance; impaired in AD |
| Chaperone-Mediated Autophagy (CMA) | Hsc70, LAMP-2A | Proteins with KFERQ motif | Declines with age; contributes to tau/Aβ accumulation |
| Microautophagy | ESCRT machinery, lysosomes | Cytosolic components directly engulfed | Role in AD not fully characterized |
Figure 3: Protein Clearance Pathways and Their Failure in Alzheimer's Disease. Cellular clearance mechanisms including the ubiquitin-proteasome system and autophagy-lysosome pathway normally degrade protein aggregates. Age-related and pathology-related impairment of these systems leads to pathological accumulation of Aβ and tau aggregates.
Experimental Methodologies for Studying Protein Aggregation
Oligomer Preparation and Characterization
The study of protein aggregation requires sophisticated methodologies to prepare, isolate, and characterize specific aggregate species. For Aβ oligomer research, methods have been developed to generate fibril-free AβO solutions that enable the specific study of oligomer toxicity without confounding effects from fibrils or monomers [2]. These preparations typically involve very low doses of Aβ or the chaperone-like action of clusterin to stabilize oligomeric species [2].
For tau oligomer research, brain-derived tau oligomers (BDTO) can be isolated from AD brain tissue and amplified by seeding pure recombinant tau monomer (rTauM) [6]. In one established protocol, a 1:100 molar ratio of BDTO to rTauM is incubated at 37°C for 48 hours with continuous rotation to generate amplified BDTO (aBDTO) [6]. Quality control of these preparations is typically performed using immunoblotting with sequence-specific anti-tau antibodies (Tau5, Tau13) and oligomer-conformation-specific antibodies (T22, T18), alongside size exclusion chromatography [6].
Assessment of Pathological Effects
Electrophysiological approaches provide valuable tools for uncovering the mechanisms of tau oligomers on synaptic transmission within single neurons [3]. Understanding the concentration-, time-, and neuronal compartment-dependent actions of soluble tau oligomers on neuronal and synaptic properties is essential for developing effective treatment strategies [3]. New approaches are being developed that address specific challenges with current methods, allowing real-time toxicity evaluation at the single-neuron level [3].
For in vivo assessment, intracerebroventricular (ICV) injections of AβOs in animal models have been shown to impair brain insulin signaling and metabolism along with memory loss, recapitulating insulin neuropathology observed in AD brain [2]. Similarly, injecting mice with BDTO in brain areas closer to or inside the hippocampus causes prompt memory impairment, demonstrating the causal role of tau oligomers in cognitive dysfunction [6].
Table 4: Research Reagent Solutions for Protein Aggregation Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Oligomer-Specific Antibodies | T22 (tau oligomers), A11 (Aβ oligomers) | Detect oligomeric conformations; avoid detection of monomers/fibrils | T22 recognizes soluble tau oligomers but not tau fibrils or monomers [6] |
| Sequence-Specific Antibodies | Tau5 (total tau), Tau13 (N-terminal tau) | Detect total tau regardless of phosphorylation state | Tau5 targets epitopes 210-230; detects both phosphorylated and non-phosphorylated tau [6] |
| Phospho-Tau Antibodies | AT8, AT100, PHF-1 | Detect specific phosphorylation epitopes | Critical for assessing tau hyperphosphorylation pathology |
| Amplification Reagents | Recombinant tau monomer (rTauM) | Amplify brain-derived tau oligomers for study | 1:100 molar ratio BDTO:rTauM, 37°C, 48h with rotation [6] |
| Oligomer Modulators | TMAO, sorbitol, GPC, citrulline | Modulate oligomer formation and toxicity | Brain osmolytes differentially affect aBDTO; TMAO prevents/clears aBDTO [6] |
Therapeutic Strategies and Research Directions
Targeting Oligomeric Species
Current therapeutic strategies increasingly focus on targeting the soluble oligomeric forms of Aβ and tau, as these are recognized as the most pathogenic species [2] [5]. For Aβ, promising approaches include the use of highly specific AβO antibodies that can eliminate toxins through immunotherapy [2]. Several monoclonal antibodies targeting Aβ have been developed, with aducanumab and lecanemab receiving FDA approval through accelerated pathways, though their efficacy and long-term safety remain under evaluation [5].
For tau pathology, therapeutic development has included approaches targeting tau post-translational modifications, particularly hyperphosphorylation [5]. Kinase inhibitors targeting enzymes such as GSK3β, CDK5, and p38α MAPK have been investigated to reduce tau hyperphosphorylation [5]. Additionally, tau immunotherapy using anti-tau antibodies is being explored to block the cell-to-cell propagation of tau pathology [5].
Enhancing Clearance Mechanisms
Modulation of protein clearance pathways represents another promising therapeutic avenue [8] [7]. Enhancement of proteasome activity or autophagic-lysosomal potential extends lifespan and protects organisms from symptoms associated with proteostasis disorders, suggesting that protein clearance mechanisms are directly linked to ageing and age-associated diseases [7].
Strategies to enhance autophagy include mTOR inhibition using compounds such as rapamycin and CCI-779, which induce autophagy [8]. Similarly, AMPK activation and Sirtuin 1 (SIRT1) modulation can stimulate autophagic flux [7]. The interdependence of the UPS and autophagy suggests that combinatorial approaches targeting multiple clearance pathways simultaneously may yield enhanced benefits [8].
Novel Diagnostic Approaches
The clinical relevance of AβOs and tau oligomers has stimulated development of diagnostic tools targeting these species [2]. An AD-dependent accumulation of AβOs in CSF suggests their potential use as biomarkers, and new AβO probes are opening the door to brain imaging [2]. Similarly, the development of tau oligomer-specific imaging agents could enable early detection of tau pathology before the formation of neurofibrillary tangles [5].
Advanced neuroimaging techniques including PET imaging with Aβ- and tau-specific tracers allow in vivo visualization and quantification of protein aggregates in the human brain [4]. These techniques have revealed the spatial-temporal evolution of brain Aβ accumulation that occurs initially in cerebral regions with neuronal populations at high metabolic bio-energetic activity rates, spreading from neocortex to allocortex to brainstem, eventually reaching the cerebellum [4].
The understanding of protein aggregation in neurodegeneration has evolved significantly from a focus on insoluble fibrils and plaques to the recognition that soluble oligomeric species are the primary drivers of toxicity and disease progression. The intricate interplay between Aβ and tau oligomers, along with the failure of cellular clearance mechanisms, creates a self-reinforcing cycle of pathology that propagates through neural networks. Current research continues to elucidate the precise structural characteristics of these oligomers, their mechanisms of toxicity, and their spatiotemporal dynamics throughout disease progression.
Therapeutic development is increasingly targeting the early stages of the aggregation pathway, with particular emphasis on neutralizing oligomeric species and enhancing cellular clearance mechanisms. The integration of advanced diagnostic tools with targeted therapeutics holds promise for early intervention in the disease process, potentially before irreversible neuronal loss occurs. Future research directions include the development of more specific oligomer-targeting agents, combinatorial approaches addressing multiple pathological processes simultaneously, and personalized therapeutic strategies based on individual biomarker profiles.
In the pathogenesis of Alzheimer's disease (AD), the accumulation of amyloid-β (Aβ) peptides in the brain represents a critical pathological hallmark. While genetic mutations can lead to increased Aβ production in familial AD, the majority of sporadic cases are characterized by an age-dependent impairment in Aβ clearance mechanisms [9] [4]. Enzymatic degradation constitutes a fundamental pathway for maintaining Aβ homeostasis, with neprilysin (NEP) and insulin-degrading enzyme (IDE) emerging as the two most prominent Aβ-degrading enzymes [10] [11]. This whitepaper provides a comprehensive technical analysis of the enzymatic pathways responsible for Aβ clearance, focusing on their distinct mechanisms, synergistic relationships, and experimental approaches for their investigation. Understanding these pathways is essential for developing targeted therapeutic strategies aimed at enhancing Aβ clearance in Alzheimer's disease.
Core Aβ-Degrading Enzymes: Mechanisms and Specificities
Neprilysin (NEP)
Neprilysin is a membrane-bound zinc metalloendopeptidase that plays a pivotal role in extracellular Aβ degradation. As a type II membrane protein, NEP exposes its C-terminal catalytic domain to the extracellular space, positioning it ideally for interacting with Aβ peptides in the brain parenchyma [9]. Recent genetic evidence has strengthened the link between NEP and AD pathogenesis, with genome-wide association studies identifying risk variants in the MME gene encoding NEP [9].
Key characteristics of NEP include:
- Primary Localization: Cell surface and extracellular vesicles, with localization regulated by phosphorylation of its N-terminal intracellular domain [9]
- Cleavage Specificity: Preferentially cleaves Aβ at residues V12-H13, H13-H14, H14-Q15, V18-F19, F19-F20, F20-A21, K28-G29, G33-L34, L34-M35, and M35-V36 [12]
- Fragment Generation: Produces small peptide fragments consisting of 2-11 amino acid residues from monomeric Aβ40 [12]
- Substrate Range: Capable of degrading both full-length Aβ and partial structures, including Aβ16 and peptide fragments generated by other enzymes [12]
A significant functional aspect of NEP is its age-dependent decline in expression, which begins approximately after age 50 in the human temporal and frontal cortices, providing a plausible explanation for increased Aβ accumulation in sporadic AD [9]. The AD-associated M8V mutation in NEP reduces extracellular Aβ degradation not by impairing catalytic activity but by increasing phosphorylation at serine 6, which decreases NEP localization on the cell surface and extracellular vesicles [9].
Insulin-Degrading Enzyme (IDE)
IDE is a conserved Zn²⁺ metalloprotease primarily located in the cytosol, with a smaller fraction present in the extracellular space [13]. Unlike NEP, IDE exhibits a strong preference for monomeric Aβ substrates and shows limited activity against aggregated forms [12].
Key characteristics of IDE include:
- Primary Localization: Mainly cytosolic with some extracellular presence [13]
- Cleavage Specificity: Cleaves Aβ at multiple sites, generating larger fragments of 6-33 amino acid residues [12]
- Substrate Specificity: Degrades only whole Aβ40 and cannot process partial structures or fragments [12]
- Allosteric Regulation: Subject to complex regulation, with certain mutations (e.g., E111Q, cf-E111Q-IDE) exhibiting selective activity against Aβ while being inactive against insulin [13]
IDE's activity is notably affected by metal ions, particularly zinc. Zinc binding to Aβ can jeopardize IDE's catalytic activity, whereas zinc removal restores its function, suggesting potential therapeutic strategies involving zinc chelation [13].
Comparative Analysis of NEP and IDE
Table 1: Comparative characteristics of major Aβ-degrading enzymes
| Characteristic | Neprilysin (NEP) | Insulin-degrading Enzyme (IDE) | Other Enzymes |
|---|---|---|---|
| Primary Localization | Cell surface, extracellular vesicles | Cytosol, extracellular space | Varies by enzyme |
| Cleavage Products | 23 peptides (2-11 aa) | 23 peptides (6-33 aa) | Varies by enzyme |
| Aggregated Aβ Degradation | Limited | Limited | Limited for most |
| Fragment Degradation | Can degrade Aβ fragments | Cannot degrade fragments | Varies |
| Genetic Association with AD | MME gene risk variants identified | Associated with sporadic AD | ECE-2, plasminogen system |
| Age-Dependent Decline | Significant decline after age 50 | Reduced in AD | Varies |
Table 2: Additional Aβ-degrading enzymes and their characteristics
| Enzyme | Localization | Reported Changes in AD | Key Features |
|---|---|---|---|
| Endothelin-converting enzyme (ECE) | Neuronal, vascular | ECE-2 reduced in AD | Membrane-bound metalloprotease |
| Plasmin | Extracellular | Plasmin/plasminogen activators reduced in AD | Serine protease, requires activation |
| Matrix metalloproteinases (MMPs) | Extracellular | MMP-2, -3, -9 unchanged in AD | Can degrade both soluble Aβ and fibrils |
| Angiotensin-converting enzyme (ACE) | Vascular, neuronal | Increased in AD (related to plaque load) | Dipeptidyl carboxypeptidase |
Experimental Models and Methodologies
In Vivo Models for Studying Aβ Degradation
Genetic Mouse Models: The AppNL-F knock-in mouse model, which harbors the Swedish (KM670/671NL) and Beyreuther/Iberian (I716F) mutations in the humanized mouse App gene, recapitulates typical Aβ pathology and neuroinflammation from approximately 8 months of age [9]. This model has been crossbred with Mme knock-out (KO) and Ide KO mice to generate:
- AppNL-F × Mme KO
- AppNL-F × Ide KO
- AppNL-F × Mme/Ide double KO
These models have demonstrated that NEP deficiency accelerates Aβ plaque formation more prominently than IDE deficiency, with double knockout exhibiting a synergistic exacerbation of plaque deposition [9].
Experimental Workflow for In Vivo Assessment:
In Vivo Experimental Workflow for Assessing Aβ Pathology
In Vitro Methodologies for Studying Enzyme Activity
Aβ Degradation Assays:
- Sample Preparation: Monomeric Aβ40 is typically dissolved in appropriate buffers (e.g., PBS or Tris-HCl) and incubated with purified enzymes at specific molar ratios [12]
- Time Course Experiments: Reactions are stopped at various time points by acidification or heating to assess degradation kinetics
- Analytical Techniques:
- Liquid Chromatography-Mass Spectrometry (LC-MS): Identifies specific cleavage fragments and degradation patterns [12]
- Diffusion-Ordered NMR Spectroscopy: Monitors degradation in solution state [13]
- Thioflavin T (ThT) Fluorescence: Measures aggregation kinetics in the presence of degrading enzymes [13]
- Electron Microscopy: Characterizes morphological changes in Aβ species after enzymatic treatment [13]
Cell-Based Systems: SH-SY5Y neuroblastoma cells have been utilized to study the functional impact of NEP mutations, particularly the AD-associated M8V variant. These systems allow assessment of extracellular Aβ degradation, enzyme localization, and the impact of post-translational modifications [9].
Comparative Degradation Mechanisms and Synergistic Relationships
Enzymatic Processing Pathways
The degradation of Aβ by NEP and IDE follows distinct mechanistic pathways with different fragment profiles. NEP generates numerous small peptides (2-11 amino acids) through cleavages primarily in the N-terminal and mid-region of Aβ, while IDE produces larger fragments (6-33 amino acids) through more limited proteolysis [12]. This differential cleavage pattern suggests complementary roles in Aβ catabolism.
Comparative Aβ Degradation Pathways by NEP and IDE
Functional Synergy Between Degradation Pathways
Recent evidence demonstrates a synergistic relationship between NEP and IDE in Aβ metabolism. While NEP deficiency has a more pronounced effect on accelerating Aβ plaque formation than IDE deficiency, the double knockout of both enzymes exacerbates plaque deposition beyond what would be expected from simply additive effects [9]. This synergy may be explained by their complementary cleavage patterns, where IDE-generated fragments can be further processed by NEP, but not vice versa [12].
The functional interaction between these enzymes extends to their response to aggregated Aβ. Neither NEP nor IDE can efficiently degrade aggregated Aβ40, highlighting the importance of targeting soluble, monomeric Aβ species for effective clearance [12]. This limitation underscores the need for therapeutic approaches that enhance enzymatic activity before significant aggregation occurs.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key research reagents for studying Aβ-degrading enzymes
| Reagent/Cell Line | Key Features | Research Applications |
|---|---|---|
| AppNL-F Mice | Knock-in model with Swedish + Iberian mutations | In vivo assessment of Aβ pathology |
| Mme KO Mice | NEP deficiency model | Studying NEP-specific contributions to Aβ clearance |
| Ide KO Mice | IDE deficiency model | Studying IDE-specific contributions to Aβ clearance |
| SH-SY5Y Neuroblastoma Cells | Human-derived cell line | Cell-based studies of enzyme function and localization |
| cf-E111Q-IDE Mutant | Catalytically inactive against insulin | Studying allosteric regulation and Aβ-specific degradation |
| Monoclonal Aβ Antibodies | Specific to various Aβ epitopes | Detection of full-length Aβ and degradation fragments |
Research Gaps and Future Directions
Despite significant advances in understanding Aβ-degrading enzymes, several critical knowledge gaps remain. The precise mechanisms regulating the age-dependent decline of NEP expression are not fully elucidated. Similarly, the factors controlling IDE's transition between cytosolic and extracellular compartments require further investigation. The recent identification of AD-associated risk variants in the MME gene underscores the need to characterize the functional impact of these genetic changes on NEP activity and regulation [9].
Future research should focus on:
- Developing selective activators of NEP and IDE that enhance Aβ degradation without affecting other physiological substrates
- Exploring combination approaches that simultaneously target multiple degradation pathways
- Investigating the temporal window for therapeutic intervention, given the limited efficacy of these enzymes against aggregated Aβ
- Developing better biomarkers to monitor Aβ degradation activity in human subjects
The strategic upregulation of key Aβ-degrading enzymes represents a promising approach for preclinical AD intervention, particularly as evidence continues to support the role of impaired Aβ clearance in sporadic Alzheimer's disease pathogenesis [9].
Alzheimer's disease (AD), the most common cause of dementia, is characterized pathologically by the excessive accumulation of toxic protein aggregates in the brain—primarily amyloid-β (Aβ) plaques and hyperphosphorylated tau neurofibrillary tangles (NFTs) [14] [15]. The progressive buildup of these misfolded proteins suggests a critical failure in the brain's protein quality control mechanisms, particularly the ubiquitin-proteasome system (UPS) and the autophagy-lysosomal pathway (ALP) [16] [17]. These two systems represent the major intracellular routes for maintaining proteostasis through the selective degradation of damaged organelles, misfolded proteins, and protein aggregates [18]. A growing body of genetic, pathological, and experimental evidence now confirms that impairment of both the UPS and ALP contributes significantly to AD pathogenesis [16] [14] [19]. This technical review examines the mechanisms, interactions, and therapeutic targeting of these essential clearance systems within the context of Alzheimer's disease research.
The Ubiquitin-Proteasome System: Mechanism and Role in AD
UPS Molecular Machinery
The ubiquitin-proteasome system is the primary pathway for targeted degradation of short-lived and soluble proteins in eukaryotic cells [20]. This highly specific process occurs through two sequential steps: (1) tagging of target proteins with ubiquitin, and (2) degradation by the proteasome [16].
The tagging reaction involves a cascade of three enzymes: ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes. Initially, a ubiquitin monomer is activated in an ATP-dependent reaction by E1. The activated ubiquitin is then transferred to an E2 enzyme. Finally, an E3 ligase facilitates the covalent attachment of ubiquitin to the target protein. Repeated cycles add multiple ubiquitin molecules to form a polyubiquitin chain, with chains of four or more ubiquitins serving as the recognition signal for proteasomal degradation [16].
The proteasome complex, known as the 26S proteasome, consists of three major subunits: a 20S catalytic core and two 19S regulatory caps. The 20S core contains three distinct proteolytic activities: chymotrypsin-like, trypsin-like, and peptidylglutamyl-like activities [16]. The 19S regulatory caps recognize polyubiquitinated proteins, facilitate substrate unfolding, and gate access to the catalytic channel [16].
UPS Dysfunction in Alzheimer's Pathology
Multiple lines of evidence demonstrate UPS impairment in AD brains. Histopathological studies show ubiquitin accumulations in both plaques and tangles [16]. The AD brain also contains ubiquitin-B mutant protein (UBB+1), which blocks ubiquitin-dependent proteolysis and may mediate Aβ-induced neurotoxicity [16]. Additionally, the ubiquitin carboxy-terminal hydrolase L1 (UCH-L1), which liberates ubiquitin monomers from polyubiquitinated proteins, is oxidized and down-regulated in specific brain regions of early AD cases [16].
Mechanistic studies reveal complex interactions between AD pathology and UPS function. Keller et al. demonstrated a selective decrease in proteasome activity in AD-vulnerable brain regions like the hippocampus, while less susceptible regions like the cerebellum showed no changes [16]. In vitro evidence indicates that Aβ40 directly binds inside the proteasome and selectively inhibits its chymotrypsin-like activity [16]. Aβ42 similarly impairs proteasome function, with oligomeric species potentially exhibiting the greatest inhibitory effect [16]. Genetic studies further support UPS involvement, showing positive associations between AD and single-nucleotide polymorphisms in UBQLN1, which encodes the ubiquitin-like protein ubiquilin [16].
Table 1: Key Evidence Linking UPS Impairment to Alzheimer's Disease
| Evidence Type | Specific Findings | Research Methods |
|---|---|---|
| Histopathological | Ubiquitin accumulation in plaques and tangles; UBB+1 mutant protein in AD lesions | Immunohistochemistry, western blot |
| Biochemical | Selective decrease in proteasome activity in vulnerable brain regions; Aβ40/42 directly inhibits proteasome | Enzyme activity assays, transmission electron microscopy |
| Genetic | Association between UBQLN1 polymorphisms and AD risk | Genome-wide association studies |
| Oxidative Damage | Oxidation of UCH-L1; accumulation of oxidized proteins | Mass spectrometry, enzyme assays |
The Autophagy-Lysosomal Pathway: Mechanism and Role in AD
ALP Molecular Machinery
Autophagy is a highly conserved lysosome-dependent process for degrading intracellular long-lived proteins, protein aggregates, and organelles [14]. The ALP process involves multiple coordinated steps: initiation, phagophore formation, autophagosome maturation, fusion with lysosomes, and cargo degradation [14].
Autophagy initiation is controlled by the ULK1 complex (ULK1/2, ATG101, ATG13, and FIP200), which is regulated by nutrient-sensing pathways including AMPK and mTORC1 [14]. Nutrient deficiency inhibits mTORC1 and activates AMPK, leading to ULK1 complex activation and autophagy induction [14].
Phagophore formation requires the VPS34/PIK3C3 phosphatidylinositol 3-kinase complex (VPS34, PIK3R4/VPS15, BECN1, ATG14L, and NRBF2), which produces phosphatidylinositol 3-phosphate (PI3P) to recruit downstream autophagy proteins [14].
Autophagosome elongation involves two ubiquitin-like conjugation systems: ATG12-ATG5-ATG16L facilitates the lipidation of microtubule-associated protein 1 light chain 3 (LC3-I to LC3-II), which becomes incorporated into the growing autophagosomal membrane [14].
Cargo degradation occurs after autophagosomes fuse with lysosomes to form autolysosomes, where contents are degraded by lysosomal hydrolases, including cathepsins B and D [18].
ALP Dysfunction in Alzheimer's Pathology
ALP impairment is increasingly recognized as a central contributor to AD pathogenesis. In normal conditions, Aβ is generated intracellularly and degraded via the autophagy-lysosomal system [18]. However, in AD, Aβ overload disrupts this pathway, creating a vicious cycle of impaired clearance and further Aβ accumulation [18]. Lysosomal dysfunction in AD involves multiple factors, including lysosomal membrane permeabilization (particularly with ApoE4), impaired acidification, and reduced cathepsin activity [18].
The relationship between autophagy and tau pathology is equally significant. Hyperphosphorylated tau aggregates, the main component of NFTs, are normally degraded through autophagy [14]. Impaired ALP function contributes to tau accumulation and spread [14] [17]. Recent evidence suggests that soluble tau oligomers, rather than mature NFTs, may be the most toxic species, and these are preferentially cleared by autophagy [14].
Table 2: Autophagy-Lysosomal Pathway Impairments in Alzheimer's Disease
| ALP Component | Nature of Dysfunction | Consequence in AD |
|---|---|---|
| Lysosomal Hydrolases | Reduced activity of cathepsins B and D; impaired acidification | Decreased degradation of Aβ and tau aggregates |
| Lysosomal Membrane | Permeabilization associated with ApoE4 | Leakage of cathepsins into cytosol; oxidative stress |
| Autophagosome Formation | Disrupted vesicle fusion; accumulation of autophagic vacuoles | Impaired clearance of protein aggregates |
| Autophagic Induction | Altered mTORC1/AMPK signaling | Reduced initiation of autophagy under stress |
Advanced Research Technologies and Experimental Approaches
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Clearance Pathways in AD
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Proteasome Activity Assays | Fluorogenic substrates (Suc-LLVY-AMC for chymotrypsin-like activity) | Quantifying proteasome function in tissue extracts or live cells |
| Autophagy Modulators | Rapamycin (inductor), chloroquine (inhibitor), Bafilomycin A1 | Investigating causal relationships between autophagy and protein clearance |
| Lysosomal Function Assays | Lysotracker dyes, cathepsin activity probes, acridine orange | Assessing lysosomal pH, protease activity, and membrane integrity |
| UPS Function Assays | Ubiquitin-protein conjugates antibodies, proteasome inhibitors (MG132) | Monitoring ubiquitination status and UPS-dependent degradation |
| LRP1-Targeted Nanoparticles | Angiopep-2-conjugated polymersomes (A40-POs) | Restoring BBB transport function and enhancing Aβ clearance [21] |
Experimental Protocols for Key Assessments
Protocol 1: Assessing Proteasome Activity in Brain Tissue
- Homogenize fresh or frozen brain tissue in lysis buffer (50 mM Tris-HCl, pH 7.5, 250 mM sucrose, 5 mM MgCl₂, 1 mM DTT, 2 mM ATP)
- Centrifuge at 13,000 × g for 15 minutes at 4°C
- Collect supernatant and determine protein concentration
- Incubate aliquots with fluorogenic substrates: Suc-LLVY-AMC (chymotrypsin-like), Boc-LRR-AMC (trypsin-like), or Z-LLE-AMC (caspase-like)
- Measure fluorescence (excitation 380 nm, emission 460 nm) at 37°C over 60 minutes
- Calculate enzyme activity as fluorescence increase per mg protein per minute [16]
Protocol 2: Evaluating Autophagic Flux Using LC3 Turnover
- Culture cells expressing GFP-LC3 fusion protein or treat primary neurons with autophagy modulators
- Fix cells and immunostain for LC3 using anti-LC3 antibodies
- Quantify LC3 puncta formation per cell using confocal microscopy
- Parallel samples should be treated with lysosomal inhibitors (chloroquine 50-100 μM for 4-6 hours) to block degradation
- Calculate autophagic flux as the difference in LC3-II levels with and without inhibitors using western blot densitometry [14] [17]
Protocol 3: Assessing Aβ Clearance Across BBB Models
- Establish in vitro BBB models using primary brain endothelial cells or cell lines (bEnd.3)
- Seed cells on Transwell filters and confirm barrier integrity (TEER >150 Ω·cm²)
- Add fluorescently-labeled Aβ (e.g., Aβ1-42-Alexa488) to the apical chamber
- Apply experimental treatments (e.g., LRP1-targeted nanoparticles [21])
- Collect samples from basolateral chamber at timed intervals
- Quantify Aβ transport using fluorescence measurements or ELISA
- Confirm LRP1 involvement using receptor-blocking antibodies or siRNA approaches [21]
Signaling Pathways and Cross-Talk Between Clearance Systems
The UPS and ALP do not function in isolation but exhibit extensive cross-talk and coordination. Under normal conditions, the UPS rapidly degrades soluble misfolded proteins, while autophagy handles larger aggregates and organelles [20]. However, when one system becomes impaired, the other may compensate, though this compensatory relationship often fails in neurodegenerative conditions like AD [20].
The following diagram illustrates the key components and regulatory relationships within and between these two clearance systems:
Diagram 1: UPS and ALP Pathways in AD. The diagram shows key components of both clearance systems and their impairment by Aβ and tau pathology. Red arrows indicate inhibitory effects, while blue arrows show activation or sequential steps. Dashed lines represent cross-talk mechanisms.
Emerging Therapeutic Strategies and Research Directions
UPS-Targeted Interventions
Therapeutic strategies targeting the UPS focus primarily on enhancing proteasome activity or reducing the burden of misfolded proteins. Experimental approaches include:
Proteasome activators: Small molecules that enhance proteasome activity show promise in preclinical models but face challenges with specificity and potential off-target effects [19].
E3 ligase modulators: Compounds that regulate specific E3 ligases involved in tau or APP processing could provide more targeted approaches [19].
UPS-ALP combination therapies: Given the cross-talk between degradation systems, combined approaches may prove more effective than single-target interventions [19] [20].
ALP-Targeted Interventions
ALP-directed therapies represent a promising avenue for AD treatment, with multiple strategies in development:
mTOR-independent autophagy inducers: Compounds like metformin and other AMPK activators bypass potential side effects of direct mTOR inhibition [14] [17].
Lysosomal function enhancers: Approaches to improve lysosomal acidification or increase cathepsin activity may enhance degradation capacity without increasing autophagic flux [18].
Transcription factor EB (TFEB) activators: As a master regulator of lysosomal biogenesis, TFEB represents an attractive target for comprehensively enhancing ALP function [17].
Nanotechnology and BBB-Targeted Approaches
Recent groundbreaking research demonstrates a novel nanotechnology approach that repairs blood-brain barrier function to restore Aβ clearance. Supramolecular nanoparticles designed to target low-density lipoprotein receptor-related protein 1 (LRP1) on the BBB act as "avidity-optimized" therapeutics that bias LRP1 trafficking toward transcytosis rather than degradation [22] [21]. This innovative strategy:
- Reduced brain Aβ by 45% within hours of administration
- Restored LRP1 expression and vascular function
- Reversed cognitive deficits in AD mouse models, with benefits lasting at least six months [22] [23] [21]
The following diagram illustrates this novel therapeutic approach and its mechanism of action:
Diagram 2: Nanoparticle-Mediated BBB Repair. This illustrates how LRP1-targeted nanoparticles restore Aβ clearance by biasing receptor trafficking toward transcytosis rather than degradation.
The ubiquitin-proteasome system and autophagy-lysosomal pathway represent complementary protein quality control mechanisms whose dysfunction significantly contributes to Alzheimer's disease pathogenesis. The complex interplay between these systems, along with emerging evidence of vascular clearance mechanisms, highlights the multifactorial nature of protein aggregation in AD. Current research is moving beyond simple activation or inhibition of these pathways toward more nuanced approaches that restore their natural homeostasis and coordination. The promising results from nanotechnology-based BBB repair strategies further underscore the importance of considering extracellular clearance mechanisms alongside intracellular degradation systems. As our understanding of these complex clearance networks deepens, so too does the potential for developing effective therapeutic interventions that target the fundamental protein homeostasis failures underlying Alzheimer's disease.
The efficient clearance of protein aggregates from the brain is a critical determinant in the pathogenesis and progression of Alzheimer's disease (AD). This whitepaper provides a comprehensive technical analysis of the principal clearance pathways, with a specific focus on interstitial fluid bulk flow driven by the glymphatic system, perivascular drainage, and receptor-mediated transport across the blood-brain barrier (BBB) via the Low-Density Lipoprotein Receptor-Related Protein 1 (LRP1) and the Receptor for Advanced Glycation End Products (RAGE). An imbalance in the LRP1/RAGE axis significantly contributes to amyloid-β (Aβ) accumulation. Herein, we synthesize current mechanistic insights, present quantitative data from key studies, detail foundational experimental protocols, and visualize critical pathways and experimental workflows. This resource is designed to equip researchers and drug development professionals with the foundational knowledge and methodologies needed to advance therapeutic strategies targeting protein clearance in neurodegenerative disorders.
The accumulation of toxic protein aggregates, such as amyloid-β (Aβ) and tau in Alzheimer's disease, results not only from overproduction but also from a failure of the brain's clearance mechanisms [24]. The brain, which lacks a conventional lymphatic system, relies on a complex set of specialized pathways to remove metabolic waste. These pathways operate within a functional unit known as the neurovascular unit (NVU), which includes vascular cells (endothelial cells, pericytes), glial cells (astrocytes, microglia), and neurons [24]. Dysfunction of the NVU is an early event in AD, leading to impaired BBB integrity and reduced cerebral blood flow, which in turn hampers the clearance of neurotoxic proteins [24].
The major clearance routes can be categorized as follows:
- The Glymphatic System and Perivascular Drainage: A paravascular network where subarachnoid cerebrospinal fluid (CSF) influx along arterial walls mixes with interstitial fluid (ISF) and solutes, facilitating their clearance along venous pathways.
- Receptor-Mediated Transport at the BBB: A highly regulated exchange of molecules between the blood and the brain, governed by specific influx and efflux receptors on endothelial cells. The LRP1 (efflux) and RAGE (influx) receptors play a particularly pivotal role in Aβ homeostasis.
Understanding the intricate balance and regulation of these pathways is fundamental to developing effective interventions for Alzheimer's disease and other proteinopathies.
Core Transport Mechanisms and Pathway Dysregulation in AD
Interstitial Fluid Bulk Flow and the Glymphatic System
The glymphatic system is a brain-wide clearance pathway that facilitates the efficient removal of solutes and waste, including Aβ. Its function is characterized by a defined directional flow [25]:
- Influx: Subarachnoid CSF enters the brain parenchyma along paravascular spaces surrounding penetrating arteries.
- Exchange: CSF mixes with ISF and solutes in the brain interstitium.
- Efflux: The combined fluid, now containing waste products, is cleared along paravenous drainage pathways.
A critical molecular component of this system is the water channel aquaporin-4 (AQP4), which is densely expressed on astrocytic endfeet ensheathing cerebral vessels. AQP4 supports the bulk fluid flow between influx and efflux routes. Studies in mice lacking AQP4 have demonstrated a ~70% reduction in interstitial solute clearance, underscoring its vital role [25].
Table 1: Experimental Tracer Data in Glymphatic Pathway Studies
| Tracer Molecule | Molecular Weight (Da) | Observation after Intracisternal Injection | Implication for Pathway Function |
|---|---|---|---|
| Alexa Fluor 594 (A594) | 759 | Rapid, widespread movement throughout brain interstitium; minimal concentration in paravascular spaces [25]. | Demonstrates efficient parenchymal exchange and bulk flow of small solutes. |
| Texas Red-dextran-3 (TR-d3) | 3,000 | Concentrated in paravascular spaces but also entered the interstitium [25]. | Highlights the sieving function of astrocytic endfeet; intermediate-sized solutes can access the interstitium. |
| FITC-dextran-2000 | 2,000,000 | Confined to paravascular spaces; did not enter the surrounding interstitial space [25]. | Illustrates the size-dependent exclusion from the parenchyma; very large molecules are restricted to the paravascular influx route. |
| FITC-dextran-70 | 70,000 | Used to label and quantify perivascular spaces (PVS); more readily observed around arteries than veins [26]. | Provides a tool for visualizing the anatomical substrate of the glymphatic system and its asymmetry between arterial and venous sides. |
Perivascular Drainage and Intramural Clearance
An alternative or complementary model to the glymphatic system is the Intramural Peri-Arterial Drainage (IPAD) pathway. This model proposes that solutes, including Aβ, are cleared from the brain along the basement membranes within the walls of cerebral arteries [26]. The driving forces for this clearance are believed to include arterial pulsatility. Recent in vivo studies in mice have shown that the perivascular spaces around arteries are significantly larger and more frequently labeled by CSF tracers than those around veins, suggesting a preferential role for arteries in the influx and drainage of fluids [26]. The exact anatomical location of the drainage route—whether within the arterial wall (intramural) or directly adjacent to it (extramural)—remains a subject of ongoing investigation, but both views acknowledge the primacy of arterial pathways in solute clearance [26].
Receptor-Mediated BBB Transport: The LRP1/RAGE Axis
The BBB is a highly selective barrier formed by endothelial cells connected by tight junctions, pericytes, astrocytes, and a basement membrane [27] [28] [29]. It tightly controls molecular exchange between blood and brain via several mechanisms, with receptor-mediated transcytosis being critical for larger molecules like Aβ.
Table 2: Key Receptors in Amyloid-β Transport at the Blood-Brain Barrier
| Receptor | Primary Direction of Transport | Role in Aβ Metabolism | Expression Change in AD |
|---|---|---|---|
| LRP1(Low-Density Lipoprotein Receptor-Related Protein 1) | Brain-to-Blood (Efflux) [24] | Binds to and mediates the cellular clearance of Aβ from the brain across the BBB into the circulation [30] [24]. | Decreased expression in endothelial cells, reducing Aβ clearance and contributing to accumulation [24]. |
| RAGE(Receptor for Advanced Glycation End products) | Blood-to-Brain (Influx) [24] | Binds circulating Aβ and facilitates its transport across the BBB into the brain, also mediating Aβ-induced oxidative stress and neuroinflammation [24]. | Increased expression in endothelial cells, leading to greater influx of Aβ into the brain [24]. |
| P-gp(P-glycoprotein) | Brain-to-Blood (Efflux) [24] | An ATP-dependent efflux pump that works alongside LRP1 to remove Aβ and other toxins from the brain [24]. | Deficient expression, contributing to reduced Aβ clearance [24]. |
The opposing actions of LRP1 and RAGE create a critical equilibrium at the BBB. In the healthy brain, this system maintains low levels of Aβ. In AD, the system becomes dysregulated, with decreased LRP1 and increased RAGE expression, creating a vicious cycle of Aβ accumulation and neuroinflammation [24]. LRP1's role is complex and extends beyond Aβ clearance; it also interacts with apoE, the strongest genetic risk factor for AD, and is involved in maintaining overall brain homeostasis [30]. It is important to note that LRP1's function may be disease-specific, as its deletion has been reported to be protective in Parkinson's disease models by reducing the transmission of α-synuclein [31].
Quantitative Data and Experimental Models
Key Quantitative Findings
- Glymphatic Flow Rate: Approximately 40% of intracisternally injected [³H]mannitol (182 Da) tracer was recovered in the brain within 45 minutes, demonstrating substantial CSF influx, while the larger [³H]dextran-10 (10 kDa) accumulated more slowly [25].
- AQP4 Dependence: Genetic deletion of Aqp4 in mice results in a ~70% reduction in the clearance of interstitial solutes, including soluble Aβ [25].
- Perivascular Space Dimensions: In vivo imaging in mice reveals that the perivascular spaces (PVS) around pial arteries are significantly larger than those around pial veins. The size of the PVS correlates with blood vessel diameter for pial vessels but not for penetrating vessels [26].
- LRP1 Genetic Association: A meta-analysis of 18 case-control studies (4,668 AD patients and 4,473 controls) found no overall significant effect of the LRP1 C766T polymorphism on AD risk. However, subsequent studies suggest its effect may be modified by other factors, such as tau pathology, or be associated with specific Aβ deposition patterns like cerebral amyloid angiopathy (CAA) [30].
In Vivo and In Vitro BBB Transport Models
Understanding the permeability of the BBB is crucial for drug development. Several experimental models are used to study this.
Table 3: Experimental Models for Studying BBB Transport
| Model Type | Description | Key Applications & Measurable Outputs |
|---|---|---|
| In Vivo Permeability Studies | Direct injection of tracers or drugs into the bloodstream or CSF of live animals (e.g., mice), followed by measurement of brain uptake [25] [29]. | - CSF Influx: Intracisternal injection of fluorescent or radiolabeled tracers to track paravascular flow [25].- Blood-to-Brain Permeability: Intravenous injection with subsequent analysis of brain homogenates to calculate permeability coefficients (e.g., Permeability-Surface Area product) [29]. |
| In Vitro Cell-Based Models | Culture of brain endothelial cells on permeable transwell filters, often in co-culture with astrocytes or pericytes to improve barrier properties [29]. | - Transepithelial Electrical Resistance (TEER): Measures the tightness of the cell monolayer [29].- Permeability Coefficient (Papp): Quantifies the rate of solute flux across the cell layer [29]. |
| Mathematical Transport Models | Computational models that simulate the diffusion and transport of molecules across the BBB based on physicochemical properties (e.g., molecular weight, lipophilicity) and anatomical parameters [29]. | - Predicting Drug Permeability: In silico screening of compound libraries for BBB penetration potential [32]. |
Detailed Experimental Protocols
Protocol: In Vivo Tracer Imaging of Paravascular CSF Influx
This protocol, adapted from Iliff et al. [25], details the procedure for real-time visualization of CSF tracer movement in the mouse brain.
Key Research Reagents:
- Anesthetics: Ketamine and Dexmedetomidine for induction and maintenance.
- Fluorescent Tracers: FITC-dextran (40-2000 kDa, for CSF) and Texas Red-dextran-70 (70 kDa, for blood plasma).
- Artificial CSF (aCSF): Ionic solution mimicking natural CSF.
- Surgical Equipment: Stereotactic frame, dental drill, glass cover slip.
Procedure:
- Animal Preparation and Cranial Window: Anesthetize a mouse and secure it in a stereotactic frame. Perform a craniotomy by carefully drilling and removing a ~3 mm diameter circle of skull above the region of interest (e.g., the middle cerebral artery), leaving the dura intact. Seal the opening with a glass coverslip [25] [26].
- Tracer Injection: Inject FITC-labeled dextran (in aCSF) into the cisterna magna at a slow, controlled rate (e.g., 1 µl/min) to label the CSF. Simultaneously or subsequently, inject Texas Red-dextran-70 intravenously (e.g., via retro-orbital injection) to label the blood plasma and visualize the vasculature [25] [26].
- In Vivo Two-Photon Imaging: Place the animal under a two-photon microscope. Using a water-immersion objective, image the cortical surface and parenchyma to depths of ~200 µm. Use appropriate excitation wavelengths (e.g., 790 nm for FITC, 910 nm for Texas Red) to track the movement of the CSF tracer in real-time.
- Data Analysis: Analyze the time-lapse image stacks to determine the kinetics of para-arterial CSF influx, the distribution of tracer between paravascular spaces and the interstitium, and the size of perivascular spaces relative to the accompanying vessel [25] [26].
Protocol: Assessing BBB Permeability to Amyloid-β
This protocol outlines methods to evaluate the functional role of LRP1 and RAGE in Aβ transport across the BBB.
Key Research Reagents:
- Radiolabeled or Fluorescently-Tagged Aβ peptides: (e.g., ¹²⁵I-Aβ40, FITC-Aβ42).
- Receptor-Specific Modulators: RAGE inhibitors (e.g., FPS-ZM1), LRP1 antagonists (e.g., RAP - Receptor-Associated Protein).
- Transwell Assay Systems: Permeable supports for in vitro BBB models.
- Antibodies: For immunohistochemistry or Western blot analysis of LRP1, RAGE, and tight junction proteins (e.g., occludin, claudin-5).
Procedure: In Vitro Transwell Assay:
- Culture a monolayer of brain endothelial cells (e.g., bEnd.3 cells or primary human BMVECs) on a transwell insert until a high TEER value is achieved.
- Apply the tagged Aβ peptide to the "luminal" (top) or "abluminal" (bottom) chamber in the presence or absence of receptor modulators.
- At timed intervals, sample from the opposite chamber and quantify the tracer that has crossed the cell layer using a gamma counter (for radioactive tracers) or a fluorometer.
- Compare transport rates between treatment groups to infer the contribution of LRP1 (efflux) or RAGE (influx) to Aβ translocation [24] [29].
In Vivo Brain Efflux Index (BEI):
- Anesthetize a rat or mouse and place it in a stereotactic frame.
- Inject a small volume of a solution containing the tagged Aβ peptide (and a reference compound) directly into a specific brain region (e.g., hippocampus or cortex).
- At designated time points, collect blood from the superior sagittal sinus and/or decapitate the animal to collect the brain.
- Measure the amount of tracer remaining in the brain and the amount that has appeared in the blood. The percentage of Aβ cleared from the brain over time provides a measure of efflux capacity, which can be compared between wild-type and genetically modified animals or after pharmacological blockade of LRP1 [29].
Pathway and Workflow Visualizations
The Glymphatic Pathway and LRP1/RAGE Axis in Alzheimer's Disease
Experimental Workflow for Investigating Perivascular Drainage
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Models for Investigating Brain Clearance Pathways
| Reagent / Model | Specification / Example | Primary Function in Research |
|---|---|---|
| Fluorescent Dextrans | FITC-, TRITC-, or Alexa Fluor-conjugated; 3 kDa - 2,000 kDa [25] [26]. | Size-dependent tracers for visualizing paravascular CSF influx, interstitial diffusion, and defining the functional limits of the glymphatic system. |
| AQP4 Knockout Mice | Genetically modified mouse model lacking aquaporin-4 water channels [25]. | To definitively establish the role of AQP4 in glymphatic fluid flow and solute clearance, and to study its contribution to Aβ pathology. |
| LRP1 Modulators | Receptor-Associated Protein (RAP) - a universal LRP1 antagonist [30]. | To pharmacologically inhibit LRP1 function in vitro or in vivo, allowing researchers to dissect its specific role in Aβ efflux transport. |
| RAGE Inhibitors | Small-molecule antagonists like FPS-ZM1. | To block RAGE-mediated Aβ influx and neuroinflammatory signaling, assessing its therapeutic potential and validating its role in AD pathogenesis. |
| In Vitro BBB Models | Transwell cultures of brain endothelial cells (primary or immortalized), often co-cultured with astrocytes [29]. | To perform controlled, reductionist studies of transporter function (LRP1/RAGE), tight junction integrity, and compound permeability without the complexity of a whole organism. |
| Dynamic Contrast-Enhanced MRI (DCE-MRI) | Used in clinical and preclinical research with Gadolinium-based contrast agents [24]. | A non-invasive method to quantify BBB leakage and permeability in living subjects, allowing for longitudinal studies of NVU dysfunction in disease progression. |
The brain employs a multi-faceted clearance system, encompassing the glymphatic flow, perivascular drainage, and receptor-mediated BBB transport, to prevent the accumulation of proteotoxic waste. The dysregulation of these pathways, particularly the opposing LRP1 and RAGE functions at the BBB, is a hallmark of Alzheimer's disease pathology. A deep and quantitative understanding of these mechanisms—their kinetics, regulatory factors, and interactions—is paramount. The experimental methodologies and reagents detailed in this whitepaper provide a foundation for ongoing research. Future therapeutic success will likely depend on integrated strategies that co-target multiple clearance pathways to restore the brain's innate ability to remove protein aggregates and maintain homeostasis.
The progressive accumulation of protein aggregates is a defining pathological feature of Alzheimer's disease (AD). Glial cells, particularly microglia and astrocytes, serve as crucial regulators of brain proteostasis through specialized clearance mechanisms. This whitepaper examines the sophisticated phagocytic and degradative pathways employed by these cells to manage amyloid-β (Aβ) and other pathological proteins. We synthesize current understanding of how microglial phagocytosis and astrocytic clearance mechanisms become dysregulated during AD progression, creating a permissive environment for protein aggregation. The document further explores emerging therapeutic strategies aimed at modulating glial functions to restore proteostatic balance, with particular emphasis on targets currently under investigation for drug development. By integrating recent genetic, molecular, and clinical findings, this review provides a comprehensive technical resource for researchers and drug development professionals working to translate glial biology into effective neurodegenerative disease therapeutics.
Alzheimer's disease pathophysiology is characterized by the accumulation of misfolded proteins, primarily amyloid-β (Aβ) and tau, which aggregate into oligomers, fibrils, and ultimately mature plaques and tangles [1]. The brain maintains a delicate balance between protein production and clearance, with glial cells playing an indispensable role in this proteostatic regulation [33] [34]. When these clearance mechanisms become impaired—whether through aging, genetic risk factors, or chronic inflammatory responses—the resulting protein accumulation initiates a destructive cascade that includes synaptic dysfunction, neuroinflammation, and ultimately neuronal loss [35] [4].
Microglia and astrocytes employ complementary strategies for protein clearance. As the resident immune cells of the central nervous system (CNS), microglia function as professional phagocytes, capable of engulfing Aβ plaques, cellular debris, and synapses [36]. Astrocytes contribute to proteostasis through both enzymatic degradation and facilitator roles in Aβ transport across the blood-brain barrier [33] [34]. The coordinated efforts of these glial populations normally prevent protein accumulation; however, in AD, both cell types undergo functional alterations that transform them from protective to potentially pathogenic entities [36] [37]. Understanding the molecular mechanisms governing glial clearance pathways provides critical insights for developing targeted therapies aimed at restoring proteostatic balance in the AD brain.
Microglial Phagocytosis in Alzheimer's Disease
Phagocytic Mechanisms and Receptor-Mediated Clearance
Microglia constantly survey the CNS microenvironment, recognizing and phagocytosing misfolded proteins, cellular debris, and apoptotic cells through an array of specialized receptors [36]. The phagocytosis process occurs in three distinct phases: (1) the "find-me" phase involving chemotaxis toward apoptotic or damaged cells; (2) the "eat-me" phase comprising recognition and engulfment of targets; and (3) the "digest-me" phase involving enzymatic degradation of engulfed content within phagolysosomes [36].
Table 1: Key Microglial Phagocytosis Receptors in Alzheimer's Disease
| Receptor | Primary Ligand(s) | Biological Function | Role in AD |
|---|---|---|---|
| TREM2 | Apolipoproteins, Aβ | Chemotaxis, cell survival, phagocytic activation | Reduced function increases AD risk; role in Aβ compaction |
| LRP1 | Aβ, apolipoproteins | Aβ uptake and degradation | Clearance of Aβ aggregates |
| CD33 | Sialic acid residues | Inhibitory receptor dampening phagocytosis | Increased AD risk; reduces Aβ uptake |
| TAM Receptors (Tyro3, Axl, Mer) | Gas6, Protein S | Phagocytosis of apoptotic cells, Aβ plaque detection | Aβ plaque clearance; efferocytosis |
| P2Y6 | UDP | Phagocytosis of apoptotic neurons | Mediates microglial chemotaxis toward damage |
| Complement Receptors (CR3, CR4) | C3b, iC3b | Phagocytosis of opsonized targets | Excessive synaptic pruning in AD |
| Scavenger Receptors (e.g., SR-A, CD36) | Aβ fibrils, oxidized lipids | Aβ binding and uptake | Clearance of fibrillar Aβ |
During the "find-me" phase, nucleotides such as UDP and ATP released by damaged neurons act as potent chemoattractants by activating microglial P2Y6 receptors [36]. TREM2 (Triggering Receptor Expressed on Myeloid Cells 2) plays an essential role in microglial chemotaxis toward neuronal injury and non-inflammatory clearance of apoptotic neurons [36]. In the subsequent "eat-me" phase, surface-exposed phosphatidylserine on apoptotic cells is recognized by receptors including TREM2, complement receptors, and TAM family receptors (Tyro3, Axl, Mer), initiating engulfment [36] [37]. The "digest-me" phase culminates in the lysosomal degradation of internalized cargo, with cathepsin B playing a significant role in processing longer forms of Aβ into less toxic species [33].
Genetic Regulation of Phagocytic Function
Genome-wide association studies have revealed that many genes associated with increased AD risk are predominantly expressed in microglia and regulate phagocytic function [35]. These include TREM2, CD33, CR1, ABCA1, and INPP5D, among others [35]. The identification of these genetic risk factors provides compelling evidence for the central role of microglial phagocytosis in AD pathogenesis.
The TREM2 pathway is particularly crucial, as rare variants significantly increase AD risk [35] [36]. TREM2 supports microglial survival, activation, and phagocytic capacity, with its ligands including apolipoproteins and Aβ itself [36]. Upon ligand binding, TREM2 associates with the adaptor protein DAP12 to initiate downstream signaling through SYK kinase, which promotes cytoskeletal reorganization necessary for phagocytosis and activates transcriptional programs that enhance degradative capacity [35]. CD33 represents another critical immunomodulatory receptor, acting as an inhibitory checkpoint that dampens Aβ phagocytosis when engaged by sialic acid-containing glycans [35]. The balanced signaling between activating receptors like TREM2 and inhibitory receptors like CD33 fine-tunes microglial phagocytic activity in the AD brain.
Dual Roles in Neuroprotection and Neurotoxicity
Microglial phagocytosis serves paradoxically both protective and detrimental functions in AD, largely dependent on the disease stage and specific cellular targets [35]. During early disease phases, microglial phagocytosis of Aβ via TREM2, LRP1, and TAM receptors helps restrict plaque expansion and compact existing plaques, thereby limiting subsequent tau pathology [35]. This protective phagocytosis creates a physical barrier that sequesters toxic Aβ species and reduces neuritic damage.
However, in later disease stages, microglial phagocytosis becomes detrimental through excessive engulfment of synaptic structures and potentially even live neurons [35] [37]. Complement proteins C1q and C3 are deposited on synapses, marking them for elimination by microglial complement receptors [37]. This complement-mediated synaptic pruning, while essential during development, becomes pathological in the AD brain, contributing significantly to synaptic loss and cognitive decline [35] [37]. Additional receptors including P2Y6 and TREM2 itself may also mediate this excessive phagocytosis of synapses and neurons, highlighting the complex duality of these pathways [35].
Astrocytic Clearance Mechanisms
Enzymatic Degradation Pathways
Astrocytes contribute significantly to Aβ clearance through the production and secretion of a diverse array of proteolytic enzymes that degrade Aβ in the extracellular space [33] [34]. These enzymes target different cleavage sites within the Aβ sequence, generating fragments with reduced aggregation propensity and neurotoxicity.
Table 2: Major Astrocytic Aβ-Degrading Enzymes in Alzheimer's Disease
| Enzyme Class | Specific Enzymes | Aβ Species Targeted | Cellular Localization |
|---|---|---|---|
| Metalloendopeptidases | Neprilysin (NEP), Insulin Degrading Enzyme (IDE), Endothelin-Converting Enzyme (ECE) | Monomeric Aβ (NEP also cleaves oligomers) | Extracellular space, cell membrane |
| Matrix Metalloproteinases | MMP-2, MMP-9 | Monomeric and fibrillar Aβ | Extracellular space |
| Lysosomal Peptidases | Cathepsin B (CAT-B) | Phagocytosed Aβ, longer Aβ forms | Intracellular lysosomes |
| Plasminogen Activators | Tissue Plasminogen Activator (tPA) | Aggregated Aβ | Extracellular space |
| Other Proteases | Angiotensin-Converting Enzyme (ACE) | Aggregated Aβ | Extracellular space |
Neprilysin (NEP) and insulin-degrading enzyme (IDE) represent the most extensively characterized Aβ-degrading proteases [33] [34]. Both enzymes are metalloendopeptidases that cleave monomeric Aβ species, with NEP also demonstrating activity against oligomeric forms [33]. The significance of these enzymes is substantiated by animal models where genetic deletion of NEP or IDE exacerbates Aβ deposition, while their overexpression reduces Aβ burden [33]. Matrix metalloproteinases (MMPs), particularly MMP-2 and MMP-9 secreted by astrocytes, contribute to the extracellular degradation of both monomeric and fibrillar Aβ forms [33]. Astrocyte-conditioned medium demonstrates Aβ-degrading activity that is significantly attenuated by MMP inhibitors or when derived from MMP-deficient mice [33].
Receptor-Mediated Clearance and Chaperone Functions
Beyond enzymatic degradation, astrocytes actively participate in Aβ clearance through receptor-mediated endocytosis and transporter-facilitated removal from the CNS [33] [34]. Astrocytes express several receptors capable of binding Aβ, including lipoprotein receptor-related protein 1 (LRP1), scavenger receptors, receptor for advanced glycation end products (RAGE), and formyl peptide receptors [34]. Following internalization, Aβ is trafficked to lysosomes where cathepsin B and other hydrolases complete its degradation [33].
Astrocytes also release extracellular chaperones that sequester Aβ and facilitate its transport across the blood-brain barrier [33] [34]. Key chaperones include apolipoprotein E (ApoE), apolipoprotein J (clusterin), α2-macroglobulin, and α1-antichymotrypsin [33]. These chaperones form complexes with Aβ that interact with transporters such as LRP1 on the abluminal side of cerebral endothelial cells, enabling Aβ efflux from the brain to the peripheral circulation [33]. The ApoE isoform (ApoE4) associated with highest AD risk demonstrates impaired Aβ binding and clearance compared to ApoE2 and ApoE3, providing a mechanistic link between this genetic risk factor and Aβ accumulation [33].
Experimental Models and Methodologies
In Vivo and In Vitro Assessment of Phagocytosis
The investigation of glial phagocytic function employs a diverse methodological toolkit spanning in vivo imaging, ex vivo histological analysis, and in vitro assays. Two-photon intravital microscopy enables real-time observation of microglial dynamics and phagocytic activity in living animals [36]. This approach has revealed that even "resting" microglia continuously extend and retract processes to survey their microenvironment, making frequent contacts with synapses [36].
For quantitative assessment of phagocytic capacity, primary microglial and astrocytic cultures exposed to fluorescently-labeled Aβ, synaptosomes, or apoptotic cells provide a controlled system for measuring engulfment [36]. Internalization is typically quantified by flow cytometry or confocal microscopy following careful removal of surface-bound (non-internalized) targets using trypsinization or acid washes [36]. To determine the fate of ingested cargo, pH-sensitive fluorophores (e.g., pHrodo) can distinguish internalized materials within acidic phagolysosomes from those merely attached to the cell surface [37].
Table 3: Key Experimental Approaches for Studying Glial Phagocytosis
| Method Category | Specific Techniques | Key Readouts | Considerations |
|---|---|---|---|
| In Vivo Imaging | Two-photon microscopy, PET imaging | Microglial dynamics, plaque clearance, synaptic engulfment | Real-time assessment in physiological context |
| Ex Vivo Analysis Immunohistochemistry, RNA sequencing | Receptor localization, transcriptomic profiles, plaque load | Preserved tissue architecture but static snapshot | |
| In Vitro Phagocytosis Assays | Flow cytometry, confocal microscopy with pH-sensitive dyes | Quantification of internalized targets, degradation kinetics | Controlled environment but lacks full physiological complexity |
| Genetic Manipulation | CRISPR/Cas9, siRNA, transgenic models | Functional validation of specific genes | Establishes causality but may require compensatory mechanisms |
| Human Tissue Models | iPSC-derived microglia/astrocytes, cerebral organoids | Human-specific pathways, patient-specific effects | Relevance to human disease but variable differentiation efficiency |
Genetic approaches including CRISPR/Cas9-mediated gene editing, siRNA knockdown, and analysis of transgenic models enable functional validation of specific phagocytosis receptors and signaling components [35] [36]. The emergence of human induced pluripotent stem cell (iPSC)-derived microglia and astrocytes provides platforms for investigating human-specific phagocytic pathways and patient-specific effects [35]. These human cell models can be exposed to brain substrates including Aβ plaques or tau fibrils to examine transcriptional and functional responses under controlled conditions [35].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Glial Phagocytosis
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| Phagocytosis Reporters | pHrodo-labeled Aβ, fluorescent synaptosomes, apoptotic cells | Quantifying internalization and degradation | pH-sensitive fluorophores signal only upon phagolysosomal acidification |
| Receptor Agonists/Antagonists | TREM2 agonists, CD33 blocking antibodies, P2Y6 receptor ligands | Modulating specific phagocytic pathways | Determine receptor necessity and sufficiency |
| Genomic Tools | CRISPR/Cas9 for phagocytosis genes, scRNA-seq, RNAi | Identifying and validating genetic regulators | Single-cell sequencing reveals cellular heterogeneity |
| Cell Type-Specific Markers | IBA1 (microglia), GFAP (astrocytes), C1q (complement) | Identifying and quantifying glial populations | Multiple markers recommended for accurate identification |
| Animal Models | 5XFAD, APP/PS1, Trem2 KO, Cd33 KO | In vivo functional studies | Models vary in pathology progression and completeness of phenotypic replication |
Critical reagents for phagocytosis research include fluorescent probes that distinguish internalized targets, with pHrodo-labeled Aβ and synaptosomes being particularly valuable as their fluorescence intensifies upon phagolysosomal acidification [36] [37]. Receptor-specific agonists and antagonists allow pharmacological dissection of individual pathways, exemplified by TREM2 agonistic antibodies, CD33 blocking antibodies, and P2Y6 receptor ligands like UDP [35] [36]. Genomic tools including CRISPR/Cas9 systems optimized for primary glia enable targeted manipulation of phagocytosis-related genes, while single-cell RNA sequencing reveals transcriptomic signatures associated with different phagocytic states [35] [36]. Animal models ranging from conventional transgenics (e.g., 5XFAD, APP/PS1) to knockout strains (e.g., Trem2 KO, Cd33 KO) provide in vivo systems for evaluating phagocytic function throughout disease progression [35].
Visualization of Key Phagocytosis Signaling Pathways
Figure 1: Microglial Phagocytosis Signaling Pathways. This diagram illustrates the principal "find-me," "eat-me," and "don't-eat-me" signals regulating microglial phagocytosis in Alzheimer's disease. "Find-me" signals (yellow) including UDP/ATP and CX3CL1 promote microglial activation through receptors such as P2Y6 and CX3CR1. "Eat-me" signals (red) such as phosphatidylserine and complement proteins engage TAM receptors, TREM2, and complement receptors to initiate phagocytosis via SYK-dependent signaling and cytoskeletal reorganization. "Don't-eat-me" signals (white/gray) including CD47 and SRPX2 inhibit excessive phagocytosis through receptors like SIRPα and C1q inhibition.
Figure 2: Astrocytic Aβ Clearance Mechanisms. This diagram outlines the four primary pathways through which astrocytes clear amyloid-β: (1) Extracellular enzymatic degradation via proteases including neprilysin (NEP), insulin-degrading enzyme (IDE), matrix metalloproteinases (MMPs), and angiotensin-converting enzyme (ACE); (2) Receptor-mediated uptake through LRP1, scavenger receptors, RAGE, and formyl peptide receptors; (3) Intracellular degradation within lysosomes via cathepsin B and endothelin-converting enzyme (ECE); (4) Transporter-mediated clearance across the blood-brain barrier following complex formation with chaperones like ApoE and clusterin.
Therapeutic Implications and Future Directions
The central role of glial phagocytosis in AD pathogenesis has positioned these cells as promising therapeutic targets. Current approaches aim to enhance beneficial clearance while minimizing detrimental phagocytic activity [35] [36]. The most advanced strategy involves anti-Aβ antibodies, which act as opsonins that enhance microglial phagocytosis and clearance of Aβ aggregates [35]. These antibodies, including aducanumab, lecanemab, and donanemab, demonstrate that increasing microglial phagocytosis of amyloid plaques can moderately slow clinical decline in early AD patients [35].
Future therapeutic development focuses on more precise modulation of specific phagocytic pathways. TREM2 agonism represents a leading approach to enhance microglial survival, chemotaxis toward plaques, and Aβ clearance capacity [35] [36]. Conversely, CD33 inhibition may relieve phagocytic repression and increase Aβ uptake [35]. Complement pathway inhibition, particularly targeting C1q or C3, aims to reduce excessive synaptic pruning while preserving beneficial functions [37]. Additional strategies include enhancing astrocytic degradative capacity through upregulation of NEP or IDE, and modulating astrocytic phenotype to reduce neuroinflammatory responses [33] [34].
The development of these targeted therapies faces significant challenges, including the need for precise temporal intervention and cell-specific delivery to avoid disrupting essential phagocytic functions in other tissues [35] [36]. Future research directions should prioritize better understanding of how glial phagocytic function changes throughout AD progression, identifying biomarkers of phagocytic competence, and developing compounds that can selectively modulate specific phagocytic pathways without inducing widespread immune activation [35] [36] [37]. The integration of human iPSC-derived glia, advanced animal models, and multi-omics technologies will accelerate the translation of basic phagocytosis research into effective clinical interventions for Alzheimer's disease and related protein aggregation disorders.
Microglial phagocytosis and astrocytic clearance mechanisms represent essential components of the brain's protein quality control system. In Alzheimer's disease, the dysregulation of these glial functions contributes significantly to the accumulation of Aβ and other pathological proteins. The dual nature of glial phagocytosis—serving both protective and detrimental roles—underscores the therapeutic challenge of selectively enhancing beneficial functions while suppressing harmful ones. Emerging insights from genetic studies, molecular profiling, and clinical trials continue to refine our understanding of these complex processes. As drug development efforts increasingly target glial clearance pathways, the potential grows for transformative therapies that modify disease progression by restoring proteostatic balance in the Alzheimer's brain.
The efficient clearance of protein aggregates is a critical determinant in the pathogenesis of Alzheimer's disease (AD). Genetic factors, most notably APOE and TREM2, profoundly influence the cellular mechanisms responsible for clearing amyloid-β (Aβ) and tau pathologies. This whitepaper synthesizes current research to delineate how specific risk variants impair microglial function, astrocytic support, and overall clearance pathways. Understanding these genotype-driven impairments provides a foundational framework for developing genetically-informed therapeutic strategies aimed at restoring proteostatic balance in the AD brain.
In neurodegenerative diseases like Alzheimer's, the accumulation of protein aggregates such as amyloid-β plaques and neurofibrillary tangles represents a failure of clearance mechanisms rather than solely overproduction. The brain employs multiple pathways for protein clearance, including microglial phagocytosis, autophagic processes, and receptor-mediated endocytosis. The efficiency of these systems is not uniform across individuals but is significantly modulated by genetic background. This review focuses on the central roles of APOE, TREM2, and related genetic factors in regulating these clearance mechanisms, framing them within the broader context of protein aggregation clearance pathways in AD research.
Key Genetic Regulators of Clearance Efficiency
APOE: The Master Lipid Coordinator and Clearance Modulator
The APOE gene encodes apolipoprotein E, a lipid-transport protein essential for cholesterol metabolism and neuronal repair in the brain. Its three major isoforms—APOE2, APOE3, and APOE4—differ by single amino acid substitutions that dramatically alter their structure and function [38].
- Isoform-Specific Clearance Efficiency: The APOE isoforms demonstrate a clear hierarchy in AD risk and clearance capability. APOE4 constitutes the strongest genetic risk factor for late-onset AD, while APOE2 is protective [38]. This risk profile is directly linked to differential efficacy in clearing amyloid-β peptides.
- Structural Basis of Function: APOE is a 299-amino acid glycoprotein with two primary domains: an N-terminal receptor-binding domain and a C-terminal lipid-binding domain. The APOE4 isoform, with arginine at both positions 112 and 158, exhibits a characteristic domain interaction that alters its lipid-binding properties and receptor interactions compared to APOE2 and APOE3 [38].
- Mechanisms of Clearance Impairment: APOE4 is associated with reduced stability and impaired receptor binding, leading to deficient clearance of Aβ aggregates. Specifically, APOE4 shows impaired binding to LRP1, a key receptor involved in the endocytic clearance of Aβ, resulting in enhanced AD pathology [38]. Furthermore, APOE4 exacerbates tau pathology, neuroinflammation, and compromises cerebrovascular integrity, creating an environment hostile to efficient clearance.
Table 1: APOE Isoform Characteristics and Clearance Implications
| Isoform | Amino Acid Positions | AD Risk Relative to E3/E3 | Key Clearance Impairments |
|---|---|---|---|
| APOE2 | Cys112, Cys158 | ~99% risk reduction [39] | Elevated plasma levels but not linked to clearance deficits |
| APOE3 | Cys112, Arg158 | Neutral (reference) | Optimal receptor interactions and clearance function |
| APOE4 | Arg112, Arg158 | ~3-4x (1 copy); ~10-12x (2 copies) [40] | Impaired LRP1 binding, reduced Aβ clearance, exacerbated tau pathology |
TREM2: The Microglial Activation Gateway
TREM2 (Triggering Receptor Expressed on Myeloid cells 2) is a transmembrane receptor primarily expressed on microglia that regulates their survival, proliferation, and phagocytic activity. Multiple TREM2 variants (e.g., R47H, R62H) significantly increase the risk for late-onset AD, frontotemporal dementia, and other neurodegenerative disorders [41].
- Role in Microglial Function: TREM2 is essential for the transition of microglia from a homeostatic to a disease-associated microglia (DAM) phenotype. This transition is crucial for microglia to cluster around amyloid plaques and perform effective phagocytic clearance of Aβ and cellular debris [41] [42].
- Ligand Interactions: TREM2 binds to a diverse array of ligands, including anionic lipids, APOE, and Aβ itself. The interaction between TREM2 and APOE is particularly critical; it regulates the lipid environment around Aβ plaques and enhances microglial Aβ clearance ability [41].
- Consequences of TREM2 Dysfunction: Pathogenic mutations in TREM2 (e.g., R47H) impair ligand binding, protein folding, and trafficking. This leads to reduced microglial activation and a diminished ability to clear amyloid aggregates, exacerbating neuroinflammatory responses and accelerating disease progression [41] [42]. Furthermore, TREM2 deficiency impairs microglial synaptic clearance, potentially contributing to synaptic loss in AD [43].
Table 2: Key TREM2 Pathogenic Variants and Functional Consequences
| Variant | Domain | AD Risk (Odds Ratio) | Primary Functional Deficits |
|---|---|---|---|
| R47H | Immunoglobulin | ~3-fold increase [40] | Impaired ligand binding (lipids, APOE), reduced phagocytosis |
| R62H | Immunoglobulin | ~2-fold increase [41] | Altered protein folding and trafficking |
| H157Y | Stalk (Cleavage site) | Increased risk [41] | Enhanced TREM2 shedding, disrupted signaling |
| T66M | Immunoglobulin | Associated with NHD [41] | Severe disruption of microglial function |
Synergistic Interactions Between APOE and TREM2
APOE and TREM2 do not operate in isolation; they function in a tightly coordinated pathway that regulates microglial response to pathology.
- Co-regulation of Microglial States: Single-nucleus RNA sequencing of human post-mortem brain tissue reveals that both APOE and TREM2 risk variants are associated with a significant reduction in a specific microglial subpopulation termed amyloid-responsive microglia (ARM). These CD163-positive ARM are depleted in carriers of APOE4 and TREM2 risk variants, indicating a convergent mechanism where genetic risk impairs the necessary microglial response to amyloid deposition [40].
- APOE as a TREM2 Ligand: APOE is a putative ligand for TREM2. The TREM2-APOE interaction drives the transcriptional reprogramming of microglia into the DAM phenotype, which is essential for effective aggregate clearance [43]. The APOE-TREM2 axis is therefore a critical regulatory node; its disruption by risk variants like APOE4 and TREM2 R47H stalls the microglial response, allowing for unchecked accumulation of Aβ [42].
Quantitative Impact of Genetic Risk
The individual and collective impact of these genetic risk factors can be quantified in terms of disease burden. Recent research has introduced an approach to estimate their effect on disability-adjusted life years (DALYs), or "lost healthy life years" [44].
- APOE4 Impact: Carrying the high-risk APOE ε4/ε4 haplotype, compared to the neutral ε3/ε3 haplotype, results in 2.48 attributable DALYs (95% CI: 2.28–2.68). This effect is driven predominantly by a dramatic increase in the risk of Alzheimer's disease and other dementias (Hazard Ratio = 5.97) [44].
- Polygenic Risk: The cumulative impact of many common genetic variants, expressed as a polygenic risk score, can also be significant. For instance, being in the top 10% of a polygenic score for multisite chronic pain had an effect of 3.63 DALYs, highlighting how aggregated small effects can translate into a substantial health burden [44].
Experimental Models and Methodologies for Studying Clearance
Understanding the mechanistic influence of APOE and TREM2 has been advanced by sophisticated in vivo and in vitro models.
Inducible APOE Switch Model
A groundbreaking knock-in mouse model (APOE4s2) allows for a tamoxifen-inducible 'switch' from the risk-associated APOE4 to the protective APOE2 allele in adult mice [39].
Experimental Workflow:
- Model Generation: APOE4s2 mice express a floxed coding region of human APOE4 followed by exon 4 of human APOE2. These mice are crossed with a ROSA26-CreERT1 strain for tamoxifen-activated, global Cre recombination.
- Induction of Switch: Administration of tamoxifen to adult APOE4s2G mice induces excision of the APOE4 exon, leading to exclusive expression of APOE2.
- Validation: The switch is confirmed at the mRNA level via qPCR with allelic discrimination and at the protein level via targeted mass spectrometry, which showed 84-93% of ApoE peptides in the brain were unique to E2 post-switch.
- Phenotypic Assessment: Mice are assessed for changes in cerebral transcriptome (single-cell RNAseq), lipidome (LC-MS/MS), amyloid pathology, gliosis, and cognition (e.g., in cross with 5xFAD AD model) [39].
Key Findings: A whole-body or astrocyte-specific switch from E4 to E2 in adult 5xFAD mice decreased amyloid pathology, reduced gliosis, lowered plaque-associated ApoE, and improved cognitive function. This demonstrates that the detrimental effects of APOE4 are reversible in adulthood and targeting APOE is a viable therapeutic strategy [39].
The following diagram illustrates the logic and workflow of the APOE switch experiment:
Single-Nucleus RNA Sequencing to Profile Microglial Responses
To investigate how human microglia respond to pathology based on genotype, researchers employ single-nucleus RNA sequencing (snRNA-seq) on post-mortem brain tissue [40].
- Protocol Summary:
- Sample Preparation: Frozen frontal cortex tissue is homogenized, and nuclei are isolated via ultracentrifugation through a sucrose cushion.
- Library Preparation & Sequencing: Isolated nuclei are processed using the 10x Genomics Chromium system for droplet-based snRNA-seq, followed by sequencing on an Illumina HiSeq 2500.
- Bioinformatic Analysis: Raw sequencing data is aligned (CellRanger) and a pre-mRNA reference is used to capture intronic reads. Data is normalized (SCANPY), highly variable genes are selected, and nuclei are clustered using the DESC algorithm to effectively remove batch effects.
- Differential Expression & Population Analysis: Clusters are annotated to cell types (e.g., microglia, astrocytes), and differential expression analysis is performed to identify genotype-specific changes. The abundance of specific microglial subpopulations (like ARM) is quantified across genotypes [40].
Visualizing Key Signaling Pathways
The core pathway linking genetic risk to impaired clearance involves a critical APOE-TREM2 interaction on microglia. The following diagram synthesizes this mechanism from the cited literature [38] [41] [42].
The Scientist's Toolkit: Key Research Reagents and Models
The following table details essential materials and models used in the experiments cited within this review, providing a resource for researchers seeking to replicate or build upon these findings.
Table 3: Research Reagent Solutions for Investigating Genetic Clearance Mechanisms
| Reagent / Model | Specific Example | Primary Research Application |
|---|---|---|
| Inducible Genetic Mouse Models | APOE4s2 (APOE switch) [39] | To study the temporal and cell-type-specific effects of switching risk alleles to protective ones in adulthood. |
| Humanized Mouse Models | APOE2, E3, E4 Targeted Replacement (TR) mice [39] | To investigate isoform-specific effectsof human APOE on pathology and clearance in a controlled in vivo setting. |
| Single-Cell/Nucleus RNA-Seq | 10x Genomics Chromium System [40] | To unbiasedly profile cell-type-specific transcriptomic responses to pathology across different genotypes in human or mouse brain. |
| Cell Surface Markers for Imaging | Anti-CD163 (for ARM) [40], Anti-GFAP (astrocytes), Anti-IBA1 (microglia) [39] | To identify and quantify specific cell populations and their activation states via immunohistochemistry or flow cytometry. |
| Mass Spectrometry | Targeted LC-MS/MS for ApoE peptides [39], Untargeted LC-MS/MS for lipidomics [39] | To precisely quantify protein isoforms and conduct comprehensive lipidomic profiling of brain and plasma samples. |
The genetic architecture of Alzheimer's disease, with APOE and TREM2 as central pillars, exerts a profound influence on the brain's capacity to clear protein aggregates. The evidence is clear that risk variants converge on microglial dysfunction, impairing the detection, response, and phagocytic elimination of Aβ and pathological tau. The demonstrated reversibility of APOE4-related deficits in adult mouse models offers a powerful and promising therapeutic outlook.
Future research must focus on translating this genetic knowledge into precision medicine. This includes developing gene-editing approaches (e.g., in vivo conversion of APOE4 to APOE2), TREM2-agonistic antibodies (e.g., AL002), and small molecules that can modulate these pathways to restore resilient clearance function. Furthermore, integrating genetic profiling into clinical trial design will be essential for identifying patient subgroups most likely to benefit from targeted clearance-enhancing therapies.
Advanced Technologies: Proteomics, Imaging, and Biomarker Development for Clearance Pathway Analysis
Alzheimer's disease (AD) is a progressive neurodegenerative disorder characterized by the accumulation of protein aggregates, primarily amyloid-beta (Aβ) plaques and tau neurofibrillary tangles [45] [46]. The clearance of these aggregates represents a crucial area of therapeutic investigation. Mass spectrometry (MS)-based proteomics has emerged as a powerful tool for mapping the complex protein pathways underlying AD pathogenesis, offering unprecedented insights into disease mechanisms beyond canonical amyloid and tau pathology [45] [47]. Advanced proteomic technologies now enable researchers to profile thousands of proteins simultaneously in brain tissues and biofluids, revealing novel components in broad protein networks involving RNA splicing, immune response, synaptic function, and mitochondrial activity [48]. This technical guide examines three cornerstone MS techniques—tandem mass tag (TMT) labeling, data-independent acquisition (DIA), and parallel reaction monitoring (PRM)—and their application for mapping protein aggregation clearance pathways in AD research.
Core Mass Spectrometry Technologies
Tandem Mass Tag (TMT) Proteomics
TMT employs isobaric chemical labels to enable multiplexed protein quantification across multiple samples in a single MS run [45]. The typical TMT workflow involves:
- Sample Preparation: Protein extracts from AD and control brains are digested with trypsin to generate peptides.
- Labeling: Peptides from different samples are labeled with TMT reagents that have identical mass but yield unique reporter ions upon fragmentation.
- Pooling and Fractionation: Labeled samples are combined and often fractionated using two-dimensional liquid chromatography to reduce complexity.
- LC-MS/MS Analysis: Fractions are analyzed by liquid chromatography coupled to tandem mass spectrometry.
- Data Analysis: Quantification is achieved by measuring the relative intensities of reporter ions in MS2 or MS3 scans [45].
Key Applications in AD Research: TMT enables comprehensive proteome profiling across brain regions from AD patients at different Braak stages, revealing consensus protein alterations [45]. This approach has identified novel disease-associated proteins including MDK, PTN, NTN1, and SMOC1, which have been validated in functional studies [45]. One significant study quantified 6,533 proteins from the dorsolateral prefrontal cortex across AD, asymptomatic AD (AsymAD), and controls, revealing alterations in proteins involved in mRNA splicing that correlated with AD pathology and cognitive decline [46].
Table 1: Technical Specifications of TMT Proteomics
| Parameter | Specification | Application in AD Research |
|---|---|---|
| Multiplexing Capacity | Up to 16 samples (with TMTpro) | Longitudinal studies of AD progression |
| Protein Coverage | >10,000 proteins with fractionation | Comprehensive mapping of AD proteome |
| Sample Requirement | As low as 1μg protein | Precious brain tissue samples |
| Quantification Precision | Moderate (ratio compression effects) | Identifying moderate effect size changes |
| Key Advantage | Reduced missing data | Consistent protein detection across cohorts |
Data-Independent Acquisition (DIA)
DIA operates by systematically fragmenting all ions within predetermined m/z windows throughout the LC separation, creating comprehensive digital proteome maps [49]. The DIA workflow consists of:
- Library Generation: A spectral library is created from data-dependent acquisition (DDA) or synthesized from sequence databases.
- DIA Acquisition: Instead of isolating individual precursors, the mass spectrometer cycles through sequential isolation windows (typically 20-40) covering the entire m/z range.
- Data Extraction: Computational tools extract fragment ion chromatograms for each peptide using the spectral library.
- Quantification: Peak areas are integrated for quantification across samples [49].
Key Applications in AD Research: DIA has been applied to profile postmortem brain tissues from well-characterized cohorts including autosomal dominant AD, sporadic AD, and controls free of significant comorbidities [49]. This approach provides consistent sampling and quantification at the peptide level, which is crucial for detecting specific proteoforms such as truncated Aβ peptides or phosphorylated tau species [49]. Recent advancements with Astral mass analyzers have increased proteome coverage to nearly 10,000 proteins with less than 1μg protein input, enabling deep profiling of limited AD brain samples [45].
Table 2: Technical Specifications of DIA Proteomics
| Parameter | Specification | Application in AD Research |
|---|---|---|
| Data Completeness | High (minimal missing values) | Longitudinal and cross-regional brain studies |
| Reproducibility | Excellent (systematic sampling) | Multi-cohort biomarker verification |
| Dynamic Range | ~5 orders of magnitude | Detection of low-abundance regulatory proteins |
| Throughput | Moderate to high | Large cohort screening for biomarker discovery |
| Key Advantage | Archive of all detectable species | Retrospective analysis of new hypotheses |
Parallel Reaction Monitoring (PRM)
PRM is a targeted proteomics method that provides highly specific and sensitive quantification of predetermined proteins of interest [45]. The PRM workflow includes:
- Assay Development: Proteotypic peptides representing target proteins are selected based on prior discovery data.
- Method Optimization: Retention times and fragmentation patterns are established using synthetic standards.
- Targeted Acquisition: The mass spectrometer monitors specific precursor ions and records all fragment ions in a high-resolution orbitrap.
- Data Analysis: Fragment ion chromatograms are extracted for quantification, with matching to reference spectra for verification [45].
Key Applications in AD Research: PRM serves as the gold standard for validating candidate biomarkers from discovery studies [50]. In one recent multicenter study, PRM was used to validate 58 CSF and 12 serum proteins as early diagnostic biomarkers for AD, leading to the development of a 19-protein CSF panel that accurately classified mild cognitive impairment due to AD from normal cognition with an area under the curve of 0.984 [50]. PRM enables precise measurement of specific proteoforms, such as hyperphosphorylated tau species, without the need for specific antibodies [45].
Table 3: Technical Specifications of PRM Proteomics
| Parameter | Specification | Application in AD Research |
|---|---|---|
| Sensitivity | Attomole to femtomole range | Quantifying low-abundance biomarkers in biofluids |
| Specificity | High (MS/MS fragmentation patterns) | Distinguishing between protein isoforms |
| Precision | Excellent (CVs typically <15%) | Longitudinal monitoring of disease progression |
| Multiplexing | Tens to hundreds of targets | Validating biomarker panels |
| Key Advantage | Antibody-free quantification | Novel protein targets without available immunoassays |
Integrated Workflow for AD Pathway Mapping
Figure 1: Integrated MS Workflow for AD Pathway Mapping
A synergistic approach combining TMT, DIA, and PRM provides a powerful framework for comprehensively mapping protein aggregation clearance pathways in AD [45]. The typical integrated workflow begins with TMA-based discovery proteomics to identify potential protein alterations across multiple AD brain regions and biofluid samples. Candidates from this initial phase are subsequently verified using DIA, which provides more reproducible quantification across larger sample sets. Finally, the most promising targets undergo rigorous validation using PRM for ultimate confirmation [50]. This tiered approach balances discovery power with quantitative rigor, efficiently allocating resources while maximizing the robustness of findings. The integration of proteomic data with genetic information through protein quantitative trait locus (pQTL) analysis further strengthens the biological relevance of identified pathways [45].
Experimental Protocols for AD Proteomics
Protocol 1: TMT-based Brain Proteome Profiling
Sample Requirements: Postmortem brain tissue (prefrontal cortex, hippocampus) from AD and control cases, typically 10-20mg per sample [46].
Step-by-Step Procedure:
- Tissue Homogenization: Homogenize brain tissue in urea lysis buffer (8M urea, 100mM Tris pH 8.0) with protease and phosphatase inhibitors.
- Protein Digestion: Reduce with dithiothreitol (5mM, 30min), alkylate with iodoacetamide (15mM, 30min in dark), and digest with Lys-C (1:100, 3h) followed by trypsin (1:50, overnight) after 4-fold dilution.
- Peptide Labeling: Label 100μg peptides from each sample with TMT reagents (resuspended in anhydrous acetonitrile) for 1h at room temperature.
- Pooling and Quenching: Combine labeled samples and quench with hydroxylamine to 0.4% final concentration.
- High-pH Fractionation: Separate pooled peptides using high-pH reverse-phase chromatography into 96 fractions consolidated into 24-48 samples.
- LC-MS/MS Analysis: Analyze fractions on a nano-LC system coupled to an Orbitrap mass spectrometer with MS3-based quantification method [45] [46].
Quality Control Measures:
- Include quality control pools in each TMT set
- Monitor labeling efficiency (>98%) by analyzing small aliquot pre- and post-labeling
- Assess fractionation quality by base peak chromatograms
Protocol 2: DIA for Aggregated Proteome Analysis
Sample Requirements: Detergent-insoluble protein fractions from AD brain tissues or laser-capture microdissected plaques/tangles [51].
Step-by-Step Procedure:
- Aggregate Enrichment: Extract detergent-insoluble proteins using sarkosyl fractionation - homogenize tissue in 10 volumes of buffer (1% sarkosyl, 50mM Tris pH 7.5), centrifuge at 100,000g for 30min, collect pellet.
- Protein Digestion: Solubilize pellet in 8M urea, 100mM Tris pH 8.0, and digest as described in Protocol 1.
- Spectral Library Generation: Create project-specific library by data-dependent acquisition or use available brain proteome libraries.
- DIA Acquisition: Program mass spectrometer to acquire MS1 scans (120,000 resolution) followed by 30-40 DIA windows (variable width) covering 400-1000m/z.
- Data Processing: Use specialized software (DIA-NN, Spectronaut) to extract peptide quantities with project-specific library [49] [51].
Quality Control Measures:
- Monitor retention time stability across runs (<0.5min drift)
- Include quality control samples every 10-12 injections
- Assess quantitative precision with coefficient of variation <20% for high-abundance proteins
Protocol 3: PRM for Biomarker Validation
Sample Requirements: Cerebrospinal fluid (CSF) or plasma/serum from well-characterized AD cohorts and controls [50].
Step-by-Step Procedure:
- Peptide Selection: Choose 2-3 proteotypic peptides per target protein, avoiding polymorphisms and modifications.
- Synthetic Standards: Obtain heavy isotope-labeled versions of target peptides as internal standards.
- Sample Preparation: Deplete high-abundance proteins from biofluids if necessary, then reduce, alkylate, and digest as in Protocol 1.
- Spike-in Standards: Add heavy labeled synthetic peptides to each sample before LC-MS analysis.
- PRM Acquisition: Program instrument to target specific precursors with 1-2Th isolation width, high-resolution MS2 (35,000-70,000) in orbitrap.
- Data Analysis: Extract fragment ion chromatograms for light and heavy peptides, calculate light-to-heavy ratios for quantification [45] [50].
Quality Control Measures:
- Monitor retention time alignment with synthetic standards (<1min deviation)
- Ensure fragment ion ratios match reference spectra (<20% deviation)
- Maintain signal-to-noise ratio >10 for quantification
Pathway Mapping in Alzheimer's Disease
Protein Aggregation Clearance Pathways
Figure 2: Key AD Pathways Identified by Proteomics
Proteomic studies have revealed intricate networks of protein aggregation clearance pathways in AD that extend far beyond the canonical amyloid and tau pathways [47]. The ubiquitin-proteasome system (UPS) and autophagy-lysosomal pathway emerge as central clearance mechanisms, with multiple components showing altered expression in AD brain [48]. Specifically, proteomic analysis of detergent-insoluble protein aggregates from AD brain tissue has identified numerous proteins involved in proteostasis, including ubiquitin ligases and autophagy receptors [51]. Interestingly, the U1 small nuclear ribonucleoprotein (U1 snRNP) complex, a key component of the RNA splicing machinery, was identified as a major constituent of protein aggregates in AD, suggesting a novel link between RNA processing defects and protein aggregation [51]. These findings underscore the complexity of proteostasis disruption in AD and highlight potential therapeutic targets for enhancing aggregate clearance.
Multi-Omics Integration for Pathway Validation
Integrating proteomic data with genetic and transcriptomic information provides a powerful approach for validating the biological relevance of identified pathways [45]. Protein quantitative trait locus (pQTL) analysis links genetic risk variants to protein expression changes, helping prioritize causal proteins in AD pathogenesis [45]. For example, proteogenomic integration has revealed discrepancies between transcriptomic and proteomic changes in AD brain, suggesting altered protein turnover contributes to disease progression [45]. This multi-omics approach has helped validate the involvement of diverse cellular processes in AD, including RNA splicing, immune response, mitochondrial function, and synaptic transmission [48]. The integration of proteomic data from brain tissue with biofluid proteomes further enables the translation of pathway insights into accessible biomarkers for clinical applications [50].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for AD Proteomics
| Reagent Category | Specific Products | Function in AD Proteomics |
|---|---|---|
| Protein Extraction | Sarkosyl, Urea, RIPA Buffer | Solubilization of aggregate-prone proteins from AD brain tissue |
| Digestion Enzymes | Trypsin, Lys-C | Protein digestion to peptides for MS analysis |
| Labeling Reagents | TMTpro 16-plex, TMT 11-plex | Multiplexed quantification of samples from different AD stages |
| Chromatography | C18 columns, High-pH fractionation | Peptide separation pre-MS analysis |
| Internal Standards | Heavy labeled synthetic peptides | Absolute quantification in PRM assays |
| Affinity Reagents | Olink, SomaScan | Validation of MS findings in large cohorts |
The integration of TMT, DIA, and PRM mass spectrometry approaches provides a powerful technological framework for mapping protein aggregation clearance pathways in Alzheimer's disease research. TMA-based discovery proteomics enables comprehensive profiling of AD brain proteomes, revealing novel disease-associated proteins and pathways. DIA offers robust digital mapping for verification across larger cohorts, while PRM delivers precise targeted quantification for biomarker validation. Together, these technologies are advancing our understanding of the complex molecular networks underlying AD pathogenesis and accelerating the development of biomarkers for early diagnosis and therapeutic monitoring. As these technologies continue to evolve with improvements in sensitivity, throughput, and computational analysis, they promise to unlock further insights into protein homeostasis disruption in AD and related neurodegenerative disorders.
The pursuit of biomarkers for Alzheimer's disease (AD) and other neurodegenerative conditions has entered a transformative phase with the advent of high-throughput proteomic technologies. Affinity-based proteomic platforms represent a powerful approach for large-scale protein quantification in biological fluids, enabling researchers to discover novel biomarkers and elucidate complex disease mechanisms. These technologies are particularly valuable for studying protein aggregation clearance pathways in AD, as they can simultaneously measure hundreds to thousands of proteins across numerous samples with exceptional sensitivity. The emergence of these platforms addresses a critical need in neurodegenerative disease research, where understanding the interplay between pathological protein aggregation and cellular clearance mechanisms is paramount for therapeutic development [52] [53].
Among the various affinity-based solutions, Olink and SomaScan have emerged as leading platforms, each employing distinct biochemical principles to achieve comprehensive proteomic coverage. Olink utilizes a Proximity Extension Assay (PEA) technology that combines antibody-based protein detection with DNA amplification for highly specific quantification. SomaScan employs single-stranded DNA aptamers (SOMAmers) that undergo conformational changes upon protein binding, enabling precise protein measurement. Both platforms overcome traditional limitations in proteomic research by providing high multiplexing capabilities, excellent sensitivity, and high sample throughput - essential characteristics for large-scale biomarker discovery initiatives in complex disorders like Alzheimer's disease [54] [55].
The integration of these technologies into AD research has revealed profound insights into the molecular underpinnings of disease pathology. Recent studies have demonstrated that beyond the canonical amyloid-beta (Aβ) and tau pathology, numerous other proteomic alterations occur in AD, including dysregulation of proteins involved in synaptic function, inflammation, microglial reactivity, and cellular clearance pathways. Affinity-based platforms have been instrumental in identifying these changes, providing a more comprehensive understanding of AD pathophysiology and opening new avenues for therapeutic intervention [56] [52].
Olink's Proximity Extension Assay (PEA) Technology
Olink's PEA technology represents a sophisticated approach to high-plex protein detection that combines the specificity of immunoassays with the amplification power of DNA sequencing. The core mechanism relies on matched antibody pairs labeled with complementary DNA oligonucleotides. When both antibodies bind to their target protein epitopes, the DNA tags come into close proximity, enabling hybridization and extension by a DNA polymerase. This creates a double-stranded DNA barcode that uniquely identifies the target protein and is quantified using next-generation sequencing or microfluidic real-time PCR [57] [58].
The PEA technology offers several distinctive advantages for neurodegenerative disease research. The requirement for dual antibody binding significantly enhances specificity and reduces cross-reactivity compared to single-antibody assays. Additionally, the DNA-based readout is highly sensitive, capable of detecting proteins in the low picogram per milliliter range, which is crucial for measuring low-abundance biomarkers in blood-based AD diagnostics. The platform requires minimal sample volume (typically 1-6 μL per panel), making it particularly valuable for studies with limited biospecimen availability, such as cerebrospinal fluid (CSF) analyses from patients with neurodegenerative conditions [54] [57].
Olink provides several product lines with varying degrees of multiplexing capacity. The Explore platform offers the highest plex, capable of measuring up to 5,400 proteins from a single sample aliquot. The Target series provides focused panels (e.g., 96-plex) for specific research areas, including inflammation, neurology, and oncology. The Focus series offers smaller custom panels designed for clinical validation studies. This flexibility allows researchers to tailor their proteomic profiling strategy to specific experimental needs throughout the biomarker development pipeline [57].
SomaScan's Aptamer-Based Proteomics
SomaScan employs a different affinity reagent class based on single-stranded DNA aptamers called SOMAmers (Slow Off-rate Modified Aptamers). These engineered molecules incorporate modified nucleotides with protein-like side chains that enhance structural diversity and binding affinity to protein targets. Each SomaScan assay uses a single SOMAmer that undergoes a conformational change upon target protein binding, which forms the basis for protein quantification through a specialized capture and detection process [55] [59].
The SomaScan workflow involves incubating the biological sample with the SOMAmer library, followed by partitioning of bound and unbound SOMAmers through a series of steps that ultimately result in the quantification of protein-bound SOMAmers. The platform's key innovation lies in the nucleotide modifications that significantly expand the chemical diversity beyond natural nucleic acids, enabling high-affinity binding to a wide range of protein targets. This approach allows SomaScan to achieve exceptional proteomic coverage, with current versions measuring up to 11,000 proteins from approximately 50-65 μL of sample [55] [59].
A notable characteristic of SomaScan is its broad dynamic range, which spans up to 10 orders of magnitude, enabling simultaneous quantification of high-abundance and low-abundance proteins without sample pre-fractionation. This is particularly advantageous for comprehensive biomarker discovery in neurodegenerative diseases, where relevant protein signals may occur across extreme concentration ranges in biofluids. The platform's reproducibility and relatively low coefficient of variation (median ~10% based on replicate measurements) further support its utility in large-scale longitudinal studies of disease progression [55].
Table 1: Technical Comparison of Olink and SomaScan Platforms
| Parameter | Olink | SomaScan |
|---|---|---|
| Technology Basis | Proximity Extension Assay (PEA) with paired antibodies | Modified aptamers (SOMAmers) with protein-like side chains |
| Multiplexing Capacity | Up to 5,400 proteins | Up to 11,000 proteins |
| Sample Volume | 1-6 μL (varies by panel) | ~50-65 μL |
| Detection Principle | DNA barcode creation + qPCR/NGS | SOMAmer conformational change + quantification |
| Dynamic Range | ~10 logs | ~10 logs |
| Median CV | ~16.5% (Explore 3072) | ~9.9% (v4) |
| Throughput | High (96-384 samples per run) | High (96-384 samples per run) |
| Measurement Type | Relative quantification (NPX) | Relative quantification (RFU) |
Application in Alzheimer's Disease and Protein Aggregation Research
Insights into AD Pathobiology and Biomarker Discovery
Affinity-based proteomic platforms have dramatically advanced our understanding of Alzheimer's disease beyond the traditional amyloid and tau-centric models. Large-scale studies using these technologies have revealed consistent proteomic alterations in AD brain tissues, biofluids, and animal models, providing unprecedented insights into disease mechanisms. Multi-cohort analyses have identified consensus protein changes (n=866) in AD brains, with many of these proteins functionally validated in subsequent studies. Notable findings include dysregulation of proteins involved in diverse biological processes, including MDK/PTN, NTN1, SMOC1, GPNMB, NPTX2, NRN1, VGF, and U1 snRNP, many of which represent potential therapeutic targets or biomarker candidates [52].
The application of Olink and SomaScan in biofluid profiling has been particularly transformative for AD biomarker development. Studies comparing CSF and plasma proteomes from the same individuals have revealed that many proteins altered in AD CSF show opposite directional changes in plasma, with the notable exception of SMOC1, a matrisome-associated protein that is elevated in both biofluids and linked to amyloid-β deposition. Protein co-expression analyses of large proteomic datasets have identified significantly altered modules related to autophagy, ubiquitination, sugar metabolism in CSF, and endocytosis and matrisome pathways in plasma, highlighting the potential of these platforms to uncover systemic biological processes relevant to AD pathogenesis [58].
These technologies have also enabled the identification of distinct molecular subtypes of AD based on proteomic signatures, moving the field toward precision medicine approaches. For instance, a study leveraging Olink technology identified a protein risk score for dementia in individuals with major depressive disorder, highlighting specific proteins (NfL, GFAP, PSG1, VGF, GET3, and HPGDS) associated with increased AD risk in this vulnerable population. Such findings demonstrate how affinity proteomics can stratify patient populations and identify context-specific biomarker signatures, ultimately supporting more targeted therapeutic development [57].
Studying Protein Aggregation Clearance Pathways
The integration of Olink and SomaScan platforms into research on protein quality control mechanisms has provided critical insights into the dysfunction of aggregation clearance pathways in Alzheimer's disease. These technologies enable comprehensive profiling of proteins involved in key clearance mechanisms, including the ubiquitin-proteasome system (UPS), autophagy-lysosomal pathway (ALP), chaperone-mediated autophagy (CMA), and the unfolded protein response (UPR) [53].
Research using these platforms has revealed significant alterations in multiple components of cellular protein quality control systems in AD. For example, studies have identified dysregulation of molecular chaperones (e.g., HSP70 family members), ubiquitin ligases, and autophagy-related proteins in AD biofluids and tissues. These findings align with the growing recognition that impaired clearance of misfolded proteins, rather than solely their overproduction, contributes significantly to AD pathogenesis. The ability to simultaneously measure numerous components of these complex pathways provides a systems-level view of how protein homeostasis becomes disrupted in neurodegenerative conditions [52] [53].
Affinity proteomics has also shed light on the interplay between different pathological proteins in AD. Beyond Aβ and tau, these platforms have detected alterations in α-synuclein and TDP-43 related pathways in AD biofluids, suggesting convergent mechanisms of proteostasis failure across different proteinopathies. This has important implications for understanding the mixed pathologies commonly observed in AD patients and for developing therapeutic strategies that target shared clearance mechanisms rather than individual aggregated proteins [56] [60].
Table 2: Key Protein Clearance Pathways Studied Using Affinity Proteomics in AD
| Clearance Pathway | Key Components Identified | Relevance to AD |
|---|---|---|
| Ubiquitin-Proteasome System (UPS) | Ubiquitin ligases, proteasome subunits | Impaired degradation of misfolded proteins, tau clearance |
| Autophagy-Lysosomal Pathway (ALP) | LC3, p62, LAMP proteins, cathepsins | Defective clearance of protein aggregates, organelle quality control |
| Chaperone-Mediated Autophagy (CMA) | HSC70, LAMP2A | Impaired targeting of specific substrates including tau |
| Unfolded Protein Response (UPR) | PERK, IRE1, ATF6 signaling components | ER stress response to protein misfolding |
| Microglial Phagocytosis | TREM2, complement proteins | Clearance of extracellular protein aggregates |
Experimental Design and Methodologies
Standardized Protocols for Neurodegenerative Disease Studies
Implementing robust experimental protocols is essential for generating reliable data from affinity-based proteomic platforms, particularly when studying complex neurodegenerative diseases like Alzheimer's. Well-designed studies incorporate careful consideration of cohort selection, sample processing, quality control measures, and data normalization strategies to minimize technical variability and enhance biological discovery.
For AD biomarker studies, participant characterization should include comprehensive clinical assessment, cognitive testing, and ideally, neuroimaging or established fluid biomarkers (e.g., CSF Aβ42/40, p-tau) to define pathological endophenotypes. As demonstrated in recent studies, this enables stratification based on underlying pathology rather than clinical symptoms alone, increasing the likelihood of identifying specific biomarker signatures. Sample collection protocols must be standardized, with attention to variables such as fasting status, time of day, sample processing delays, and storage conditions, all of which can influence protein measurements. For plasma and serum studies, the choice of anticoagulant (EDTA, heparin, or citrate) can also impact protein quantification and should be consistent within a study [56] [61].
The analytical process begins with sample thawing and dilution according to platform-specific requirements. For Olink, samples are typically diluted and mixed with the incubation solution containing antibody pairs. For SomaScan, samples are diluted and incubated with the SOMAmer reagent mixture. Both platforms incorporate internal controls to monitor technical performance throughout the process. Following the binding reaction, each platform employs distinct detection methods: Olink uses proximity extension and PCR amplification, while SomaScan uses a series of partitioning steps and SOMAmer quantification. The entire workflow for both platforms is automated in 96- or 384-well formats to ensure consistency and enable high throughput [55] [57].
Quality control measures are critical for data integrity. Both platforms include internal controls for normalization, and samples should meet platform-specific QC metrics before inclusion in final analyses. Additional study-specific QC measures may include technical replicates, sample randomization to avoid batch effects, and the inclusion of reference samples for cross-batch normalization in large studies. For neurodegenerative disease research, where effect sizes may be modest, these rigorous QC procedures are essential for distinguishing true biological signals from technical noise [61] [55].
Data Processing and Normalization Approaches
Data processing for affinity-based proteomics involves multiple steps to transform raw signals into normalized protein values suitable for statistical analysis. For Olink data, raw Ct values (for qPCR readout) or sequence counts (for NGS readout) are converted to Normalized Protein eXpression (NPX) values, which are on a log2 scale where a one-unit increase represents a doubling of protein concentration. The normalization procedure accounts for intra- and inter-run variation using internal controls.
SomaScan data processing involves several normalization steps to address technical variability. The first normalization corrects for inter-plate variation using hybridization controls. Subsequent steps include median signal normalization to correct for overall protein content differences between samples, and calibration normalization to standardize signals across runs. A critical consideration for SomaScan data is whether to apply the additional median normalization step (SMP normalization) recommended by the manufacturer, as this can impact inter-platform correlations and biological interpretations [55].
Following platform-specific normalization, additional study-specific normalization may be applied to address batch effects and other technical confounders. Methods such as ComBat, remove unwanted variation (RUV), or variance component analysis can be employed to identify and adjust for technical artifacts. For studies integrating genetic data, protein quantitative trait locus (pQTL) analysis can serve as both a validation of protein measurements and a means to identify genetic influences on protein levels, potentially revealing biological insights into disease mechanisms [55].
Performance Benchmarking and Comparative Analyses
Analytical Performance Metrics
Rigorous benchmarking studies have provided valuable insights into the comparative performance of Olink and SomaScan platforms, highlighting their respective strengths and limitations for neurodegenerative disease research. A large-scale comparison using data from the UK Biobank Pharma Proteomics Project (Olink Explore 3072) and Icelandic population (SomaScan v4) revealed distinct performance characteristics across multiple metrics [55].
Precision analysis based on duplicate measurements shows that SomaScan assays generally exhibit lower median coefficients of variation (CV) compared to Olink (9.9% versus 16.5%, respectively). This pattern persists even when restricting analysis to the 1,823 proteins targeted by both platforms (9.5% for SomaScan versus 14.7% for Olink). The higher precision of SomaScan measurements may be advantageous for detecting subtle protein changes in longitudinal studies or for identifying modest effect sizes in large population studies. However, both platforms demonstrate sufficient precision for most biomarker discovery applications [55].
Correlation between matching assays on the two platforms is generally modest, with a median Spearman correlation of 0.33 across 1,848 protein pairs in a direct comparison study. This correlation improves to 0.39 when SomaScan data are analyzed without the recommended median normalization step. The distribution of correlation coefficients is bimodal, with one mode just above zero and another just below 0.6, suggesting that a subset of proteins shows reasonable concordance between platforms while others do not. These findings highlight that measurements from the two platforms are not directly interchangeable, and platform selection can significantly influence research conclusions [55].
Both platforms show similar patterns related to protein abundance, with the lowest correlation between platforms observed for proteins in the lowest dilution group (i.e., those with lowest expected abundance in plasma). The fraction of values below the limit of detection is higher for Olink assays, particularly for proteins in the undiluted group, and correlates positively with CV (Spearman correlation 0.69). These observations underscore the challenges in quantifying low-abundance proteins, which include many biologically relevant signaling molecules and potential biomarkers for neurological disorders [55].
Biological Validation and Concordance with Other Platforms
The performance of affinity-based platforms is often assessed through biological validation using established protein biomarkers and comparison with orthogonal technologies. For Alzheimer's disease biomarkers, both Olink and SomaScan show good concordance with established immunoassays and mass spectrometry methods for key analytes, though with some important variations.
Studies benchmarking these platforms for AD-relevant biomarkers have found that CSF measures of Aβ42/40, NfL, GFAP, and p-tau217 are highly correlated between affinity platforms and established methods, with similar predictive performance for amyloid pathology. In plasma, p-tau217 shows similar performance across technologies for predicting amyloidosis, supporting its utility as a core AD biomarker. However, other established and exploratory biomarkers (total tau, p-tau181, NRGN, YKL40, sTREM2, VILIP1) show a wide range of correlation values depending on the biofluid and comparison platform [61].
The presence of protein quantitative trait loci (pQTLs) provides genetic evidence supporting assay performance. Both platforms detect a similar absolute number of cis pQTLs (approximately 2,100), but the proportion of assays with such genetic support is higher for Olink (72% versus 43% for SomaScan). This difference may reflect the dual antibody requirement of Olink assays, which potentially increases specificity, though both platforms demonstrate robust genetic validation for a substantial portion of their assays [55].
Multi-platform proteomic studies of AD biofluids have further informed our understanding of platform concordance. One study comparing SomaScan, Olink, and tandem mass tag-based mass spectrometry in paired CSF and plasma samples found median correlations of overlapping protein measurements of approximately r=0.7 in CSF and r=0.6 in plasma, with greater variability observed in plasma. Interestingly, SomaScan provided the most protein measurements in plasma, highlighting its extensive coverage, while all platforms generated complementary data contributing to a more comprehensive understanding of the AD proteomic landscape [58].
Table 3: Performance Comparison in Neurodegenerative Disease Research
| Performance Metric | Olink | SomaScan | Implications for AD Research |
|---|---|---|---|
| Correlation with MS/Immunoassays | Variable by analyte; strong for key AD biomarkers (p-tau217, GFAP, NfL) | Variable by analyte; generally good for abundant proteins | Key AD biomarkers reliably measured by both platforms |
| cis-pQTL Support | 72% of assays | 43% of assays | Higher genetic validation for Olink assays |
| Sample Throughput | High (96-384 samples/run) | High (96-384 samples/run) | Suitable for large cohort studies |
| Low-Abundance Protein Detection | Challenging for some low-abundance targets | Broader dynamic range | Differential coverage of signaling pathways |
| Cross-Platform Correlation | Median r=0.33 with SomaScan | Median r=0.33 with Olink | Measurements not directly interchangeable |
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing affinity-based proteomic studies requires careful selection of reagents and materials to ensure experimental success. The following table outlines key components of the research toolkit for studies utilizing Olink and SomaScan platforms in neurodegenerative disease research.
Table 4: Essential Research Reagents and Materials for Affinity Proteomics
| Category | Specific Reagents/Materials | Function and Importance |
|---|---|---|
| Biological Samples | Plasma, serum, CSF, brain tissue homogenates | Source of protein biomarkers; sample type and processing critical for data quality |
| Sample Collection Supplies | EDTA/K2EDTA blood collection tubes, CSF collection kits, protease inhibitors | Standardized collection to preserve protein integrity and minimize pre-analytical variability |
| Platform-Specific Kits | Olink Panels (Explore, Target, Focus), SomaScan Kits | Core reagent sets containing affinity reagents, buffers, and controls for protein quantification |
| Quality Control Materials | Platform controls, pooled reference samples, internal standards | Monitor technical performance and enable cross-batch normalization |
| Laboratory Equipment | Thermal cyclers, plate washers, liquid handlers, sequencers (for Olink NGS) | Essential instrumentation for executing platform workflows |
| Data Analysis Tools | Platform-specific software, statistical packages (R, Python), bioinformatics resources | Data processing, normalization, and biological interpretation |
| Validation Reagents | Western blot antibodies, ELISA kits, IP-MS reagents | Orthogonal validation of key findings using alternative methods |
Signaling Pathways in Protein Aggregation and Clearance
The application of affinity proteomics in Alzheimer's disease research has elucidated numerous molecular pathways implicated in protein aggregation and clearance mechanisms. The following diagram illustrates key pathways that can be effectively studied using Olink and SomaScan platforms, highlighting potential therapeutic targets for enhancing clearance of pathological protein aggregates.
Affinity-based proteomic platforms have fundamentally transformed biomarker discovery and pathway analysis in Alzheimer's disease research. Olink and SomaScan technologies provide powerful tools for comprehensively profiling the proteomic alterations associated with protein aggregation and clearance dysfunction in neurodegenerative conditions. While each platform has distinct technical characteristics and performance metrics, both have demonstrated substantial utility in elucidating the complex molecular landscape of AD.
The future of these technologies in neurodegenerative disease research will likely involve increased integration with other omics technologies, including genomics, transcriptomics, and metabolomics. Such multi-omic approaches promise to provide more comprehensive insights into disease mechanisms and identify novel therapeutic targets. Additionally, the application of single-cell and spatial proteomics methods to human brain tissue may reveal cellular heterogeneity in proteostatic responses and identify cell-type-specific vulnerabilities in AD [52].
As these technologies continue to evolve, their implementation in large-scale longitudinal studies and clinical trials will be crucial for validating candidate biomarkers and understanding dynamic protein changes throughout disease progression. The ability to simultaneously measure established AD biomarkers alongside novel protein signatures positions affinity proteomics as a key technology for advancing personalized medicine approaches in neurodegenerative diseases, ultimately contributing to earlier diagnosis, better patient stratification, and more effective therapeutic interventions [56] [57].
The pathological aggregation of proteins such as amyloid-β (Aβ) and tau is a defining feature of Alzheimer's disease (AD), and the efficiency of biological clearance mechanisms is now recognized as a critical determinant in the kinetics of this process [62]. Mathematical models of in vivo aggregation indicate that a critical clearance threshold exists; surpassing this threshold prevents aggregate accumulation, while subtle reductions in clearance efficiency can trigger a dramatic switch from a healthy to a disease state [62]. This framework creates an urgent need for imaging technologies capable of monitoring early protein aggregation and the efficacy of clearance-promoting therapies.
Saturation Transfer Magnetic Resonance Imaging (ST-MRI) emerges as a powerful, non-invasive tool to meet this need. Unlike conventional MRI, ST-MRI is sensitive to the molecular configuration and size of mobile proteins, providing a window into the very early stages of protein aggregation before the formation of solid, insoluble plaques [63] [64]. By detecting changes in the brain's proteomic environment linked to the formation of oligomers and larger aggregates, ST-MRI offers a potential molecular biomarker for assessing the balance between aggregate formation and clearance, thereby providing a unique tool for early diagnosis and therapeutic monitoring in Alzheimer's disease research and drug development [63].
Theoretical Foundations of Saturation Transfer MRI
ST-MRI encompasses techniques that generate image contrast by magnetically labeling specific pools of protons and observing the transfer of this saturation to the bulk water signal. The two primary modalities are Chemical Exchange Saturation Transfer (CEST) and Magnetization Transfer Contrast (MTC).
The CEST Mechanism
CEST detects soluble proteins and metabolites through the exchange of protons between their labile groups (e.g., amide protons) and bulk water [65]. The process can be broken down as follows:
- Saturation: A prolonged, low-power radiofrequency (RF) pulse is applied at the specific resonance frequency of exchangeable protons on a mobile protein, such as the amide protons found in the protein backbone (at +3.6 ppm from water) [63].
- Chemical Exchange: These saturated protons naturally exchange with the abundant, unsaturated protons of bulk water.
- Signal Amplification: The continuous exchange process leads to an accumulation of saturated protons in the water pool, resulting in a measurable decrease (or contrast) in the water signal. This provides an amplification mechanism, allowing the detection of low-concentration compounds [65].
The CEST effect is typically analyzed via the Z-spectrum, a plot of water signal intensity as a function of the saturation pulse frequency offset [63]. Contributions from mobile proteins are often found at specific offsets, notably the composite amide proton signal at +3.6 ppm and the aliphatic proton signal (relayed Nuclear Overhauser Effect, rNOE) at -3.6 ppm [63].
Distinguishing CEST from MTC
While CEST originates from mobile proteins and metabolites through chemical exchange, MTC arises from the dipolar cross-relaxation between water protons and protons bound to solid-like macromolecules and semi-solid tissues [63] [64]. MTC typically produces a very broad Z-spectrum and can confound the specific signal from mobile proteins. Advanced ST-MRI sequences are designed to minimize MTC contributions to isolate the specific signals related to protein aggregation [63].
Technical Implementation: UTE-CEST for Aggregation Monitoring
A key challenge in applying CEST to in vivo protein aggregation is achieving high-quality imaging in the complex brain environment. A implemented solution is the Ultrashort Echo Time CEST (UTE-CEST) sequence with a radial acquisition scheme [63].
UTE-CEST Sequence Design
The UTE-CEST sequence combines a train of saturation pulses with a 2D-UTE radial readout [63]. This design offers two critical advantages for brain imaging:
- Minimized Artefacts: Radial acquisition oversamples the center of k-space, making it inherently less sensitive to motion artefacts and susceptibility differences at tissue interfaces, which are common sources of image degradation [63].
- Detection of Short-T2 Components: The ultrashort echo time (TE = 0.3 ms) allows for the detection of signals from a wide range of water components, including those bound to myelin sheets, which would be lost with conventional longer-TE sequences. This results in a higher signal-to-noise ratio and more accurate visualization of pure CEST contrast [63].
Table 1: Key Parameters of the UTE-CEST Sequence for Protein Aggregation Monitoring [63]
| Parameter | Specification | Function/Rationale |
|---|---|---|
| Saturation Pulse | Gaussian, 30 ms duration, 0.9 μT peak B1 | Provides frequency-selective saturation of target protons while minimizing direct water saturation. |
| Readout Pulse | Gaussian, 0.3 ms duration, 7 μT peak B1 (15° flip angle) | Short, low-flip-angle excitation preserves magnetization steady-state. |
| Echo Time (TE) | 0.3 ms | Ultrashort TE minimizes signal loss from tissues with short T2. |
| Repetition Time (TR) | 40 ms | Establishes a steady state for the combined saturation and readout process. |
| k-space Trajectory | 2D Radial | Reduces motion and susceptibility artefacts; enables self-gating. |
The Saturation Transfer Difference (ΔST) Metric
To quantitatively measure changes in mobile protein configuration, a practical metric called the Saturation Transfer Difference (ΔST) is used [63]. This metric is defined by subtracting the Z-spectral signals at the protein frequencies (±3.6 ppm) from a control signal at a frequency where no meaningful CEST effect is expected (e.g., 8 ppm):
ΔST = Z(8 ppm) - Z(±3.6 ppm) [63]
This calculation helps minimize confounding contributions from direct water saturation and the broad MTC background, providing a more specific measure of the signal from mobile proteins [63].
Experimental Validation and Workflow
The UTE-CEST technique and the ΔST metric were systematically validated in phantom studies and a transgenic AD mouse model (APPswe;PS1ΔE9) [63].
- Phantom Studies: Experiments on glutamate solution, protein (egg white), and hair conditioner demonstrated the sequence's capability to distinguish the target mobile protein signal from signals of amine protons, direct water saturation, and MTC, respectively [63].
- Monitoring Aggregation: Studies on cross-linked bovine serum albumin (BSA) solutions confirmed that the ΔST signal could track the protein aggregation process in a controlled setting [63].
- In Vivo Application: High-resolution ΔST images of AD mouse brains showed a significantly reduced ΔST(-3.6) signal compared to age-matched wild-type controls, indicating its sensitivity to the pathological protein aggregation occurring in vivo [63].
The following diagram illustrates the logical pathway connecting the biochemical process of aggregation to the measurable MRI signal.
Research Reagent Solutions and Experimental Materials
The following table details key reagents and materials used in the featured UTE-CEST experiments for monitoring protein aggregation [63].
Table 2: Essential Research Reagents and Materials for ST-MRI Protein Aggregation Studies
| Reagent/Material | Function in the Experimental Context |
|---|---|
| Cross-linked BSA Solutions | Used as a phantom model to validate the ST-MRI signal's sensitivity to protein aggregation in a controlled in vitro environment. |
| Glutamate Solution | Serves as a control phantom to demonstrate the method's ability to minimize contributions from non-protein CEST sources, such as amine protons. |
| Hair Conditioner | Acts as a phantom rich in solid-like macromolecules to test and verify the suppression of the confounding Magnetization Transfer Contrast (MTC) signal. |
| Egg White | A model system for mobile proteins, used to characterize the Z-spectrum signature of proteins before aggregation. |
| APPswe;PS1ΔE9 Mice | A transgenic mouse model of Alzheimer's disease used for in vivo validation, providing a system with progressive protein aggregation pathology. |
Quantitative Findings and Data
The application of UTE-CEST in AD models yields quantifiable data on the saturation transfer signal, which serves as a biomarker for protein aggregation.
Table 3: Key Quantitative Findings from ST-MRI Studies on Protein Aggregation
| Experimental Model | Key Measured Outcome | Interpretation and Significance |
|---|---|---|
| Cross-linked BSA Phantoms | ΔST signal changes during the aggregation process. | The ΔST signal is a valid indicator for monitoring the protein aggregation process in a controlled solution. |
| AD Mouse Brain (in vivo) | Significantly reduced ΔST(-3.6) signal compared to wild-type controls. | Indicates changes in the mobile protein pool consistent with increased aggregation and a broader Z-spectral lineshape in AD brain tissue. |
| Theoretical Aggregation/Clearance Model | A critical clearance value emerges, above which aggregates do not accumulate. | Provides a mathematical framework showing system stability is highly sensitive to clearance efficiency; small changes can trigger disease [62]. |
Integration with Broader Research and Future Outlook
ST-MRI does not exist in isolation but complements a growing toolkit of biomarkers and imaging technologies for neurodegenerative disease. The AT(N) framework (Amyloid, Tau, Neurodegeneration) for Alzheimer's disease classification relies on a multi-parametric approach [64]. While PET imaging with specific tracers for Aβ and tau provides high specificity, it involves radioactive ligands and has limited sensitivity to the earliest, pre-plaque stages of protein aggregation [64]. ST-MRI fills this gap by providing a non-radioactive, sensitive readout of the mobile proteomic environment, including the formation of oligomeric aggregates [63] [64].
The field is moving toward integrated imaging approaches. For example, combined PET-MRI systems allow for simultaneous acquisition of metabolic or protein-specific data (PET) and high-resolution structural/functional data (MRI), including ST-MRI contrasts, providing a more comprehensive picture of the disease process [66]. Furthermore, the recent development of PET tracers for alpha-synuclein, another protein prone to aggregation in Parkinson's disease and other synucleinopathies, highlights the broader push for molecular imaging across neurodegenerative diseases [67] [68]. ST-MRI, with its label-free nature and sensitivity to general protein configuration changes, holds promise as a complementary and screening tool in this evolving landscape.
In conclusion, Saturation Transfer MRI, particularly advanced implementations like UTE-CEST, represents a powerful technical advancement for monitoring in vivo protein aggregation. By providing a sensitive, non-invasive measure of the early molecular changes linked to impaired clearance pathways in Alzheimer's disease, it offers researchers and drug developers a critical tool for early diagnosis and for assessing the efficacy of novel therapeutics aimed at restoring proteostatic balance.
The accumulation of toxic protein aggregates—amyloid-β (Aβ) plaques and hyperphosphorylated tau tangles—represents the pathological hallmark of Alzheimer's disease (AD) [15] [69]. Emerging evidence suggests that impaired clearance of these aggregates, rather than solely their overproduction, plays a crucial role in AD pathogenesis [15]. Historically, bulk proteomic approaches have identified molecular signatures of AD but have masked critical cellular heterogeneity—a significant limitation given that protein clearance systems operate differently across distinct brain cell types [52] [45].
Single-cell and spatial proteomics technologies now provide unprecedented resolution to study this heterogeneity, enabling researchers to investigate clearance pathways within individual cells and their specific pathological microenvironments [52] [70]. These advanced methodologies reveal cellular subtypes and interactions that were previously obscured, offering new insights into how different cells contribute to protein aggregation and clearance in AD [70]. This technical guide explores how these cutting-edge proteomic approaches are reshaping our understanding of cellular heterogeneity in AD clearance pathways, with practical methodologies and applications for researchers and drug development professionals.
Core Technologies and Methodological Approaches
Mass Spectrometry-Based Single-Cell Proteomics
Mass spectrometry (MS)-based approaches have evolved significantly to address the challenges of low protein abundance in single cells. Data-independent acquisition (DIA) methods, particularly diaPASEF (trapped ion mobility spectrometry coupled with DIA), have emerged as powerful tools for single-cell proteomics [71]. The diaPASEF approach enhances sensitivity by focusing MS/MS acquisition on the most productive precursor population while excluding most singly charged contaminating ions [71].
Key Experimental Protocol for DIA-based Single-Cell Proteomics:
- Sample Preparation: Utilize simulated single-cell-level proteome samples consisting of tryptic digests of cells (e.g., human HeLa cells) with total protein abundance of 200 pg to mimic single-cell input [71]
- Instrumentation: Analyze samples using timsTOF Pro 2 mass spectrometer with diaPASEF acquisition [71]
- Data Analysis: Employ specialized software tools (DIA-NN, Spectronaut, or PEAKS Studio) for peptide identification and quantification [71]
- Bioinformatic Processing: Implement sparsity reduction, missing value imputation, normalization, and batch effect correction to handle unique challenges of single-cell data [71]
Table 1: Performance Comparison of DIA Analysis Software for Single-Cell Proteomics
| Software Tool | Proteome Coverage (Proteins/Run) | Quantitative Precision (Median CV) | Key Strengths |
|---|---|---|---|
| Spectronaut (directDIA) | 3,066 ± 68 | 22.2-24.0% | Highest detection capabilities |
| DIA-NN | 2,607 (shared proteins) | 16.5-18.4% | Best quantitative accuracy |
| PEAKS Studio | 2,753 ± 47 | 27.5-30.0% | Balanced performance |
Multiplexed Antibody-Based Spatial Proteomics
Spatial proteomics techniques preserve architectural context while enabling high-plex protein detection. Two prominent methods include:
CODEX (Co-detection by indexing) Technology:
- Principle: Uses DNA-barcoded antibodies with fluorescent imaging [70]
- Protocol Enhancements: Pretreatment of formalin-fixed paraffin-embedded brain sections with hydrogen peroxide under LED lights to suppress autofluorescence [70]
- Multiplexing Capacity: Up to 32-100 protein markers simultaneously [70]
- Image Analysis: Custom algorithms (e.g., OTSM - Otsu's Thresholding-based Segmentation and Merge) to trace complex cellular morphologies and resolve microglial tentacles [70]
MIBI-TOF (Multiplexed Ion Beam Imaging by Time of Flight):
- Principle: Employs antibodies tagged with elemental isotopes detected via mass spectrometry [70]
- Resolution: Nanometer-level resolution across entire tissue sections [70]
- Advantage: Bypasses fluorescence limitations, enabling high-plex protein detection without spectral overlap [70]
Key Research Findings in Alzheimer's Disease
Cellular Heterogeneity in Clearance Systems
Spatial proteomics has revealed remarkable cellular heterogeneity in AD clearance pathways. Studies using CODEX-CNS have identified distinct microglial subtypes surrounding Aβ plaques, including a previously unrecognized population expressing both microglial (TMEM119) and macrophage (CD163) markers [70]. These "hybrid" cells suggest either infiltration of perivascular macrophages into the parenchyma or microglial transition to a macrophage-like state in plaque environments [70].
Furthermore, analyses of nearly 50,000 microglia across AD and control brains have revealed 10 transcriptionally distinct subpopulations based on protein expression patterns [70]. Plaque-associated microglia showed reduced expression of phagocytic marker CD68 and homeostatic marker TMEM119, suggesting that the plaque microenvironment alters microglial function, potentially impairing clearance capabilities [70].
Novel Molecular Insights into Clearance Mechanisms
Multi-cohort analyses of AD brain tissues have identified 866 consensus proteins with altered expression in AD [52] [45]. When compared to AD mouse models, 108 of these proteins were consistently altered in both humans and mice, with approximately 40% originating from microglia, followed by neurons and astrocytes [52]. This conserved proteomic signature highlights the interplay between different cell types in clearance pathways.
Complementing these findings, a 2024 study combining CSF proteomics with Aβ and tau PET imaging identified 127 differentially abundant proteins along the AD spectrum [72]. The strongest Aβ-associated proteins (SMOC1, ITGAM) were primarily expressed in glial cells, while tau-associated proteins were preferentially expressed in neurons and linked to ATP metabolism [72]. This cell-type-specific signature underscores the differential involvement of clearance mechanisms across cell types.
Table 2: Key Cell-Type-Specific Proteins in Alzheimer's Disease Clearance Pathways
| Protein | Primary Cell Expression | Association with AD Pathology | Potential Role in Clearance |
|---|---|---|---|
| SMOC1 | Glial cells | Strongly associated with Aβ pathology | Early response to Aβ accumulation |
| ITGAM | Microglia | Associated with both Aβ and tau pathology | Immune response modulation |
| GPNMB | Microglia | Consensus AD-associated protein | Lysosomal function, lipid metabolism |
| NPTX2 | Neurons | Consensus AD-associated protein | Synaptic function, network activity |
| FABP3 | Neurons | Associated with tau pathology | Energy metabolism, lipid transport |
| MFN2 | Neurons | Associated with tau-resilient neurons | Mitochondrial fusion, cellular defense |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Single-Cell and Spatial Proteomics
| Reagent/Platform | Type | Key Function | Application in Clearance Pathways |
|---|---|---|---|
| Olink Platform | Affinity-based proteomics | Dual antibody-based probes detect >5,400 proteins from ~6 µL sample | Biomarker discovery in biofluids, patient stratification |
| SomaScan Platform | Aptamer-based proteomics | DNA aptamers measure up to 11,000 proteins from ~50 µL sample | Large-cohort studies, biomarker validation |
| CODEX Antibody Panels | DNA-barcoded antibodies | Multiplexed spatial imaging of 32-100 protein markers | Cellular neighborhood analysis, microglial subtypes |
| MIBI-TOF Antibody Panels | Metal-tagged antibodies | Nanometer-resolution spatial proteomics with 36+ markers | Subcellular localization, pathological microenvironment |
| TMT (Tandem Mass Tag) | Isobaric labeling | Quantification of 10,000+ proteins across 35 samples | Deep proteome profiling, post-translational modifications |
Experimental Workflows and Signaling Pathways
Integrated Workflow for Spatial Proteomics in Clearance Studies
Cellular Interactions in Protein Clearance Pathways
Discussion and Future Perspectives
The application of single-cell and spatial proteomics to Alzheimer's disease clearance pathways has fundamentally transformed our understanding of cellular heterogeneity in protein aggregation disorders. These technologies have revealed previously unappreciated cellular states and interactions, particularly in microglial subpopulations that respond differently to proteinopathies [70]. The identification of specific proteins associated with resilient neurons—such as MFN2-rich neurons that resist tau tangle formation—opens new avenues for therapeutic development aimed at enhancing endogenous clearance mechanisms [70].
Future directions in this field should focus on increasing the scalability of these techniques to enable larger cohort studies, integrating spatial proteomics with other omics modalities, and developing more dynamic functional assays to complement snapshot spatial data. As these technologies become more accessible and standardized, they promise to uncover novel therapeutic targets that modulate specific cellular responses in protein clearance pathways, ultimately contributing to more effective interventions for Alzheimer's disease and related proteinopathies.
In Alzheimer's disease (AD) research, the focus is increasingly shifting beyond the mere presence of pathological proteins like amyloid-β (Aβ) and tau to the dynamic equilibrium of protein aggregation and clearance. The efficient clearance of protein aggregates from the brain is a critical biological process, the failure of which is now recognized as a central mechanism in AD pathogenesis. Cerebrospinal fluid (CSF) and blood serve as key conduits in this clearance system. The glymphatic system facilitates the efflux of soluble protein aggregates from the brain interstitial fluid into the CSF, from which they ultimately reach the peripheral circulation for removal [73] [74]. This process is vital for maintaining proteostasis, and its dysfunction leads to the accumulation of cytotoxic species. The recent emergence of minimally invasive blood-based biomarkers (BBMs) has revolutionized our ability to probe these clearance pathways in vivo, offering a window into brain pathology and enabling the development of sophisticated assays to track the fate of protein aggregates. Understanding these clearance mechanisms is fundamental to developing new therapeutic strategies aimed at enhancing the brain's innate capacity to remove pathogenic proteins.
Current Landscape of CSF and Blood-Based Biomarkers
The diagnostic and research landscape for Alzheimer's disease is being transformed by the validation and clinical implementation of biomarkers that reflect core pathological features. The following table summarizes the key biomarkers currently in use and under investigation.
Table 1: Key Biomarkers in Alzheimer's Disease Diagnosis and Research
| Biomarker | Biological Fluid | Pathological Correlation | Primary Utility |
|---|---|---|---|
| Amyloid-β 42/40 Ratio | CSF, Blood [75] | Amyloid plaque pathology | Detecting the presence of cerebral amyloidosis; lower ratio indicates pathology [75] |
| p-tau217 | CSF, Blood [76] [75] | Both amyloid and tangle pathology | Highly accurate for identifying AD pathology; strong predictor of dementia [76] [75] |
| p-tau181 | CSF, Blood [77] [75] [78] | Tau tangle pathology | Aids in ruling out AD pathology; associated with dementia risk [77] [75] |
| Neurofilament Light (NfL) | CSF, Blood [75] | Non-specific neuronal injury | Marker of neuroaxonal damage; predicts general dementia risk [75] |
| Glial Fibrillary Acidic Protein (GFAP) | CSF, Blood [75] | Astrocyte activation | Marker of neuroinflammation and astrogliosis; predicts dementia risk [75] |
The performance of these biomarkers, particularly in blood, has been rigorously evaluated. For instance, the Lumipulse G pTau217/ß-Amyloid 1-42 Plasma Ratio test demonstrated that 91.7% of individuals with positive results had amyloid plaques confirmed by PET or CSF, and 97.3% with negative results were truly negative [76]. Similarly, in a community-based study, elevated levels of p-tau181, p-tau217, NfL, and GFAP showed strong predictive performance for 10-year all-cause and AD dementia, with negative predictive values (NPVs) exceeding 90%, although positive predictive values (PPVs) remained low [75]. This high NPV is the foundation for the recent FDA clearance of Roche's Elecsys pTau181 test for use in primary care to rule out Alzheimer's-related amyloid pathology [77] [78].
To guide appropriate use, the Alzheimer's Association has released clinical practice guidelines establishing performance thresholds for BBMs in specialized memory care. They recommend that BBMs with ≥90% sensitivity and ≥75% specificity can be used as a triaging test, while tests with ≥90% for both sensitivity and specificity can serve as a substitute for PET or CSF testing [79]. This framework ensures that these powerful tools are applied responsibly to improve diagnostic accuracy and accessibility.
Experimental Protocols for Biomarker and Clearance Assay Development
Protocol: Single-Aggregate Analysis for Characterization of Protein Aggregates in Biofluids
This protocol details a suite of biophysical methods for the specific detection and characterization of individual protein aggregates in CSF and serum, as employed by Lobanova et al. (2021) [73].
- Objective: To quantify the number, size, and protein composition of individual β-sheet structured aggregates in biofluids from patients with neurodegenerative disease compared to controls.
- Sample Preparation: Collect CSF and serum via lumbar puncture and venipuncture, respectively. Process samples promptly (centrifuge at 20,000 × g for 30 minutes at 4°C to remove cells and debris) and store aliquots at -80°C. For immunodepletion, incubate serum with specific antibodies against α-synuclein and amyloid-β, followed by precipitation with protein A/G beads to remove targeted proteins [73].
- Single-Aggregate Imaging:
- Aptamer DNA-PAINT: Use DNA-conjugated aptamers or antibodies specific for β-sheet structures for target recognition. Employ transient binding of dye-labeled imager strands for super-resolution imaging. This allows for counting and sizing of individual aggregates down to nanometer resolution [73].
- Single-Aggregate Confocal Fluorescence Spectroscopy: Incubate biofluid samples with thioflavin T (ThT) or other amyloid-binding dyes. Use confocal microscopy with a diffraction-limited focus to detect bursts of fluorescence from single aggregates diffusing through the focal volume. Analyze fluorescence trajectories to determine aggregate size and concentration [73].
- High-Resolution Atomic Force Microscopy (AFM): Deposit a diluted biofluid sample onto a freshly cleaved mica surface. Allow adsorption, rinse with Milli-Q water, and air-dry. Image using AFM in tapping mode in air. Analyze AFM images to determine the morphology and height distribution of aggregates [73].
- Data Analysis: Correlate data from all three techniques. Determine the size distribution (e.g., 20 nm to 200 nm) and the proportion of larger aggregates (>150 nm). Following immunodepletion, calculate the relative composition of aggregates (e.g., α-synuclein vs. amyloid-β) based on the reduction in aggregate count [73].
Protocol: Validating Blood-Based Biomarkers Against Amyloid PET Status
This protocol outlines the core methodology for establishing the diagnostic accuracy of a plasma biomarker test, as seen in the FDA clearance study for the Lumipulse test [76].
- Objective: To evaluate the correlation between a blood-based biomarker ratio and the presence or absence of amyloid plaques as defined by the reference standard, amyloid PET.
- Study Population: Recruit a multi-center cohort of adult patients (e.g., n=499) who are cognitively impaired. Participants must undergo both a blood draw and the reference standard test (amyloid PET or CSF testing) within a defined timeframe [76].
- Biomarker Measurement: Collect blood into EDTA or heparin tubes. Process plasma by centrifugation (e.g., 2000 × g for 10 minutes) and store frozen at -80°C until analysis. Use a validated, automated immunoassay platform (e.g., the Lumipulse G system) to measure the concentrations of the target biomarkers (e.g., pTau217 and Aβ1-42) and calculate the predefined ratio [76].
- Statistical Analysis:
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) against the amyloid PET outcome.
- Report the percentage of indeterminate results (e.g., <20%).
- The performance benchmark for a "rule-out" test in a low-prevalence setting is a high NPV (e.g., 97.9%), ensuring that a negative result reliably excludes pathology [76] [78].
Visualization of Clearance Pathways and Experimental Workflows
The Protein Aggregation Clearance and "Proteinjury" Pathway
This diagram illustrates the pathway of protein aggregate clearance from the brain and how its failure leads to the "proteinjury" phenomenon, a mechanism of secondary neurodegeneration [73] [74].
Workflow for Single-Aggregate Analysis of Biofluids
This diagram outlines the experimental workflow for characterizing protein aggregates in serum and CSF using advanced biophysical methods [73].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of clearance assays rely on a specific set of reagents, analytical platforms, and biological materials. The following table details key components of this toolkit.
Table 2: Research Reagent Solutions for Biomarker and Clearance Assays
| Tool Category | Specific Examples / Assays | Function in Research |
|---|---|---|
| Validated Assay Platforms | Lumipulse G pTau217/β-Amyloid 1-42 Plasma Ratio [76], Elecsys pTau181 test [78] | Automated, quantitative measurement of specific biomarker concentrations in plasma or CSF for clinical validation studies. |
| Core Analytical Reagents | Phospho-specific Tau Antibodies (pTau181, pTau217) [76] [78], Amyloid-β Antibodies (Aβ40, Aβ42) [75], DNA-conjugated Aptamers [73] | Key reagents for immunoassays and super-resolution imaging, enabling specific capture and detection of target proteins and aggregates. |
| Biological Sample Collections | Characterized CSF and Serum/Plasma Banks (e.g., from cohorts like SNAC-K [75]) | Essential for assay validation; provide well-characterized, longitudinal samples from cognitively normal and impaired individuals. |
| Specialized Imaging Reagents | Thioflavin T (ThT), DNA-PAINT Imager Strands [73] | Enable detection and characterization of protein aggregates via fluorescence spectroscopy and super-resolution microscopy. |
| Reference Standard Materials | Synthetic Aβ and Tau Oligomers, Amyloid PET Imaging [76] | Serve as positive controls and gold standards for correlating blood/CSF biomarker levels with brain pathology. |
The pursuit of effective disease-modifying therapies for Alzheimer's disease (AD) remains hampered by a persistent translational gap between preclinical findings and clinical outcomes. Despite significant investment, only a limited number of treatments have demonstrated efficacy in slowing disease progression, with the majority of therapeutic candidates failing in human trials after showing promise in animal models [80] [81]. This disconnect raises critical questions about the validity of current preclinical models, particularly in recapitulating the complex clearance pathways essential for preventing toxic protein accumulation in the human brain.
Protein aggregation, specifically of amyloid-β (Aβ) and tau, represents a cardinal feature of AD pathology. The efficient clearance of these proteins through various pathways—including enzymatic degradation, cellular uptake, and transport across the blood-brain barrier (BBB)—is crucial for maintaining proteostasis. Dysfunction in these clearance mechanisms is increasingly recognized as a pivotal driver of AD pathogenesis [21] [52]. This whitepaper examines the utility and limitations of current animal models in studying these pathways, focusing specifically on their translational validity for investigating protein clearance mechanisms and their relevance to human disease.
Current Animal Models in AD Research
Transgenic Rodent Models
Transgenic mice expressing human mutations associated with familial AD (fAD) represent the most widely utilized models in preclinical research. These include models such as APP/PS1, 3×Tg, and 5×FAD, which incorporate mutations in genes encoding amyloid precursor protein (APP) and presenilins (PSEN1/2) to drive Aβ deposition [80] [82]. While these models have been instrumental in elucidating aspects of amyloid pathology, they predominantly represent the rare familial form of AD (<5% of cases), creating fundamental limitations for understanding the sporadic AD (sAD) that constitutes the vast majority of clinical presentations [80] [82].
A critical limitation of these models lies in their qualitative differences from human AD. Most fAD models fail to fully recapitulate the robust tau pathology, significant neurodegeneration, and brain atrophy characteristic of human AD [82]. When neurodegeneration does occur, it is typically modest and confined to discrete brain regions, raising questions about their ability to model the progressive neuronal loss observed in patients. Furthermore, the role of PSEN mutations in these models may drive pathological phenotypes through mechanisms independent of Aβ, as evidenced by studies showing that functional alterations persist in PSEN1 knock-in mutants even when amyloid pathology is reduced [82].
Alternative Mammalian Models
Beyond rodent models, researchers are exploring alternative mammalian species that may offer better recapitulation of human AD pathology. Canine cognitive dysfunction (CCD) in dogs represents a naturally occurring model that spontaneously develops amyloid plaques, tau pathology, and cognitive symptoms resembling human AD [83]. Non-human primates, particularly common marmosets, are also promising models due to their phylogenetic proximity to humans and age-dependent development of AD-like pathology [83]. These models may offer advantages for studying clearance pathways in a more physiologically relevant context, though their use is limited by practical considerations including cost, lifespan, and ethical concerns [83].
Table 1: Characteristics of Major AD Animal Models and Their Relevance to Clearance Pathways
| Model | Genetic Background | Key Pathological Features | Relevance to Clearance Pathways | Major Limitations |
|---|---|---|---|---|
| APP/PS1 | Human APP and PSEN1 mutations | Aβ plaques; minimal tau pathology; modest synaptic deficits | Limited translatable pathways identified; useful for studying amyloid deposition | Lacks key conserved pathways with human AD; poor predictor of therapeutic response [80] |
| 3×Tg | APPswe, PS1M146V, tauP301L | Aβ plaques; tau tangles; cognitive deficits | No translatable pathways identified in computational analyses | Limited conservation of pathway dysregulation with human AD [80] |
| 5×FAD | 5 familial APP/PS1 mutations | Rapid, aggressive Aβ deposition; synaptic loss | Preserves SREBP lipid synthesis and cytotoxic T-lymphocyte pathways shared with human AD | Overly aggressive pathology; may not reflect temporal progression in humans [80] |
| Canine CCD | Spontaneous age-related | Aβ plaques; tau pathology; cognitive decline | Naturally occurring BBB dysfunction; intact clearance pathway aging | Limited genetic tools; expensive maintenance [83] |
| Non-human Primates | Spontaneous or induced | Aβ plaques; sometimes tau pathology | Highly similar BBB and clearance mechanisms to humans | Ethical concerns; cost; long lifespan [83] |
Critical Limitations in Modeling Clearance Pathways
Qualitative and Quantitative Discrepancies
The translational validity of animal models for studying protein clearance pathways is limited by both qualitative and quantitative discrepancies from human AD. From a qualitative perspective, most transgenic models oversimplify AD pathology by focusing predominantly on amyloid accumulation while failing to fully recapitulate the multifactorial nature of the human disease, which frequently includes mixed pathologies such as α-synuclein and TDP-43 proteinopathies [81] [52]. This limitation is particularly relevant for clearance pathways, as different protein aggregates may compete for or overwhelm common clearance mechanisms.
Quantitative analyses reveal substantial differences in proteomic signatures between human AD and mouse models. A recent consensus analysis identified 866 proteins consistently altered in human AD brains, of which 654 were detected in mouse models [52]. However, only 108 of these proteins showed consistent alterations in both 5xFAD and APP-KI mouse models, with approximately 40% originating from microglia, followed by neurons and astrocytes [52]. This limited overlap highlights significant species-specific differences in proteomic responses to protein aggregation, potentially explaining why therapeutic strategies successful in mouse models frequently fail in human trials.
Temporal and Contextual Limitations
Animal models typically compress the disease timeline, with pathological changes occurring over months rather than decades. This accelerated progression fails to recapitulate the gradual dysfunction of clearance mechanisms that occurs during human aging and AD development [82]. The 5×FAD model, for instance, exhibits rapid and aggressive amyloid deposition, potentially overwhelming clearance mechanisms in a manner that does not reflect the slow progression of human AD [80].
Contextual factors, including genetic background and environmental conditions, further limit translational validity. Most transgenic models are maintained in controlled environments with standardized genetic backgrounds, failing to capture the complex gene-environment interactions that influence clearance pathway efficiency in human populations [82]. The absence of critical age-related systemic alterations—such as peripheral inflammation, metabolic dysfunction, and vascular aging—in laboratory-housed animals further reduces their ability to model the integrated system-wide failure of protein homeostasis that characterizes human AD [83].
Blood-Brain Barrier and Clearance Mechanisms
LRP1-Mediated Clearance Pathways
The blood-brain barrier plays a crucial role in regulating protein homeostasis within the brain, with low-density lipoprotein receptor-related protein 1 (LRP1) serving as a key transporter for Aβ clearance [21]. In healthy conditions, LRP1 facilitates the efflux of Aβ from the brain to the circulation through two primary trafficking pathways:
- PACSIN2-mediated transcytosis: Mid-avidity Aβ binding promotes association with PACSIN2, triggering tubular transcytosis that shuttles LRP1-Aβ complexes across endothelial cells for excretion, preserving LRP1 expression.
- Rab5-dependent degradation: High-avidity binding promotes clathrin-mediated endocytosis and Rab5-dependent sorting to lysosomes, leading to Aβ degradation but also LRP1 downregulation [21].
In AD, this balance is disrupted, with a shift toward Rab5-dependent degradation that reduces LRP1 surface expression and impairs Aβ clearance capacity [21]. This dysfunction is increasingly recognized as a critical event in AD pathogenesis, with studies demonstrating nearly undetectable BBB LRP1 levels in AD patients and animal models [21].
Diagram 1: LRP1 Trafficking Pathways in Aβ Clearance. The diagram illustrates the two major LRP1 trafficking routes that determine Aβ clearance efficiency and LRP1 homeostasis at the blood-brain barrier.
Modeling BBB Dysfunction in Animals
Current animal models partially recapitulate BBB dysfunction observed in human AD. Transgenic mice show age-dependent reduction in LRP1 expression and impaired Aβ clearance, mirroring trends seen in human patients [21]. Multi-modal imaging studies in APP/PS1 mice demonstrate progressive Aβ accumulation at the vascular level, with notable shifts in LRP1 localization from endothelial cells to pericytes during disease progression [21]. However, the timing and extent of these changes often differ substantially from human AD, with more rapid and severe BBB breakdown in many transgenic models.
Recent therapeutic approaches targeting BBB transport mechanisms highlight both the potential and limitations of current models. Nanocarriers engineered for mid-avidity LRP1 binding have demonstrated remarkable efficacy in mouse models, reducing brain Aβ levels by nearly 45% within hours and restoring cognitive function to wild-type levels [21] [84]. These interventions bias LRP1 trafficking toward PACSIN2-mediated transcytosis, effectively reprogramming endothelial trafficking to promote Aβ clearance [21]. While these findings underscore the utility of animal models for probing specific clearance mechanisms, their predictive value for human therapeutic response remains uncertain, particularly given the historical failures of other Aβ-targeting approaches that showed promise in preclinical studies.
Methodological Approaches and Assessment Techniques
Computational Assessment of Translational Validity
Advanced computational methods are increasingly employed to quantitatively evaluate the translational validity of animal models. Machine learning approaches analyzing pathway-level conservation rather than individual gene expression have revealed significant limitations in common AD models. One such workflow employing sparse principal component analysis and support vector machines on pathway enrichment scores found that APP/PS1 and 3×Tg models showed no translatable pathways conserved with human AD, while the 5×FAD model preserved dysregulation in SREBP-controlled lipid synthesis and cytotoxic T-lymphocyte pathways [80].
This methodology involves converting species-specific gene expression data into pathway enrichment scores, eliminating the need for direct gene-to-gene homolog mapping and preserving more biological context. The approach successfully predicted the clinical failure of ibuprofen for AD treatment based solely on preclinical microarray data, demonstrating potential utility for evaluating therapeutic candidates before advancing to human trials [80].
Table 2: Methodologies for Evaluating Clearance Pathways in Animal Models
| Methodology | Application | Key Parameters Measured | Technical Considerations | Translational Utility |
|---|---|---|---|---|
| Microarray Analysis with Machine Learning | Assessment of pathway conservation | Pathway enrichment scores; translatable pathways | Requires species-specific pathway mapping; dependent on data quality | Accurately predicted clinical failure of ibuprofen; identifies models with highest human relevance [80] |
| Proteomic Profiling (TMT/DIA MS) | Protein expression changes in brain tissue | Consensus protein alterations; cell-type specific signatures | Limited coverage of low-abundance proteins; ratio suppression in TMT | Identified 108 proteins consistently altered in both human AD and mouse models [52] |
| LRP1 Trafficking Assays | BBB transport efficiency | PACSIN2 vs. Rab5 pathway activation; LRP1 expression | Requires specialized endothelial isolation protocols | Revealed trafficking bias in AD models; basis for nanotherapeutic development [21] |
| Multimodal Imaging | Spatial distribution of pathology | Aβ-LRP1 colocalization; vascular deposition | Resolution limitations for microvascular changes | Demonstrated LRP1 shift from endothelial to pericytes in AD progression [21] |
| Behavioral Paradigms | Functional consequences of impaired clearance | Cognitive performance; learning and memory | Motor confounds; stress responses | Passive avoidance shows sensitivity to clearance restoration in mice [85] |
Experimental Protocols for Clearance Pathway Evaluation
LRP1 Trafficking and Aβ Clearance Assessment
Tissue Processing and Imaging Protocol:
- Perfuse transcardially with ice-cold PBS followed by 4% PFA under appropriate anesthesia
- Post-fix brains in 4% PFA for 24h, then transfer to 30% sucrose solution for cryoprotection
- Section coronally at 30μm thickness using a cryostat and collect free-floating sections
- Perform antigen retrieval with citrate buffer (10mM, pH 6.0) at 80°C for 30min
- Block with 5% normal goat serum + 0.3% Triton X-100 in PBS for 2h at room temperature
- Incubate with primary antibodies (anti-LRP1, anti-CD31, anti-Aβ, anti-CD146) in blocking solution at 4°C for 48h
- Incubate with species-appropriate fluorescent secondary antibodies for 2h at room temperature
- Mount sections and image using confocal microscopy with consistent laser settings across groups
- Quantify colocalization using Pearson's correlation coefficient or Mander's overlap coefficient [21]
Behavioral Assessment of Cognitive Function
Passive Avoidance Step-Down Protocol:
- Apparatus: Square chamber (50cm/side) with metal grid floor and elevated central platform (3.5cm height)
- Familiarization: Place animal on platform, record step-down latency, allow 10s exploration
- Learning Phase: Administer mild foot shock (50Hz, 1.5mA, 1s) upon platform descent
- Retention Test: At 24h post-learning, place animal on platform, measure step-down latency (60s maximum)
- Pharmacological Testing: Administer candidate therapeutic agents 24h post-retention test and repeat behavioral assessment [85]
This protocol leverages the natural tendency of rodents to step down from an elevated platform while assessing their ability to associate the platform with an aversive stimulus. Treatment with compounds that enhance protein clearance should improve retention test performance in AD models, as demonstrated in studies of LRP1-targeted nanotherapies where treated AD mice exhibited cognitive performance indistinguishable from wild-type controls [85] [84].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Clearance Pathways
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Animal Models | APP/PS1, 3×Tg, 5×FAD mice | Studying amyloid deposition and clearance mechanisms | 5×FAD shows highest pathway conservation with human AD; APP/PS1 suitable for rapid screening [80] |
| BBB Transport Modulators | LRP1-targeted polymersomes (A40-POs) | Restoring LRP1-mediated clearance | Mid-avidity binding biases trafficking toward transcytosis; reduces Aβ by 45% in mice [21] |
| Molecular Probes | Anti-LRP1, anti-CD31, anti-Aβ antibodies | Visualizing clearance components | Critical for assessing LRP1 localization shifts in disease progression [21] |
| Proteomics Platforms | TMT-MS, DIA-MS, Olink, SomaScan | Comprehensive protein profiling | TMT enables deep coverage; affinity platforms offer high sensitivity for biofluids [52] |
| Computational Tools | TransPath-C inspired workflows | Assessing translational relevance | Uses pathway enrichment scores rather than individual gene expression [80] |
| Behavioral Apparatus | Passive avoidance chamber | Assessing cognitive outcomes | Low motor demands suitable for impaired models; assesses aversive memory [85] |
The development of more clinically relevant animal models requires a multifaceted approach that acknowledges the complexity of protein clearance mechanisms in human AD. First, researchers should prioritize models that better recapitulate the multifactorial nature of AD, including co-pathologies (α-synuclein, TDP-43) and systemic alterations that impact brain clearance function [83] [52]. Naturally occurring models such as aged canines with canine cognitive dysfunction offer particular promise in this regard, as they develop AD-like pathology and symptoms spontaneously, including BBB dysfunction and impaired protein clearance [83].
Second, the integration of advanced computational methods for evaluating translational validity should become standard practice in preclinical studies. Machine learning approaches that assess pathway-level conservation rather than individual molecular changes provide a more realistic assessment of model relevance and therapeutic predictivity [80] [86]. These methods can help prioritize models and interventions most likely to succeed in human trials, potentially reducing the high failure rate of AD therapeutics.
Third, future research should focus on developing integrated assessment frameworks that combine multiple methodologies—including proteomics, advanced imaging, and functional outcomes—to evaluate clearance pathway function across species [52]. The identification of consensus protein alterations in human AD provides a valuable benchmark for assessing model validity, particularly for the 108 proteins consistently altered in both human AD and mouse models [52].
In conclusion, while animal models remain essential tools for studying clearance pathways in AD, their limitations must be acknowledged and addressed through rigorous validation against human data. The development of models that better recapitulate the complex, multifactorial nature of AD—including the systemic and age-related factors that influence protein clearance—will be essential for bridging the translational gap and developing effective therapies targeting proteostasis failure in Alzheimer's disease.
Overcoming Therapeutic Hurdles: Challenges in Enhancing Clearance and Preventing Pathological Spread
The accumulation of toxic protein aggregates is a pathological hallmark of neurodegenerative diseases, most notably Alzheimer's disease (AD). The amyloid-β (Aβ) cascade hypothesis posits that the accumulation of Aβ peptides in the brain initiates a pathological cascade leading to neuronal dysfunction and cognitive decline [87]. While early research focused predominantly on the overproduction of these pathological proteins, emerging evidence demonstrates that impaired clearance mechanisms play an equally critical, if not dominant, role in protein accumulation, particularly in sporadic, late-onset AD [15] [87]. The efficiency of these clearance pathways declines substantially with advancing age, the primary risk factor for neurodegenerative conditions [15] [7]. This whitepaper examines the mechanisms underlying the age-related decline in protein clearance efficiency, details experimental approaches for its investigation, and explores emerging therapeutic strategies aimed at reversing this decline to combat neurodegenerative diseases.
Core Clearance Pathways and Their Age-Related Dysregulation
The brain employs multiple, overlapping systems to remove metabolic waste and misfolded proteins. The progressive failure of these systems with age creates a permissive environment for the accumulation of pathogenic proteins like Aβ and tau.
Blood-Brain Barrier (BBB) Transport
The BBB serves as the primary interface for solute exchange between the brain and the periphery and is responsible for a significant portion (approximately 75%) of soluble Aβ clearance [15]. This transport is predominantly mediated by specific efflux transporters, including low-density lipoprotein receptor-related protein 1 (LRP1) and P-glycoprotein (P-gp), located on the abluminal side of cerebral endothelial cells [87] [88].
Age-Related Decline: The expression and functionality of these critical transporters diminish with age. Research has shown that LRP1 expression declines in aging rats, a change that is negatively correlated with the concentration of Aβ in brain cortex homogenates [89]. This age-dependent reduction in transporter activity significantly impairs the efflux of Aβ from the brain to the bloodstream, contributing to its cerebral accumulation [88].
The Glymphatic System and Interstitial Fluid Bulk Flow
The glymphatic system is a glial-dependent perivascular network that facilitates the clearance of soluble proteins and metabolites from the brain interstitial fluid (ISF) [15]. It functions via a convective flow mechanism, driven by arterial pulsation, which directs ISF and its solutes toward perivenous spaces for eventual clearance into the cerebrospinal fluid (CSF) or peripheral lymphatics. The polarized localization of aquaporin-4 (AQP4) water channels on astrocytic endfeet is critical for this process [15].
Age-Related Decline: Glymphatic function is highly vulnerable to aging. A key alteration is the mislocalization of AQP4 channels, which impairs the efficient exchange of CSF and ISF [15]. Furthermore, age-related reductions in arterial pulsatility diminish the driving force for this convective flow. This system is also highly regulated by sleep-wake cycles, with its activity being markedly enhanced during sleep; thus, age-related sleep disturbances further contribute to its functional decline [15].
Enzymatic Degradation
A plethora of proteases, collectively termed Aβ-degrading enzymes (ADE), are responsible for the catabolic clearance of Aβ within the brain [87]. Key enzymes include:
- Neprilysin (NEP): A membrane-bound metalloprotease that is a major contributor to Aβ degradation.
- Insulin-Degrading Enzyme (IDE): A zinc-metalloprotease that degrades both Aβ and insulin.
- Matrix Metalloproteinases (MMPs): A family of extracellular proteases, with MMP-9 being implicated in Aβ clearance.
Age-Related Decline: The expression and activity of multiple ADEs, including NEP and IDE, have been shown to decrease with advancing age [87]. This creates an enzymatic deficit, allowing more Aβ to escape degradation and accumulate in the extracellular space.
Cellular Clearance Mechanisms
a) Microglial Phagocytosis: Microglia, the resident immune cells of the brain, internalize and degrade soluble and fibrillar forms of Aβ via phagocytosis [87]. In early disease stages, this activity is thought to be protective. However, with aging, microglia become dystrophic and lose their phagocytic capacity [87]. An age-dependent shift in microglial phenotype toward a chronic pro-inflammatory state also contributes to impaired clearance and exacerbates neurotoxicity.
b) Autophagy-Lysosomal Pathway: Autophagy is an essential intracellular recycling process that degrades damaged organelles and protein aggregates through lysosomal hydrolases. This pathway is crucial for maintaining proteostasis, and its dysfunction is a hallmark of aging and neurodegeneration [90] [7].
Age-Related Decline: Multiple steps of the autophagy process become impaired with age, a phenomenon termed "autophagy decline". This includes:
- Reduced Initiation: Downregulation of core autophagy-related (ATG) proteins and altered signaling from upstream regulators like mTORC1 and AMPK [90].
- Impaired Lysosomal Function: Increase in lysosomal pH, leading to reduced activity of cathepsins and other acidic hydrolases, and decreased degradation capacity within autolysosomes [90] [7].
Table 1: Summary of Major Clearance Pathways and Their Age-Related Deficits
| Clearance Pathway | Key Molecular Components | Manifestation of Age-Related Decline |
|---|---|---|
| BBB Transport | LRP1, P-glycoprotein [88] | Reduced expression of efflux transporters [89] |
| Glymphatic System | AQP4, arterial pulsation [15] | AQP4 mislocalization, reduced pulsatility, sleep disruption [15] |
| Enzymatic Degradation | Neprilysin, IDE, MMP-9 [87] | Decreased expression and activity of degrading enzymes [87] |
| Microglial Phagocytosis | Phagocytic receptors [87] | Loss of phagocytic function, pro-inflammatory polarization [87] |
| Autophagy-Lysosomal System | ATG proteins, lysosomal hydrolases [90] [7] | Decline in autophagosome formation, reduced lysosomal degradation efficiency [90] |
Quantitative Assessment of Clearance Decline
The decline in clearance efficiency is not merely a qualitative observation but can be quantified through sophisticated kinetic modeling and biomarker analysis.
Kinetic Modeling of Aβ Turnover
Stable Isotope Labeling Kinetics (SILK) studies in humans have been instrumental in measuring the in vivo turnover rates of Aβ peptides. These studies involve administering a labeled amino acid precursor (e.g., 13C6-leucine) and sequentially sampling CSF to track the production and clearance of newly synthesized Aβ over 36-48 hours [89].
Key Findings:
- A non-steady-state physiological model decoupling CSF fluid transport from other processes revealed that changes in BBB transport and/or proteolysis are largely responsible for the age-related decline in Aβ turnover rates [89].
- The contribution of CSF-based clearance, while declining modestly with normal aging, becomes increasingly critical as other pathways (BBB/proteolysis) fail [89].
Table 2: Experimental Techniques for Assessing Clearance Efficiency
| Technique | Measured Parameters | Key Insights from Data |
|---|---|---|
| In Vivo SILK [89] | Fractional Turnover Rate (FTR) of Aβ peptides | Aβ turnover rates decrease significantly with age in humans [89] |
| Two-Photon Microscopy [15] | Real-time ISF solute movement, perivascular clearance | Visualized impairment of glymphatic flow in aged mouse models [15] |
| Biomarker Clocks (e.g., Epigenetic clocks) [91] | Biological age prediction based on DNA methylation | Successful interventions can reduce predicted biological age, indicating systemic rejuvenation [91] |
| In Vitro BBB Models (e.g., RBE4 cells) [88] | Transporter expression (Western Blot), 125I-Aβ40 transport quotient (TQ) | Quantifies drug effects on Aβ transport and transporter upregulation [88] |
Experimental Protocols for Investigating Clearance Mechanisms
Protocol: Stable Isotope Labeling Kinetics (SILK) for Aβ Kinetics
Objective: To measure the production and clearance rates of Aβ in the human central nervous system [89].
Methodology:
- Pre-infusion: An indwelling catheter is placed in the lumbar subarachnoid space for CSF sampling.
- Isotope Administration: A continuous intravenous infusion of 13C6-leucine is administered over several hours (e.g., 9 hours).
- CSF Sampling: CSF is collected hourly via the lumbar catheter for up to 36 hours. The volume of each withdrawal is carefully recorded (typically 6-10 mL).
- MRI Volumetry: Subject-specific MRI is performed to determine brain compartment volumes, which are used to refine the kinetic model.
- Sample Analysis: CSF samples are subjected to immunoprecipitation and mass spectrometric analysis to determine the enrichment of labeled Aβ peptides over time.
- Kinetic Modeling: Data is fitted to a multi-compartment physiological model to estimate the fractional turnover rates (FTR) and flux between compartments (e.g., ISF to CSF) [89].
Protocol: Assessing Glymphatic Function In Vivo
Objective: To evaluate the efficiency of the glymphatic system in a live animal model [15].
Methodology:
- Animal Preparation: Mice are anesthetized and placed in a stereotaxic frame.
- Tracer Infusion: A fluorescent tracer (e.g., fluorescently-dextran) is infused into the CSF via the cisterna magna.
- Experimental Conditions: Animals are maintained under physiological conditions controlling for factors known to affect glymphatic function, such as anesthetic state (mimicking sleep) or waking state.
- Tissue Processing: After a predetermined circulation time, the brain is harvested and fixed.
- Imaging and Analysis: Brain sections are imaged using confocal microscopy. Tracer distribution along perivascular spaces and its penetration into the brain parenchyma are quantified. Comparisons are made between young and aged animals, or between wild-type and AQP4-knockout animals [15].
Potential Reversal Strategies and Therapeutic Interventions
The understanding of clearance decline has opened new avenues for therapeutic intervention, ranging from pharmacological approaches to systemic rejuvenation strategies.
Pharmacological Enhancement of Clearance
Cholinesterase Inhibitors (ChEIs): Beyond their symptomatic effect, drugs like donepezil and rivastigmine have demonstrated disease-modifying potential. In vitro and in vivo studies show they enhance the clearance of 125I-Aβ40 across the BBB and in the liver. This enhanced clearance is concomitant with the upregulation of P-gp and LRP1 expression and is more pronounced in aged rats, leading to a significant reduction in endogenous brain Aβ levels [88].
Inducers of Proteolytic Activity: Strategies aimed at upregulating the expression or activity of Aβ-degrading enzymes (ADEs), such as neprilysin and IDE, represent a direct approach to bolstering enzymatic clearance [87].
Lifestyle and Physiological Interventions
Sleep Enhancement: Given the pronounced activity of the glymphatic system during sleep, interventions that improve sleep quality and duration may directly enhance the clearance of metabolic waste. Treating sleep disorders in the elderly could be a non-pharmacological strategy to slow the accumulation of pathogenic proteins [15].
Emerging Rejuvenation Strategies
Cellular Reprogramming: The in vivo partial reprogramming using Yamanaka factors (Oct4, Sox2, Klf4, with or without c-Myc) has shown promise in reversing age-related phenotypes. In progeria mouse models, this approach has been shown to reverse epigenetic age, restore visual function, and extend lifespan. This suggests that targeting the epigenetic drivers of aging can systemically restore function, including that of clearance pathways [91].
Autophagy Enhancement: Pharmacological or genetic strategies to boost autophagic activity are under active investigation. This includes the use of mTOR inhibitors (e.g., rapamycin) and AMPK activators. Restoring autophagic flux has been shown to extend lifespan in model organisms and protect against symptoms of proteostasis disorders [90] [7].
Lymphatic Stimulation: The recent discovery of meningeal lymphatic vessels has identified a new target for clearance enhancement. Preclinical studies suggest that enhancing meningeal lymphatic function, for instance through vascular endothelial growth factor C (VEGF-C) administration, can improve CSF drainage and reduce Aβ pathology [15].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Protein Clearance Mechanisms
| Reagent / Tool | Function/Application | Specific Example |
|---|---|---|
| Stable Isotope Tracers (e.g., 13C6-Leucine) [89] | Metabolic labeling for in vivo kinetic studies (SILK) in humans and animals | Measuring Aβ production and clearance rates [89] |
| Fluorescent Dextrans [15] | Tracers for visualizing and quantifying glymphatic flow in vivo | Assessing paravascular CSF-ISF exchange in mouse models [15] |
| AQP4 Knockout Mice [15] | Animal model for studying the specific role of the glymphatic system | Demonstrates the dependence of glymphatic flow on AQP4 channels [15] |
| Sandwich-Cultured Hepatocytes (SCHs) [88] | In vitro model for studying hepatic clearance of Aβ | Screening drugs for their ability to enhance peripheral Aβ clearance [88] |
| BBB Cell Models (e.g., RBE4 cells) [88] | In vitro model for studying transporter-mediated efflux at the BBB | Measuring 125I-Aβ40 transport quotient and transporter expression [88] |
| Epigenetic Clocks [91] | Biomarker for assessing biological age and rejuvenation | Quantifying the effect of interventions on systemic biological age [91] |
Visualizing Clearance Pathways and Therapeutic Targets
Diagram: Integrated Brain Clearance Pathways
The following diagram illustrates the major pathways involved in the clearance of amyloid-β and other waste products from the brain, highlighting sites of age-related dysfunction.
Diagram: Molecular Regulation of Autophagy in Aging
This diagram details the key molecular steps in the autophagy-lysosomal pathway and the specific points where this process declines during aging.
The age-related decline in the brain's capacity to clear itself of toxic protein aggregates represents a critical pivot point in the pathogenesis of neurodegenerative diseases. The failure is not isolated to a single system but is a multimodal collapse involving the BBB, the glymphatic network, enzymatic degradation, and cellular clearance mechanisms. The interplay between these pathways underscores the complexity of the problem but also reveals multiple therapeutic targets. Modern research, employing sophisticated kinetic modeling like SILK and biomarkers of biological aging, is now quantifying this decline and testing novel interventions. Promising strategies range from pharmacological enhancement of existing transporters and enzymes to groundbreaking rejuvenation approaches that aim to reset the aged epigenome and restore proteostatic capacity systemically. The future of combating neurodegenerative diseases may therefore lie not only in reducing the production of pathological proteins but, perhaps more importantly, in revitalizing the brain's innate, but aging, clearance machinery.
The deposition of aggregated proteins defines virtually all neurodegenerative disorders, including Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS). Protein accumulation and neurodegeneration typically proceed in a relatively stereotypical fashion for these diseases, which suggests cell non-autonomous factors drive pathology [92]. Recent studies have linked cell-to-cell propagation of pathology to molecular mechanisms reminiscent of prion pathogenesis, fundamentally reshaping our understanding of neurodegenerative disease progression [92]. This trans-cellular propagation of aggregated proteins occurs via templated conformational change, whereby an aggregated protein of a defined structure interacts with the native monomer and recruits it to a growing assembly [92].
The recognition that protein aggregates transfer between cells to propagate pathology is helping to define new treatment strategies for Alzheimer's disease and other proteinopathies [92]. Unlike classical prion diseases which are infectious, these prion-like propagation mechanisms in AD involve the spread of pathological proteins like amyloid-β (Aβ) and hyperphosphorylated tau (p-tau) along anatomical connections, ultimately leading to progressive cognitive decline [93] [94]. Understanding and blocking these transmission pathways represents a promising therapeutic avenue for halting disease progression.
Molecular Mechanisms of Propagation
The Template-Directed Misfolding Cycle
The core mechanism underlying prion-like propagation is templated conformational change, a process where an aggregated protein structure serves as a template to convert native folded proteins into the pathological conformation [92]. This process follows a specific molecular pathway:
- Cellular Release: Pathological protein aggregates escape the originating cell through various mechanisms, including exocytosis, exosomes, or through membrane damage [92].
- Transcellular Movement: The released aggregates enter neighboring cells, crossing synaptic connections or moving through the extracellular space [92].
- Seeding and Amplification: Inside the new cell, the internalized aggregate acts as a seed, recruiting endogenous native proteins and templating their conversion into the misfolded, aggregation-prone conformation [92] [94].
- Aggregate Growth: The newly converted proteins join the growing aggregate, which can itself fragment to generate new seeds, thereby amplifying the process [94].
This cycle leads to the progressive spread of pathology throughout connected brain networks, correlating with clinical symptom progression in Alzheimer's disease [92] [93].
Key Proteins and Their Structural Transitions
Several proteins central to neurodegenerative diseases demonstrate prion-like properties, undergoing specific structural transformations that enable their propagation.
Table 1: Proteins Exhibiting Prion-like Propagation Properties
| Protein | Native Function | Pathological Form | Primary Localization | Associated Diseases |
|---|---|---|---|---|
| PrP [92] | Cellular adhesion, stem cell renewal [93] | PrPSc (β-sheet-rich) [93] | Cell membrane (GPI-anchored) [93] | Creutzfeldt-Jakob Disease, GSS, FFI [93] |
| Aβ [92] | Derived from APP, function not fully defined [93] | Aβ plaques (β-sheet fibrils) [93] | Extracellular [92] | Alzheimer's Disease [92] |
| Tau [92] | Microtubule assembly and stabilization [93] | Hyperphosphorylated Tau (NFTs) [93] | Intracellular (axonal) [93] | Alzheimer's Disease, Frontotemporal Dementias [92] [94] |
| α-Synuclein [92] | Synaptic vesicle regulation [93] | Lewy bodies & neurites (α-Syn aggregates) [92] | Intracellular (presynaptic) [93] | Parkinson's Disease, Dementia with Lewy Bodies [92] [94] |
Prion Protein (PrP): The native cellular prion protein (PrPC) is a cell surface protein rich in alpha-helices. Its conversion to the pathological scrapie form (PrPSc) involves a dramatic structural transition to a beta-sheet-rich conformation that is highly insoluble and aggregation-prone [93]. This PrPSc form acts as a template that forces native PrPC molecules to adopt the same pathological conformation, enabling self-propagation [93].
Amyloid-β (Aβ) and Tau in Alzheimer's Disease: In AD, the two key pathological proteins, Aβ and tau, both exhibit prion-like characteristics. The amyloid-β peptide derives from the amyloidogenic processing of APP and aggregates into extracellular plaques [93]. The hyperphosphorylated tau protein dissociates from microtubules and forms intracellular neurofibrillary tangles (NFTs) [93]. Critically, both proteins can seed the aggregation of their native counterparts in a template-directed manner. Evidence from animal models confirms that brain homogenates from AD patients or synthetic Aβ fibrils can induce Aβ plaque formation in recipient animals, demonstrating the seeding capacity of Aβ aggregates [92]. Similarly, tau pathology spreads along connected neuronal pathways in a pattern consistent with trans-synaptic propagation [92].
Experimental Models and Methodologies for Studying Propagation
In Vitro Seeding and Propagation Assays
Cell-based models are fundamental for quantifying seeding activity and studying the initial steps of prion-like propagation. These assays typically involve exposing cultured cells expressing the native protein to pre-formed aggregates (seeds) of the pathological protein.
Table 2: Key Experimental Assays for Studying Prion-like Propagation
| Assay Type | Key Readouts | Technical Considerations | Applications in Alzheimer's Research |
|---|---|---|---|
| Seeded Aggregation in Cell Culture [92] | Reduction of soluble monomer, increase in insoluble aggregates, FRET-based aggregation sensors. | Seed preparation quality (sonication, size distribution), cell type (primary neurons vs. cell lines). | Demonstrating Aβ and tau fibrils seed aggregation of endogenous protein in acceptor cells [92]. |
| Transcellular Movement Assays [92] | Direct visualization of protein transfer (immunofluorescence, labeled aggregates), quantification of internalized aggregates. | Co-culture system design, distinguishing internalized from surface-bound aggregates. | Confirming α-synuclein and tau transfer between donor and acceptor cells in co-culture [92]. |
| Propagation of Aggregated State [92] | Detection of proteinase K-resistant aggregates in recipient cells (Western blot), secondary seeding capability. | Requires demonstration that transferred aggregates are capable of self-replication. | Showing that α-synuclein transferred between cells can template further misfolding [92]. |
Detailed Protocol: Seeded Aggregation Assay for Tau
- Seed Preparation: Synthesize recombinant tau protein and induce fibrillation using heparin in aggregation buffer (e.g., 20 mM HEPES, pH 7.4) with constant shaking at 37°C for several days. Confirm fibril formation by Thioflavin T fluorescence or electron microscopy. Sonicate the fibrils to generate short seeds that are more readily taken up by cells.
- Cell Treatment: Treat recipient cells (e.g., HEK293 cells expressing tau or primary murine neurons) with the sonicated tau seeds (e.g., 0.1 - 1 µM concentration). Include untreated controls and cells treated with non-aggregated tau monomer as negative controls.
- Detection of Aggregation: After 24-72 hours, lyse cells and fractionate lysates into soluble and insoluble (pellet) fractions via high-speed centrifugation. Analyze the insoluble fraction for pathological tau by Western blot using phosphorylation-specific antibodies (e.g., AT8 for pSer202/Thr205) or antibodies detecting conformational changes. Alternatively, fix cells and visualize aggregate formation via immunofluorescence microscopy [92] [94].
In Vivo Models of Pathology Spread
In vivo models are crucial for validating propagation in a physiological context and testing therapeutic interventions. Key approaches include:
Brain Lysate Injection Models: Inoculation of brain homogenates from human AD patients or aged transgenic mice into the brains of young APP-transgenic mice. This induces widespread Aβ plaque deposition that spreads from the injection site, demonstrating the seeding potential of Aβ aggregates [92].
- Methodology: Prepare sarkosyl-insoluble fractions from AD brain tissue or the cortex of APP/PS1 mice. Stereotactically inject small volumes (1-2 µL) of this homogenate (or control homogenate from healthy brain) into the hippocampus or cortex of young (e.g., 3-month-old) recipient mice. Analyze Aβ pathology 3-6 months post-injection using immunohistochemistry (e.g., 4G8, 6E10 antibodies) and thioflavin-S staining [92].
Fibril Injection Models: Direct injection of synthetic or recombinant pre-formed fibrils (PFFs) of Aβ or tau. This approach uses defined seeds and has shown that tau PFFs induce NFT-like pathology that spreads along connected circuits in both transgenic and wild-type mice [92] [93].
- Methodology: Generate PFFs from recombinant protein as described for in vitro assays. Confirm fibril morphology by atomic force microscopy (AFM) or electron microscopy. Perform stereotactic injection. Monitor the spatiotemporal spread of pathology over time using specific biomarkers and behavioral tests [92] [94].
Grafting Models: Transplantation of healthy neuronal precursor cells into the brains of transgenic mice expressing human α-synuclein. The observation of Lewy-body-like pathology in the grafted neurons weeks to months after transplantation provides strong evidence for the neuron-to-neuron spread of α-synuclein pathology, a key principle of prion-like propagation [92].
Therapeutic Strategies for Blocking Transmission
Therapeutic approaches targeting prion-like propagation aim to intervene at different stages of the seeding and spread cascade. These strategies can be broadly categorized as follows.
Direct Targeting of Protein Aggregates
This strategy uses small molecules or antibodies to stabilize the native protein, disrupt the pathological aggregates, or prevent the initial seed formation.
Table 3: Quantitative Data on Selected Antiprion and Prion-like Inhibitors
| Compound | Molecular Target / Proposed Mechanism | Experimental Model | Reported Efficacy (EC₅₀ or Effective Dose) | Key Findings / Clinical Status |
|---|---|---|---|---|
| (S)-Quinacrine [95] | PrPᶜ / PrPˢᶜ (multiple proposed mechanisms including direct binding, cholesterol redistribution) [96] | ScN2a cells (scrapie-infected neuroblastoma) [95] | EC₅₀ = 0.25 - 0.31 µM [95] | Stereoselective inhibition; (S)-enantiomer showed 2-6x greater potency than (R)-enantiomer in cells. Clinical trials for CJD showed mixed results [95]. |
| NPR-130 / NPR-162 [97] | PrPᶜ "hot spot" / Stabilizes native conformation, inhibits conversion [97] | Prion-infected cells / Prion-infected mice (in vivo) [97] | Significant PrPˢᶜ reduction in cells; prolonged survival in mice [97] | Identified via in silico screening (SBDD). Suppressed vacuolation, gliosis, and PrPˢᶜ accumulation in mouse brain [97]. |
| GN8 / MC Derivatives [97] | PrPᶜ / Stabilizes native conformation [97] | Prion-infected cells / Prion-infected mice (in vivo) [97] | IC₅₀ comparable to NPRs in cells; medicinal effect in animals [97] | Optimized GN8 derivatives stabilize PrPᶜ conformation and show therapeutic effect in animal models [97]. |
| A40-POs (Polymersomes) [21] | BBB LRP1 receptor / Biases trafficking toward transcytosis, promotes Aβ clearance [21] | APP/PS1 AD model mice [21] | ~45% brain Aβ reduction within 2 hrs; cognitive recovery to wild-type levels [21] | Multivalent modulation of BBB transport. Cognitive benefits persisted for up to 6 months post-treatment [21]. |
Structure-Based Drug Discovery (SBDD): This approach uses the 3D structure of the target protein to identify small molecules that bind tightly and stabilize the native state, preventing its conversion. For example, NPR-130 and NPR-162 were identified using in silico screening targeting a fragile "hot spot" region on PrPC. These compounds bind recombinant PrP, reduce PrPSc levels in infected cells, decrease aggresome formation, and significantly prolong survival in prion-infected mice [97]. This demonstrates the potential of SBDD for identifying effective aggregation inhibitors.
Immunotherapy: Antibodies that specifically recognize the pathological conformation of proteins like Aβ and tau can sequester seeds, block their cellular uptake, or promote their clearance by the immune system. For instance, anti-PrP antibodies such as Fab D18, 6H4, and ICSM18 have been shown to inhibit the interaction between PrPC and PrPSc [97]. In AD, antibodies targeting the N-terminal of Aβ can promote its clearance from the brain via the BBB [21].
Enhancing Cellular Clearance Pathways
Cellular protein quality control systems, including the ubiquitin-proteasome system (UPS) and autophagy, are responsible for clearing misfolded and aggregated proteins. Enhancing these pathways represents a complementary therapeutic strategy [60] [98].
Molecular Chaperones: Heat shock proteins (HSPs) like HSP70, HSP90, HSP40, and HSP27 play a critical role in protein homeostasis by preventing aggregation, assisting refolding, and targeting terminally misfolded proteins for degradation [98]. In AD, chaperone dysfunction contributes to pathogenesis. Strategies to boost chaperone function, such as upregulating HSF1 (the transcription factor controlling HSP expression), are being explored [98].
Modulating BBB Efflux Transport: The blood-brain barrier is not just a wall but an active clearance interface. In AD, the expression of LRP1, a major Aβ efflux transporter at the BBB, is dramatically reduced. A novel strategy using angiopep-2–conjugated LRP1-targeted polymersomes (A40-POs) was designed to modulate this transport. These polymersomes bind LRP1 with mid-level avidity, biasing its trafficking toward a non-degradative transcytosis pathway (PACSIN2-dependent). This not only promotes Aβ clearance but also upregulates LRP1 expression on the BBB, leading to rapid Aβ clearance (41% reduction within hours) and lasting cognitive recovery in AD mice [21].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Studying Prion-like Propagation
| Reagent / Tool | Category | Primary Function in Research | Example Applications & Notes |
|---|---|---|---|
| Recombinant Pre-Formed Fibrils (PFFs) [92] [94] | Protein Aggregates | Standardized seeds for inducing aggregation in vitro and in vivo. | Synthesized from Aβ, tau, or α-synuclein. Sonication is critical for generating uniform, small seeds for efficient cellular uptake [92]. |
| ScN2a Cells [95] | Cell Line | Persistently prion-infected neuronal model for screening antiprion compounds. | Used to evaluate EC₅₀ of compounds like quinacrine. Provides a robust system for quantifying PrPˢᶜ clearance [95]. |
| Proteinase K (PK) [92] [97] | Enzyme | Differential digestion; PrPˢᶜ and other pathological aggregates show partial PK resistance. | Key for Western blot analysis of PrPˢᶜ. The residual PK-resistant core is a hallmark of the pathological form [97]. |
| Conformation-Specific Antibodies [92] [97] | Antibodies | Detect pathological protein conformations (e.g., PrPˢᶜ, oligomers) specifically. | Examples: SAF83 (PrPˢᶜ), AT8 (phospho-tau). Crucial for immunohistochemistry and monitoring pathology spread [97]. |
| NUDE/DEGIMA Platform [97] | Software/Hardware | In silico screening platform for structure-based drug discovery. | Identified NPR compounds by docking ~690,000 compounds to the PrPᶜ "hot spot" [97]. |
| Surface Plasmon Resonance (SPR) [97] | Analytical Instrument | Quantifies binding affinity (KD) between candidate compounds and target proteins (e.g., recombinant PrP). | Validated the binding of NPR-130 and NPR-162 to recombinant PrP after in silico screening [97]. |
| APP/PS1 Transgenic Mice [21] | Animal Model | AD model exhibiting progressive Aβ pathology for in vivo propagation and therapy studies. | Used to test the efficacy of A40-POs, demonstrating rapid Aβ clearance and cognitive recovery [21]. |
The paradigm of prion-like propagation has fundamentally altered our understanding of neurodegenerative diseases, framing them as conditions where pathology spreads progressively through connected cellular networks. For Alzheimer's disease, this means that the classic distribution of Aβ plaques and tau tangles is not random but follows a predictable pattern of cell-to-cell transmission. This new framework provides a powerful explanation for the clinical progression of AD and related disorders.
The therapeutic implications are profound. Instead of solely targeting the symptoms or late-stage bulk protein accumulation, strategies can now be designed to block the propagation mechanism itself. Promising avenues include stabilizing the native conformation of proteins, developing seed-blocking antibodies, enhancing the brain's innate clearance mechanisms, and using sophisticated drug discovery platforms to identify novel inhibitors. The successful application of these strategies, however, relies on a deep and integrated understanding of both the molecular drivers of protein aggregation and the cellular systems responsible for their clearance. Future research must continue to bridge this gap, translating mechanistic insights into therapies that can halt the relentless spread of pathology in the human brain.
The blood-brain barrier (BBB) is a highly selective semi-permeable membrane that separates the circulating blood from the brain extracellular fluid, maintaining the delicate microenvironment required for proper neural function [27]. Comprising endothelial cells, pericytes, astrocytes, and tight junction proteins, the BBB regulates the transport of molecules into and out of the central nervous system (CNS) while restricting potentially harmful substances [99] [100]. In Alzheimer's disease (AD), BBB dysfunction emerges as a critical early pathological feature that significantly contributes to disease progression through impaired clearance of neurotoxic proteins, particularly amyloid-β (Aβ) and tau [101] [100] [102].
The BBB operates within the neurovascular unit (NVU), a complex network of cells that includes neurons and microglia alongside the traditional BBB components [99]. This dynamic interface controls cerebral homeostasis through tight junctions that seal paracellular pathways, specialized transport systems for essential nutrients, and efflux pumps that remove waste products [27] [100]. In AD, BBB dysfunction manifests through multiple mechanisms: disruption of tight junctions leading to increased permeability, altered expression of transporters affecting Aβ clearance, and inflammatory activation that further damages barrier integrity [103] [100]. Understanding and targeting these specific dysfunction mechanisms represents a promising therapeutic avenue for interrupting the pathological cascade of AD.
BBB Dysfunction in Alzheimer's Disease Pathogenesis
BBB impairment in AD establishes a vicious cycle where initial dysfunction promotes Aβ accumulation, which in turn further damages the barrier. The BBB is responsible for clearing approximately 80-85% of Aβ from the brain, primarily through receptor-mediated transcytosis [102]. Key transporters involved in this process include low-density lipoprotein receptor-related protein 1 (LRP1) for efflux and the receptor for advanced glycation end products (RAGE) for influx [101]. In AD, LRP1 expression is significantly downregulated at the BBB while RAGE expression is upregulated, creating an imbalance that favors Aβ accumulation in the brain [21] [101]. This impaired clearance capacity is further exacerbated by the degeneration of specific BBB cells, particularly pericytes, which show reduced numbers in AD models and post-mortem human tissues [100].
The pathological relationship between BBB dysfunction and AD is supported by multiple lines of evidence. Neuroimaging studies using dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) have consistently demonstrated increased BBB permeability in the hippocampi of patients with early AD and mild cognitive impairment (MCI) [100]. Post-mortem analyses of AD brain tissue reveal extensive leakage of blood-derived proteins such as fibrinogen and immunoglobulin into the brain parenchyma, along with structural alterations in tight junction complexes [100]. These changes correlate with cognitive decline severity and precede widespread neurodegeneration, positioning BBB dysfunction as an early event in AD pathogenesis rather than merely a secondary consequence [102].
Table 1: Evidence of BBB Dysfunction in Alzheimer's Disease
| Evidence Type | Methodology | Key Findings in AD | References |
|---|---|---|---|
| Neuroimaging | DCE-MRI | Increased BBB permeability in hippocampus and total gray matter | [100] |
| Neuroimaging | 7T SWI | ~78% of MCI/AD patients show cerebral microbleeds | [100] |
| Post-mortem Tissue | Immunohistochemistry | Diffuse staining of fibrinogen and immunoglobulin in brain tissue | [100] |
| Biomarker | CSF PDGFRβ | Increased levels indicating pericyte injury | [100] |
| Animal Models | APP/PS1 mice | Early progressive BBB dysfunction with decreased perfusion | [100] |
Therapeutic Strategies to Restore BBB Function
WNT/β-Catenin Signaling Activation
The WNT/β-catenin signaling pathway plays a fundamental role in development and maintenance of the BBB. Research has identified specific molecules that target this pathway to restore barrier integrity. A recent breakthrough identified L6-F4-2, a engineered molecule that selectively binds to the FZD4 receptor with 100-fold greater efficiency than natural ligands [104]. This molecule effectively activates WNT signaling, promoting BBB tight junction formation and reducing vascular leakiness in mouse models of Norrie disease and ischemic stroke [104].
In experimental models, treatment with L6-F4-2 demonstrated remarkable therapeutic potential. When administered to mice with genetic defects mimicking Norrie disease (which affects both the blood-retinal and blood-brain barriers), L6-F4-2 restored barrier integrity in the retina and cerebellum [104]. In ischemic stroke models, L6-F4-2 treatment significantly reduced stroke severity, improved survival rates, and reversed the leakiness of cerebral blood vessels [104]. These findings establish WNT activation as a promising strategy for restoring BBB integrity across multiple neurological conditions characterized by barrier dysfunction.
Table 2: Quantitative Outcomes of BBB-Directed Therapies in Preclinical Models
| Therapeutic Approach | Model System | Key Quantitative Outcomes | Significance | |
|---|---|---|---|---|
| FZD4-binding molecule L6-F4-2 | Mouse stroke model | Reduced stroke severity, improved survival, reversed vessel leakiness | First therapeutic class specifically targeting BBB repair | [104] |
| LRP1-targeted Polymersomes (A40-POs) | AD model mice | 45% reduction in brain Aβ within hours; 8-fold increase in plasma Aβ; 78% recovery of LRP1-CD31 colocalization | Rapid Aβ clearance and BBB restoration | [21] |
| LRP1-targeted Polymersomes (A40-POs) | AD model mice | Cognitive recovery lasting 6 months post-treatment | Sustained functional improvement | [21] |
LRP1-Mediated Clearance Pathways
Modulating LRP1-mediated transport represents another promising strategy for enhancing Aβ clearance at the BBB. Recent research has developed angiopep-2-conjugated LRP1-targeted polymersomes (A40-POs) engineered for intermediate binding affinity to LRP1 receptors [21]. These nanosized delivery systems are designed to bias LRP1 trafficking toward transcytosis rather than degradative pathways, thereby upregulating receptor expression and promoting efficient Aβ removal from the brain.
The avidity of ligand-receptor interaction critically determines the trafficking fate of LRP1. High-avidity binding promotes receptor clustering and recruitment of PICALM, triggering clathrin-mediated endocytosis and Rab5-dependent sorting toward lysosomal degradation [21]. In contrast, mid-avidity interactions engage PACSIN2 (syndapin-2), which generates and stabilizes tubular carriers that bypass the degradative pathway and enable rapid transcytosis of LRP1 across the BBB [21]. The A40-POs are specifically engineered for this mid-avidity binding, thereby reprogramming the intracellular trafficking of LRP1 to enhance its surface availability and Aβ clearance capacity. In AD model mice, this intervention achieved rapid clearance of 41% of brain Aβ within hours and restored cognitive function to wild-type levels, with benefits persisting for up to six months post-treatment [21].
Tight Junction Restoration and Inflammation Modulation
Beyond receptor-specific approaches, broader strategies targeting tight junction integrity and neuroinflammation show promise for BBB restoration in AD. These include compounds that enhance the expression of tight junction proteins such as claudin-5, occludin, and ZO-1, which are critical for maintaining the paracellular barrier [103] [100]. Additionally, anti-inflammatory agents that reduce endothelial activation and immune cell trafficking across the BBB may help break the cycle of neurovascular dysfunction and Aβ accumulation [99] [100].
The meningeal lymphatic system has emerged as another potential target for improving brain waste clearance. Although traditionally considered absent from the CNS, recent work has identified functional lymphatic vessels in the meninges that contribute to drainage of macromolecules from the brain [105]. Enhancing this lymphatic clearance through pharmacological or genetic approaches represents a novel strategy for compensating for impaired BBB function in AD. Dysfunction in these meningeal lymphatics has been linked to increased Aβ accumulation and cognitive impairment in mouse models, while their enhancement improves protein clearance [105].
Experimental Models and Methodologies
In Vitro BBB Models
Research on BBB function and therapeutic modulation relies heavily on in vitro models that replicate critical aspects of the neurovascular unit. These typically employ brain endothelial cells cultured in transwell systems, often in co-culture with astrocytes and pericytes to better mimic the native BBB environment [27]. These models enable quantitative assessment of barrier integrity through measurements of transendothelial electrical resistance (TEER) and paracellular permeability to tracer molecules [27]. For AD-specific research, these systems can be used to study Aβ transport across the barrier and to screen potential therapeutics for their effects on BBB function.
The experimental workflow for evaluating BBB-restorative compounds typically begins with high-throughput screening using in vitro models, followed by detailed mechanistic studies in more complex systems. Key parameters assessed include TEER measurements, expression levels of tight junction proteins (claudin-5, occludin, ZO-1), and functional transport assays for specific receptors such as LRP1 and RAGE [27]. These reductionist approaches allow for controlled manipulation of specific pathways and rapid evaluation of candidate therapeutics before proceeding to more complex in vivo models.
Diagram 1: Experimental workflow for evaluating BBB therapeutic candidates proceeds from in vitro screening to comprehensive in vivo validation.
In Vivo Assessment Techniques
In vivo evaluation of BBB-restorative therapies employs multiple sophisticated techniques to quantify barrier function and therapeutic efficacy. DCE-MRI represents the gold standard for non-invasively measuring BBB permeability in both animal models and human patients [100]. This method tracks the leakage of gadolinium-based contrast agents from blood into brain tissue, providing quantitative parameters of barrier integrity. In preclinical studies, this is often complemented with tracer techniques using Evans blue, sodium fluorescein, or fluorescent dextrans that are injected systemically and subsequently quantified in brain tissue following perfusion [103].
For AD-specific applications, these general BBB assessment methods are combined with techniques to monitor Aβ dynamics and cognitive outcomes. ELISA quantification of Aβ levels in brain homogenates and plasma provides direct measurement of clearance efficacy [21]. Immunohistochemical analysis of brain sections reveals the spatial distribution of Aβ plaques, tight junction proteins, and key transporters such as LRP1 [21] [100]. Cognitive behavioral tests, particularly the Morris water maze for assessing spatial learning and memory, serve as functional readouts of therapeutic efficacy in AD models [21]. These multifaceted approaches collectively provide comprehensive evaluation of potential BBB-restorative therapies.
Research Reagent Solutions
Table 3: Essential Research Reagents for BBB Dysfunction and Restoration Studies
| Reagent/Category | Specific Examples | Research Application | Key Functions | |
|---|---|---|---|---|
| BBB Integrity Reporters | Evans Blue, Sodium Fluorescein, FITC-Dextran | In vivo permeability assessment | Small molecule tracers that extravasate when BBB is compromised | [103] |
| BBB Integrity Reporters | Gadolinium contrast agents (DCE-MRI) | Clinical and preclinical imaging | MRI-visible tracers for quantifying BBB leakage | [100] |
| TJ Protein Antibodies | Anti-claudin-5, anti-occludin, anti-ZO-1 | Immunohistochemistry, Western blot | Visualization and quantification of tight junction components | [103] [100] |
| Transport Receptor Reagents | Anti-LRP1, anti-RAGE antibodies | Transport studies, localization | Assessing receptor expression and cellular distribution | [21] [101] |
| Specialized Cell Culture Systems | Brain endothelial cells, pericytes, astrocytes | In vitro BBB models | Recreating neurovascular unit for screening compounds | [27] |
| Engineered Therapeutic Molecules | L6-F4-2 (FZD4 agonist) | WNT pathway activation | Specific activation of BBB development signaling | [104] |
| Nanocarrier Systems | Angiopep-2-conjugated polymersomes (A40-POs) | Targeted drug delivery, LRP1 modulation | Enhancing receptor-mediated transcytosis, Aβ clearance | [21] |
| AD Model Systems | APP/PS1, 5XFAD transgenic mice | Preclinical therapeutic testing | Reproducing Aβ pathology with BBB dysfunction | [100] |
The strategic restoration of BBB function represents a paradigm shift in Alzheimer's disease therapeutics, moving beyond traditional approaches that target neural pathways alone. By addressing the fundamental clearance deficits that drive protein accumulation in AD, BBB-directed therapies offer potential for disease modification rather than symptomatic treatment. The development of specific molecules that target BBB integrity pathways, such as FZD4 receptors for WNT signaling activation and engineered polymersomes for LRP1-mediated transcytosis, demonstrates the feasibility of this approach with promising preclinical results [104] [21].
Future research directions should focus on optimizing delivery strategies for BBB-targeted therapeutics, exploring combination approaches that simultaneously address multiple aspects of barrier dysfunction, and identifying biomarkers to stratify patients most likely to benefit from these interventions. The continued elucidation of BBB biology in healthy aging and neurodegenerative states will undoubtedly reveal additional therapeutic targets. As these innovative strategies progress through clinical development, restoration of the blood-brain barrier may ultimately fulfill its potential as a transformative therapeutic foundation for Alzheimer's disease and other proteinopathies characterized by impaired clearance mechanisms.
The amyloid-β (Aβ) pathway remains central to Alzheimer's disease (AD) pathophysiology, with breakthroughs in molecular medicine positioning it as a cornerstone for therapeutic development [4]. Within this pathway, a critical dichotomy has emerged: the soluble, highly toxic Aβ oligomers versus the insoluble, largely inert amyloid plaques. The Aβ cascade hypothesis posits that an imbalance between Aβ production and clearance initiates a pathological cascade, with Aβ oligomers now recognized as the most toxic structures that drive synaptic dysfunction and neuronal damage [106] [4]. This understanding has reshaped therapeutic targeting, forcing a strategic reconsideration of whether to neutralize soluble oligomer toxicity or enhance clearance of insoluble plaques. The field is now moving beyond the simplistic view of amyloid accumulation to a more nuanced understanding of Aβ proteostasis, where distinct Aβ species interact differentially with other AD-related mechanisms including tau-mediated pathology, neuroimmune activation, and inflammatory responses [4]. This whitepaper examines the scientific rationale for targeting both oligomers and plaques within the broader context of protein aggregation clearance pathways, providing researchers with experimental frameworks and strategic considerations for advancing immunotherapeutic development.
Pathophysiological Background: Oligomers Versus Plaques
The Amyloid-β Pathway and Proteostasis Dysregulation
Aβ is generated through the sequential proteolytic cleavage of the amyloid precursor protein (APP) by β-secretase (BACE1) and γ-secretase. The prevailing view of AD pathogenesis centers on Aβ dyshomeostasis—an imbalance between production and clearance that leads to protein misfolding, aggregation, and accumulation [4]. In early-onset AD, this imbalance stems primarily from genetic-driven overproduction of Aβ, while in late-onset cases (the majority), impaired cerebral clearance mechanisms are predominant [4]. The aggregation process follows a molecular progression from monomeric Aβ to soluble oligomers, then to protofibrils and fibrils, and finally to insoluble amyloid plaques [106]. This temporal evolution occurs over decades, with Aβ accumulation beginning potentially 20-30 years before clinical manifestations [4].
The Central Paradox: Oligomer Toxicity Versus Plaque Inertia
Recent evidence has fundamentally shifted our understanding of which Aβ species drive neurodegeneration:
- Aβ Oligomers: These soluble aggregates are now considered the most toxic Aβ structures, directly inducing synaptic dysfunction, disrupting neuronal signaling, and triggering inflammatory responses [106]. Their toxicity stems from multiple mechanisms, including binding to cellular prion proteins and other receptors, initiating cascades that impair synaptic plasticity and lead to neuronal death [4].
- Amyloid Plaques: Historically considered the primary toxic entities, insoluble plaques are now viewed as relatively inert reservoirs that may sequester toxic oligomers but also serve as sources for oligomer release [106]. Plaques primarily drive pathology indirectly through physical disruption of brain architecture and by promoting chronic neuroinflammation through microglial and astrocytic activation.
Table 1: Comparative Characteristics of Aβ Oligomers and Plaques
| Characteristic | Aβ Oligomers | Amyloid Plaques |
|---|---|---|
| Solubility | Soluble | Insoluble |
| Toxicity Level | Highly toxic | Relatively inert |
| Primary Pathological Mechanism | Synaptic disruption, receptor interference | Physical architecture disruption, inflammatory activation |
| Detection Methods | Specialized immunoassays, conformation-specific antibodies | Histology, amyloid PET imaging |
| Therapeutic Targeting Approach | Neutralization, prevention of formation | Enhanced clearance, disaggregation |
| Temporal Appearance | Early in disease continuum | Later accumulation |
The recognition that oligomers and plaques represent distinct therapeutic targets with different pathological significances has profound implications for immunotherapy development, necessitating careful consideration of target engagement strategies.
Current Immunotherapeutic Landscape
Anti-Aβ Immunotherapy Approaches
Immunotherapeutic strategies for AD have evolved into two principal modalities: passive immunization through administered monoclonal antibodies and active immunization using vaccines to stimulate endogenous antibody production [106]. Both approaches must address the fundamental challenge of selectively targeting pathological Aβ species while sparing physiological Aβ forms and avoiding adverse effects.
Recent clinical successes with anti-Aβ monoclonal antibodies represent a significant milestone, with lecanemab and donanemab demonstrating ability to clear amyloid plaques and slow cognitive decline in early AD [106]. These antibodies share the common mechanism of binding Aβ and accelerating its clearance, yet differ in their precise epitope specificity and species preference, leading to variations in efficacy and safety profiles.
Strategic Targeting: Species-Specific Approaches
The choice of target Aβ species significantly influences therapeutic outcomes:
- Oligomer-Selective Approaches: SOBIN-AD, a novel peptide therapeutic, exemplifies targeted oligomer neutralization with its 27,000-fold stronger binding to toxic Aβ oligomers compared to protofibrils [107]. This exceptional selectivity enables precise engagement with the most toxic species while potentially minimizing mechanism-related adverse effects.
- Plaque-Targeting Approaches: Donanemab represents a plaque-specific strategy, recognizing a conformational epitope present only in deposited, fibrillar Aβ [106]. This approach aims to clear established amyloid pathology, with clinical trials demonstrating substantial plaque reduction.
- Broad-Spectrum Approaches: Some antibodies exhibit activity across multiple Aβ species, potentially offering broader pathological coverage but with increased risk of off-target effects.
Table 2: Comparative Analysis of Current Immunotherapeutic Approaches
| Therapeutic | Primary Target | Mechanism of Action | Clinical Stage | Key Findings |
|---|---|---|---|---|
| SOBIN-AD | Aβ oligomers | Selective oligomer binding, enhances microglial phagocytosis | Preclinical | 27,000-fold binding preference for oligomers; improves memory in AD mice [107] |
| Lecanemab | Protofibrils | Binds soluble Aβ protofibrils | FDA-approved | Clears amyloid plaques, slows cognitive decline by ~30% [106] |
| Donanemab | Fibrillar Aβ plaque | Targets deposited amyloid | FDA-approved | Significant plaque reduction, slows progression in early AD [106] |
| CT1812 | Oligomers at synapses | Displaces toxic oligomers from synapses | Phase 2B | Small molecule targeting both Aβ and alpha-synuclein oligomers [108] |
Experimental Approaches for Target Evaluation
Methodologies for Assessing Oligomer Toxicity and Engagement
Oligomer Binding Affinity Assays: Surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) provide quantitative measurements of therapeutic candidate binding to synthetic Aβ oligomers. The experimental workflow involves: (1) Preparation of homogeneous Aβ oligomer populations using standardized aggregation protocols; (2) Immobilization of oligomers or therapeutic candidates on sensor chips; (3) Measurement of binding kinetics (association/dissociation rates) and affinity constants; (4) Specificity validation against monomeric and fibrillar Aβ species [107].
Synaptic Function Protection Assays: Primary neuronal cultures exposed to synthetic Aβ oligomers enable evaluation of therapeutic protection. The protocol includes: (1) Culturing hippocampal neurons from embryonic rodents; (2) Treatment with well-characterized Aβ oligomer preparations; (3) Co-incubation with therapeutic candidates; (4) Assessment of synaptic density using immunostaining for PSD-95 and synaptophysin; (5) Measurement of long-term potentiation (LTP) using multi-electrode arrays to quantify functional rescue [4].
Methodologies for Evaluating Plaque Clearance
Microglial Phagocytosis Assays: These assays quantify the enhancement of Aβ clearance by innate immune mechanisms. The methodology involves: (1) Differentiation of human microglial cell lines or primary microglial cultures; (2) Incubation with pH-sensitive fluorescently labeled Aβ aggregates; (3) Treatment with therapeutic candidates; (4) Flow cytometry and confocal microscopy to quantify Aβ uptake and intracellular degradation; (5) Measurement of phagocytosis-related signaling pathways and receptor expression [107] [87].
In Vivo Plaque Burden Quantification: Transgenic AD mouse models enable longitudinal assessment of plaque clearance. The experimental protocol includes: (1) Treatment of Tg2576 or similar AD model mice with therapeutic candidates; (2) In vivo amyloid PET imaging at multiple timepoints; (3) Post-mortem brain sectioning and quantitative immunohistochemistry using antibodies against Aβ; (4) Image analysis to quantify plaque number, size, and total area; (5) Correlation with cognitive performance in behavioral tests [107].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Experimental Platforms
| Reagent/Platform | Function/Application | Key Characteristics |
|---|---|---|
| Tg2576 AD Mouse Model | In vivo therapeutic efficacy assessment | Overexpresses human APP with Swedish mutation; develops age-dependent Aβ pathology and memory deficits [107] |
| SOBIN-AD Peptide | Oligomer-selective targeting research | Binds Aβ oligomers with 27,000-fold preference over protofibrils; enhances microglial phagocytosis [107] |
| Conformation-Specific Antibodies | Selective detection of Aβ species | Distinguish between oligomeric, fibrillar, and plaque forms; essential for target engagement quantification |
| Amyloid PET Imaging | In vivo plaque burden quantification | Non-invasive longitudinal monitoring of plaque load; clinical correlation available [109] |
| Microglial Phagocytosis Assay | Clearance mechanism evaluation | Measures Aβ uptake and degradation by innate immune cells; key for mechanism validation [107] [87] |
| Surface Plasmon Resonance | Binding affinity and kinetics | Quantitative measurement of therapeutic candidate binding to various Aβ species [107] |
Integrated Clearance Pathways and Future Directions
Beyond Amyloid: Integration with Endogenous Clearance Mechanisms
The brain maintains sophisticated protein quality control systems that represent natural pathways for Aβ clearance, offering strategic opportunities for therapeutic enhancement:
- Enzymatic Degradation: Multiple Aβ-degrading enzymes (ADEs) have been identified, including neprilysin (NEP), insulin-degrading enzyme (IDE), matrix metalloproteinase-9 (MMP-9), and glutamate carboxypeptidase II (GCPII) [87]. These enzymes constitute a natural defense system against Aβ accumulation, with their expression and activity influencing disease progression.
- Cellular Clearance Mechanisms: Microglial phagocytosis represents the primary cellular pathway for Aβ clearance, with its efficiency critically determining Aβ homeostasis [87]. Microglia transition from protective phagocytic function in early disease to chronic inflammatory states in advanced stages, creating a therapeutic window for intervention.
- Interstitial Fluid Drainage: The bulk flow of interstitial fluid into the cerebrospinal fluid, followed by drainage through perivascular basement membranes (the glymphatic system), provides a physical clearance route that fails with aging and disease progression [87].
- Proteostasis Networks: The ubiquitin-proteasome system (UPS) and autophagy-lysosome pathway represent fundamental protein quality control mechanisms that maintain proteostasis. Dysregulation of these systems with aging contributes to Aβ accumulation [8].
Future Perspectives: Combination Therapies and Precision Medicine
The future of AD immunotherapy lies in strategic combinations and personalized approaches:
- Multi-Target Combination Therapies: The complexity of AD pathology necessitates addressing multiple targets simultaneously. Anti-amyloid therapies are increasingly being combined with tau-targeting approaches, anti-inflammatory agents, and neuroprotective compounds [110]. The PSP Platform Trial exemplifies an innovative framework for efficiently testing multiple treatment combinations under a single protocol [108].
- Staged Intervention Strategies: The temporal evolution of AD pathology suggests that optimal therapeutic approaches may vary by disease stage. Oligomer-targeting strategies may prove most beneficial in preclinical stages, while plaque-clearing approaches may be necessary once significant deposition has occurred [4].
- Biomarker-Guided Precision Medicine: Advances in blood-based biomarkers, including plasma p-tau181, p-tau217, p-tau231, neurofilament light chain (NfL), and glial fibrillary acidic protein (GFAP), enable more precise patient stratification and treatment monitoring [109] [111]. These tools facilitate the implementation of precision medicine approaches, matching the right therapeutic strategy to individual patient pathology.
- Beyond Amyloid and Tau: Emerging research highlights the importance of addressing co-pathologies such as alpha-synuclein and TDP-43, which frequently coexist with Aβ and tau pathology, particularly in older patients [110]. Future therapeutic combinations will need to address this pathological complexity.
The strategic balance between oligomer neutralization and plaque clearance continues to evolve as our understanding of Aβ biology deepens. The most promising approaches will likely involve precisely timed combinations that address both immediate synaptic protection and long-term pathological clearance, integrated with endogenous proteostasis mechanisms to achieve maximal therapeutic benefit across the AD continuum.
The accumulation of pathological proteins, primarily amyloid-β (Aβ) and tau, is a defining feature of Alzheimer's disease (AD) pathogenesis. The clearance of these aggregates depends on a complex network of interconnected biological pathways. The recognition that AD is a multifaceted disorder with numerous contributing pathological processes has positioned combination therapy as a necessary therapeutic approach [112]. While single-target therapies, such as anti-amyloid monoclonal antibodies (mAbs), demonstrate approximately 30% slowing of disease progression, a substantial 70% of cognitive decline remains unaddressed, highlighting the limitations of monotherapy and creating an imperative for more comprehensive treatment strategies [112] [113].
The scientific foundation for targeting multiple clearance pathways simultaneously rests on the dynamic equilibrium of Aβ in the brain, which is determined by the balance between its production and clearance [87]. In late-onset sporadic AD, which accounts for over 95% of cases, impaired clearance of Aβ—rather than its overproduction—is considered a key pathophysiological cause [114] [87]. Evidence from metabolic labeling studies on late-onset AD has demonstrated impaired Aβ clearance while Aβ production remains unchanged [114]. It is estimated that approximately 60% of Aβ in the brain is cleared via transport out of the central nervous system (CNS), while the remaining 40% undergoes degradation within the brain [114]. This division of labor among clearance mechanisms presents multiple synergistic targets for therapeutic intervention.
Key Clearance Pathways in Alzheimer's Disease
Enzymatic Degradation Pathways
Several Aβ-degrading enzymes (ADEs) play crucial roles in the proteolytic clearance of Aβ within the brain. A recent systematic review and meta-analysis revealed significant alterations in the levels of key ADEs in the brains of patients with AD [114].
Table 1: Key Amyloid-β Degrading Enzymes and Their Alterations in Alzheimer's Disease
| Enzyme | Change in AD Brain | Function | Correlation with Aβ Levels |
|---|---|---|---|
| Neprilysin (NEP) | Significantly altered | Zinc-metalloprotease that degrades soluble Aβ oligomers | Negative (r = -0.47) [114] |
| Insulin-Degrading Enzyme (IDE) | Significantly altered | Metalloprotease that degrades both Aβ and insulin | Not specified |
| Matrix Metalloproteinase-9 (MMP-9) | Significantly altered | Protease degrading extracellular matrix components and Aβ | Not specified |
| Cathepsin D | Significantly altered (SMD = 1.24) | Lysosomal aspartyl protease involved in Aβ degradation | Not specified |
The meta-analysis found that the levels of insulin-degrading enzymes, neprilysin, matrix metalloproteinase-9, and cathepsin D are significantly altered in the brains of patients with Alzheimer's disease compared to healthy controls [114]. Notably, correlations were observed between Aβ levels and the levels of neprilysin (r = -0.47) in patients with Alzheimer's disease, supporting its role as a key therapeutic target [114].
Cellular Clearance Mechanisms
Microglial cells, the brain's resident mononuclear phagocytes, play an essential role in Aβ clearance through their ability to take up and degrade soluble and fibrillar forms of Aβ [87]. The triggering receptor expressed on myeloid cells 2 (TREM2) has emerged as a critical regulator of microglial function, with meta-analyses showing significant changes in TREM2 levels in both brain (SMD = 0.31) and peripheral blood (SMD = 1.01) samples of AD patients, and a positive correlation with Aβ levels (r = 0.16) [114]. In early stages of AD, microglial activation delays disease progression by promoting clearance of Aβ through phagocytosis, but with aging, microglia become over-activated and lose their phagocytic ability, instigating inflammatory reactions that cause neuronal damage [87].
Blood-Brain Barrier Transport and Perivascular Drainage
The transport of Aβ across the blood-brain barrier (BBB) represents a major clearance pathway, with P-glycoprotein (P-gp) playing a particularly important role. Meta-analyses have shown significant alterations in P-gp in the brains of AD patients, with a negative correlation between P-gp function and Aβ levels (r = -0.31) [114]. The interstitial fluid (ISF) drainage pathway through perivascular Virchow-Robin spaces provides another critical clearance route, with failure of this system contributing to cerebral amyloid angiopathy (CAA), which is present in approximately 90% of AD patients [87].
Diagram 1: Aβ Clearance Pathways. This diagram illustrates the major clearance mechanisms for amyloid-β in the brain, showing how multiple pathways contribute to Aβ removal.
Current Combination Therapy Approaches in Clinical Development
Anti-Amyloid and Anti-Tau Combinations
The combination of anti-amyloid and anti-tau therapies represents a central focus in the field, with several clinical trials currently investigating this approach [115]. The DIAN-TU study (NCT06602258) exemplifies this strategy, where for patients with symptoms, lecanemab (an anti-amyloid mAb) is administered for 6 months, after which E2814 (an anti-tau agent) or placebo is added on [112]. This sequential combination approach recognizes the temporal relationship between Aβ accumulation (which occurs earlier) and tau pathology (which follows), attempting to target both key pathologies in a biologically rational sequence. Another trial (NCT06957418) plans to investigate tau-directed therapies, alone or in combination with donanemab, in individuals with late preclinical or early prodromal AD [113].
Targeting Inflammation and Immune Mechanisms
Combinations involving anti-inflammatory and immune mechanisms with anti-amyloid or other therapies also show significant promise [115]. COYA 302, for example, is a combination therapy intended to enhance the anti-inflammatory function of regulatory T cells (Tregs) and suppress inflammation produced by activated monocytes and macrophages [112]. The combination consists of low-dose interleukin-2 and abatacept and is being developed for subcutaneous administration for patients with neurodegenerative diseases including AD. The therapeutic hypothesis is that the two agents will have additive or synergistic effects by impacting several elements of the complex inflammatory network [112].
Table 2: Selected Active Clinical Trials of Combination Therapies for Alzheimer's Disease
| Trial Identifier | Phase | Population | Combination Therapy | Primary Completion |
|---|---|---|---|---|
| NCT06602258 [113] | 2 | Early AD | E2814 (anti-tau) + Lecanemab (anti-Aβ) | August 2027 |
| NCT05109169 (MET-FINGER) [112] [113] | 2 | At risk of dementia | Metformin + FINGER 2.0 lifestyle intervention | June 2027 |
| NCT05511363 (ADEPT-1) [112] [113] | 3 | AD with psychotic symptoms | KarXT (xanomeline + trospium chloride) | October 2026 |
| NCT04685590 (SToMP-AD) [113] | 2 | Amnestic MCI or early AD | Senolytic therapy (dasatinib + quercetin) | January 2028 |
| NCT06957418 [113] | 2 | Late preclinical or early prodromal AD | Tau-directed therapies ± donanemab | August 2028 |
Pharmacokinetic and Formulation-Based Combinations
Beyond combinations of pharmacodynamically active agents, innovative approaches include combinations designed to enhance blood-brain barrier penetration or reduce peripheral side effects. Trontinemab (NCT04639050), for instance, combines gantanerumab with a Brainshuttle technology that interacts with the transferrin receptor to facilitate antibody passage across the blood-brain barrier [112]. Similarly, the combination of dextromethorphan with bupropion (Auvelity) uses bupropion to inhibit the peripheral metabolism of dextromethorphan by blocking CYP2D6, thereby increasing its central availability [112].
Experimental Models and Methodologies for Evaluating Combination Therapies
Nonclinical Assessment Models
The evaluation of combination therapies targeting multiple clearance pathways relies on a range of nonclinical models. Animal models, particularly transgenic mice expressing human APP, PSEN1, and MAPT mutations, provide invaluable systems for studying the interplay between different clearance mechanisms [112]. New Approach Methodologies (NAMs), such as induced pluripotent stem cells (iPSCs) and brain organoids, offer human-relevant systems that can recapitulate complex cellular interactions and patient-specific pathophysiology [112]. These models enable researchers to investigate synergistic effects between different therapeutic mechanisms and assess potential toxicities before advancing to human trials.
Clinical Trial Designs for Combination Therapies
Clinical development of combination therapies presents unique methodological challenges. Phase 1 trials are required to characterize each member of a novel combination, while Phase 2 trials may use a 2-by-2 factorial design comparing each drug to placebo and the drug combination [112]. In Phase 3, comparison of the novel combination to standard of care may be sufficient, or more complex designs may be required [112]. The increasing use of anti-amyloid mAbs as standard of care creates both opportunities and challenges for future trials, which may need to evaluate novel agents as add-on therapies to existing approved treatments [113].
Diagram 2: Experimental Workflow for evaluating combination therapies. This diagram outlines the key stages in the development and evaluation of therapies targeting multiple clearance pathways.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Studying Clearance Pathways
| Research Tool Category | Specific Examples | Research Application |
|---|---|---|
| Cellular Models | Induced Pluripotent Stem Cells (iPSCs), Brain Organoids, Microglial Cell Lines | Human-relevant systems for studying cellular clearance mechanisms and screening compounds [112] |
| Protein Analysis Reagents | Anti-Aβ Antibodies, Anti-tau Antibodies, TREM2 Assays, Neprilysin Activity Kits | Quantifying target engagement, pathway modulation, and biomarker changes [114] |
| Animal Models | APP/PS1 Transgenic Mice, 3xTg-AD Mice, 5xFAD Mice, Tauopathy Models | In vivo assessment of target engagement, synergistic effects, and disease modification [112] |
| Computational Platforms | CKG-IMC Model, Protein-Protein Interaction Networks, AI-Based Drug Repurposing | Predicting compound-protein interactions and identifying novel combination candidates [116] |
| Biomarker Assays | CSF Aβ42/40, p-tau181, p-tau217, Plasma GFAP, Neurofilament Light Chain | Monitoring target engagement, pathway modulation, and treatment response [112] [114] |
The simultaneous targeting of multiple clearance pathways represents a paradigm shift in Alzheimer's disease therapeutics, moving beyond single-target approaches to address the multifactorial nature of the disease. The complex pathophysiology of AD, involving not only Aβ and tau but also neuroinflammation, synaptic dysfunction, and multiple co-pathologies, demands such comprehensive therapeutic strategies [112] [117]. As of 2025, combination therapies account for approximately 13% of all trials in the AD drug development pipeline, reflecting growing recognition of this approach's necessity [115].
Future advances in this field will depend on several key factors: improved understanding of the temporal sequence and interactions between different pathological processes; the development of biomarkers to guide patient selection and target engagement assessment; innovative clinical trial designs that can efficiently evaluate multi-component therapies; and enhanced collaboration between pharmaceutical companies, academic institutions, and regulatory agencies [112] [115]. Computational approaches, including artificial intelligence and network-based analysis of disease and drug interactions, validation in non-clinical models, and use of real-world data, may facilitate prioritization of candidates for combination treatments [112] [116]. As these efforts mature, combination therapies targeting multiple clearance pathways hold the promise of substantially improving outcomes for patients with Alzheimer's disease.
The progressive accumulation of protein aggregates, specifically amyloid-β (Aβ) and tau, is a defining pathological hallmark of Alzheimer's disease (AD). The efficacy of clearance pathways—including enzymatic degradation, transport across the blood-brain barrier (BBB), and glymphatic flow—diminishes with disease progression and aging. This whitepaper synthesizes current evidence to argue that therapeutic interventions aimed at enhancing clearance mechanisms demonstrate superior efficacy during early-stage pathological changes, often decades before clinical symptoms manifest. Targeting these pathways in late-stage disease presents significant challenges due to extensive irreversible neuropathology and overwhelmed endogenous clearance systems. We provide a comprehensive analysis of quantitative data, experimental methodologies for investigating clearance kinetics, and visualization of key pathways to guide future therapeutic development for researchers and drug development professionals.
In Alzheimer's disease (AD), the accumulation of toxic protein aggregates—specifically amyloid-β (Aβ) plaques and hyperphosphorylated tau tangles—results from an imbalance between production and clearance [15]. Emerging evidence indicates that impaired clearance mechanisms, rather than solely increased production, play a critical role in both early-onset (EOAD) and late-onset (LOAD) AD forms [15]. The brain employs multiple, overlapping systems for removing soluble waste proteins, which can be categorized by their operational compartments.
These clearance systems include degradation clearance (enzymatic breakdown and cellular uptake), blood-brain barrier clearance (transport from interstitial fluid to blood), interstitial fluid (ISF) bulk flow (including the glymphatic system), and cerebrospinal fluid (CSF) absorption into circulatory and lymphatic systems [15]. The relative contributions of these systems remain partially quantified, with historical research emphasizing BBB dominance while recent studies suggest substantial glymphatic involvement [15]. Critically, these systems function cooperatively to remove extracellular Aβ (eAβ), meaning dysfunction in any single pathway can contribute to pathological accumulation.
The fundamental processes governing protein aggregation follow a core reaction network applicable across biological systems: initiation (de novo aggregate formation), growth (aggregate enlargement), multiplication (generation of new aggregates), and removal (active clearance by biological systems) [118]. Therapeutic targeting of clearance mechanisms directly intervenes in this removal process, which represents the key distinction between aggregation in living systems versus in vitro environments [118].
Pathophysiological Basis for Early Intervention
The Preclinical Cascade of Alzheimer's Disease
Alzheimer's disease pathology begins decades before clinical symptoms emerge [15] [117]. During this extended preclinical stage, Aβ accumulation precedes and accelerates tau hyperphosphorylation and tangle formation, creating a pathological cascade where Aβ acts as the "trigger" and tau as the "bullet" [119]. This temporal sequence establishes a critical window for therapeutic intervention before irreversible neurodegeneration occurs.
Genetic and Biomarker Evidence: Studies of autosomal dominant EOAD caused by PSEN1, PSEN2, or APP mutations demonstrate that carriers exhibit both increased Aβ production and decreased Aβ clearance [15]. In contrast, individuals with LOAD primarily exhibit clearance impairment alone [15]. The strongest genetic risk factor for LOAD, the APOE ε4 allele, is implicated in multiple clearance pathways, including BBB transport and aggregate phagocytosis [15]. Biomarker studies reveal that decreased CSF Aβ42 levels, indicating cerebral plaque accumulation, can be detected years before symptom onset [15] [117].
The Clearance Impairment Trajectory: Multiple clearance systems exhibit age-related decline and are further impaired by AD pathology itself. Specifically, BBB efflux transporters (e.g., LRP1) show reduced expression in AD brains, while influx transporters (e.g., RAGE) demonstrate upregulated activity, creating a net imbalance that promotes Aβ retention [119]. The glymphatic system, which depends on astroglial aquaporin-4 (AQP4) channels and arterial pulsation, becomes less efficient with age and is further suppressed by sleep disturbances—a known AD risk factor [15]. Enzymatic degradation by neprilysin, insulin-degrading enzyme (IDE), and angiotensin-converting enzyme (ACE) also shows decreased activity in aging and AD brains [119].
Compensatory Mechanisms and System Overload in Early Stages
During early pathological stages, compensatory upregulation of remaining clearance pathways may temporarily maintain homeostasis. However, as aggregate burden increases, these systems become overwhelmed, creating a nonlinear progression toward clinical disease. The discovery of meningeal lymphatic vessels provides another potential clearance route that may offer therapeutic targets [15]. The interplay between oxidative stress and Aβ aggregation creates a "chicken and egg" relationship that further accelerates pathology once a critical threshold is crossed [119].
Table 1: Key Clearance Pathways and Their Alterations in Early AD
| Clearance Pathway | Primary Mechanism | Early AD Alterations | Therapeutic Implications |
|---|---|---|---|
| BBB Transport | Efflux via LRP1/P-gp; Influx via RAGE | ↓ LRP1 expression; ↑ RAGE activity; vascular dysfunction | Enhance efflux transporters; inhibit RAGE |
| Glymphatic Flow | AQP4-dependent ISF bulk flow | Impaired AQP4 polarization; sleep disruption | Improve sleep quality; target AQP4 function |
| Enzymatic Degradation | Proteolysis (neprilysin, IDE, ACE) | Reduced enzyme activity/expression | Enzyme upregulation; activator compounds |
| Lymphatic Clearance | Meningeal lymphatic drainage | Reduced drainage efficiency | Enhance lymphatic function |
| Cellular Uptake | Microglial phagocytosis | Impaired phagocytic function; APOE4-related deficits | Modulate microglial activity |
Quantitative Assessment of Therapeutic Windows
Temporal Dynamics of Aggregate Formation and Clearance
The kinetics of protein aggregation follow distinct principles that inform intervention timing. In vitro studies reveal that aggregation proceeds through a nucleated polymerization mechanism, where formation of initial aggregates (nucleation) is rate-limiting, but once seeds exist, growth and multiplication accelerate dramatically [118]. In living systems, this process spans decades rather than hours, with clearance mechanisms determining the pace of accumulation [118].
Rate-Limiting Steps: The identification of rate-determining steps in complex biological networks provides critical intervention targets. During early disease stages, aggregate initiation or cellular uptake may be rate-limiting, while in advanced disease, aggregate multiplication or overwhelmed clearance systems may control progression kinetics [118]. Pharmacological intervention should target the current rate-limiting step, which evolves throughout the disease course.
Biomarker Trajectories: Longitudinal biomarker studies demonstrate that CSF Aβ42 decreases begin up to 20 years before symptom onset, followed by tau increases approximately 15 years pre-diagnosis, with brain atrophy and cognitive changes emerging in the final 5-10 years [117]. This extended sequence provides multiple potential intervention windows, with clearance enhancement likely most effective during the initial Aβ deposition phase.
Table 2: Quantitative Parameters of Protein Aggregation and Clearance
| Parameter | In Vitro Values | In Vivo Estimates | Measurement Techniques |
|---|---|---|---|
| Aβ Production Rate | N/A | ~7.6% of total Aβ pool per hour [15] | Stable isotope labeling; CSF sampling |
| Aβ Clearance Rate | N/A | ~8.3% of total Aβ pool per hour (healthy) [15] | Stable isotope labeling; kinetic modeling |
| Aβ Half-Life | Hours (aggregation phase) | ~9 hours in human CNS [15] | Radiolabeled Aβ; PET imaging |
| Glymphatic Inflow | N/A | ~40% of CSF total volume exchanged | Two-photon imaging; contrast-enhanced MRI |
| Fraction Cleared via BBB | N/A | ~75% of total clearance (model estimates) [15] | Microdialysis; compartmental modeling |
| Fraction Cleared via ISF Bulk Flow | N/A | ~10-25% of total clearance (model estimates) [15] | Radioactive tracer studies |
Comparative Efficacy: Early vs. Late Intervention
Evidence from immunotherapy trials demonstrates substantially different outcomes based on intervention timing. The recent approvals of aducanumab and lecanemab, which primarily target aggregated Aβ, show modest clinical benefits in early AD patients but limited efficacy in moderate-to-severe disease [117]. Similarly, donanemab trials demonstrated greater slowing of cognitive decline in participants with lower tau burden [117].
Clearance Capacity Limitations: As AD progresses, the brain's total clearance capacity diminishes due to multiple factors: vascular dysfunction impairs BBB transport, AQP4 mislocalization reduces glymphatic efficiency, and chronic neuroinflammation alters microglial function [15] [119]. This creates a scenario where late-stage interventions must clear an extensive aggregate burden with diminished physiological capacity—a fundamental challenge explaining the limited success of late-stage therapeutics.
The Threshold Effect: Protein aggregation exhibits threshold behavior where initial accumulation is well-compensated until a critical point is reached, after which acceleration occurs due to saturable clearance mechanisms and enhanced secondary nucleation [118]. Interventions before this inflection point likely provide disproportionate benefits, as preventing aggregate multiplication is more efficient than clearing established aggregates.
Experimental Methodologies for Clearance Investigation
In Vivo Clearance Measurement Techniques
Stable Isotope Labeling Kinetics (SILK): This methodology involves intravenous administration of labeled leucine (13C6-leucine) that becomes incorporated into newly synthesized proteins, including Aβ. Sequential CSF sampling via indwelling catheter allows measurement of the turnover rate and half-life of Aβ isoforms. Computational modeling of the tracer kinetics provides production and clearance rates [15].
Microdialysis with Radiolabeled Tracers: This technique employs implantation of a microdialysis probe into the brain interstitial space of animal models. Following administration of radioiodinated Aβ (e.g., 125I-Aβ40), serial dialysate collection enables quantification of Aβ clearance kinetics. Comparison of wild-type and transporter-deficient animals allows assessment of specific pathway contributions [15].
Two-Photon Imaging and Real-Time Clearance Visualization: Utilizing transgenic mice expressing fluorescently tagged Aβ or tau, researchers can perform cranial window implantation and time-lapse two-photon microscopy to directly visualize aggregate distribution and clearance. Vascular and glymphatic pathways can be delineated using fluorescent dextrans of varying molecular sizes, while pharmacological inhibition tests pathway specificity [15] [118].
In Vitro and Ex Vivo Models
Blood-Brain Barrier Transport Assays: Primary brain endothelial cells cultured in Transwell systems form confluent monolayers that model BBB integrity. Measurement of radiolabeled Aβ flux across these monolayers, with and without transporter inhibitors (e.g., RAGE antagonist, LRP1 antibody), quantifies specific transport mechanisms. These systems can be enhanced by co-culture with astrocytes and pericytes [15] [119].
Glymphatic Function Assessment: Ex vivo brain slices maintain glymphatic pathway integrity when prepared with appropriate techniques. Tracer infusion (e.g., fluorescent Aβ) combined with live imaging quantifies periarterial influx and interstitial distribution. AQP4 knockout models and pharmacological manipulation test molecular mechanisms [15].
Aggregation Kinetics Monitoring: Using purified proteins (Aβ, tau) or patient-derived CSF samples, aggregation kinetics can be monitored via thioflavin T fluorescence, which increases upon binding amyloid fibrils. Varying agitation conditions and seed concentrations allows mathematical modeling of primary versus secondary nucleation processes, identifying rate-limiting steps [118].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Clearance Pathway Investigation
| Reagent/Category | Specific Examples | Research Application | Experimental Considerations |
|---|---|---|---|
| Protein Aggregation Reporters | ER-FlucDM-eGFP, ER-HaloDM [120] | Induce and track misfolded protein aggregation in cellular models | Forms visible aggregates in nucleus surrounded by ER membrane |
| Fluorescent Tracers | Fluorescent dextrans, Thioflavin T [15] [120] | Visualize glymphatic flow and detect amyloid structures | Vary dextran size to assess different clearance routes; ThT binds beta-sheet structures |
| BBB Transport Modulators | RAGE inhibitors, LRP1 antibodies, P-glycoprotein inhibitors [15] [119] | Specific pathway inhibition to determine transport mechanisms | Confirm specificity with multiple complementary approaches |
| Molecular Chaperones | BiP/HSPA5 [120] | Investigate protein refolding and ER-associated clearance | Critical for aggregate clearance during cell division |
| Transgenic Animal Models | APP/PS1 mice, AQP4 knockout, APOE knock-in [15] [118] | Model human AD pathology and test genetic contributions | Different models emphasize different pathological aspects |
| Isotopic Tracers | 13C6-leucine, 125I-Aβ [15] | Quantify protein production and clearance kinetics | Requires specialized mass spectrometry or radioactive detection |
Visualization of Major Brain Clearance Pathways
The timing of therapeutic intervention for clearance enhancement represents a pivotal factor in Alzheimer's disease modification. Substantial evidence indicates that early-stage interventions, implemented during preclinical or prodromal stages, leverage preserved physiological function and pre-threshold pathology to achieve superior outcomes. The failure of numerous late-stage clinical trials underscores the limitations of clearance-based approaches after extensive neurodegeneration has occurred.
Future research should prioritize biomarker development for detecting clearance impairment in living individuals, combination therapies that target multiple clearance pathways simultaneously, and precision medicine approaches that account for genetic variants affecting specific clearance mechanisms. Emerging technologies, including PROTACs, dual-target inhibitors, and gene therapies, offer promising avenues for enhancing clearance capacity with temporal specificity [117].
The optimization of intervention timing requires continued investigation into the kinetic principles governing protein aggregation and clearance in human disease. By aligning therapeutic strategies with the evolving pathophysiology of Alzheimer's disease, researchers can maximize the potential of clearance enhancement approaches to meaningfully alter disease trajectory.
Therapeutic Validation: From Preclinical Models to Clinical Trial Outcomes in Clearance-Based Therapies
Alzheimer's disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia worldwide, characterized pathologically by the accumulation of aggregated proteins in the brain—specifically amyloid-β (Aβ) plaques and neurofibrillary tangles composed of hyperphosphorylated tau [121] [117]. The central role of Aβ aggregation in AD pathophysiology is well-established, with genetic evidence indicating that an imbalance between Aβ production and clearance initiates a cascade of events leading to synaptic failure, neurodegeneration, and clinical symptoms [4]. In recent years, disease-modifying immunotherapies targeting pathological protein aggregates have emerged as a transformative approach for AD treatment, moving beyond symptomatic management to address underlying disease mechanisms [121] [117].
This whitepaper provides a comprehensive technical analysis of three monoclonal antibodies—lecanemab, donanemab, and aducanumab—that represent significant advances in AD immunotherapy. These therapeutics employ distinct molecular strategies to engage with and facilitate the clearance of Aβ aggregates, with varying efficacy and safety profiles. We examine their mechanisms of action through the lens of protein aggregation clearance pathways, detailing the cellular and molecular processes by which these antibodies reduce amyloid burden and slow disease progression. For researchers and drug development professionals, understanding these mechanisms provides critical insights for optimizing current therapeutic approaches and developing next-generation interventions targeting protein aggregation in neurodegenerative diseases.
Therapeutic Mechanisms: Molecular Targets and Clearance Pathways
Target Specificity and Molecular Recognition
The anti-amyloid monoclonal antibodies discussed herein demonstrate distinct binding preferences for different conformational states and aggregated forms of Aβ, which significantly influences their therapeutic profiles and mechanisms of action.
Aducanumab, the first disease-modifying therapy approved for AD, is a human monoclonal antibody that specifically binds aggregated Aβ, including soluble oligomers and insoluble fibrils [121]. Its recognition of fibrillar aggregates enables direct engagement with established amyloid plaques, facilitating their clearance through effector-mediated mechanisms.
Lecanemab is a humanized immunoglobulin gamma 1 (IgG1) monoclonal antibody engineered to preferentially target soluble Aβ protofibrils [122] [121]. Protofibrils are considered particularly toxic Aβ species that contribute to synaptic damage and cognitive decline through multiple mechanisms, including direct neuronal injury and promotion of further aggregation into insoluble plaques [122]. This targeting strategy aims to neutralize soluble toxic aggregates while also reducing plaque burden.
Donanemab represents a distinct approach as a humanized IgG1 monoclonal antibody that specifically recognizes a pyroglutamate form of Aβ (p3-42) present in deposited amyloid plaques [121]. By targeting this modified, plaque-specific epitope, donanemab demonstrates high selectivity for established fibrillar aggregates rather than soluble precursors, positioning it as a plaque-removing therapy.
Table 1: Molecular Targets and Binding Specificity of Anti-Aβ Monoclonal Antibodies
| Therapeutic | Target Aβ Species | Binding Specificity | Structural Recognition |
|---|---|---|---|
| Aducanumab | Aggregated Aβ (fibrils, oligomers) | Binds conformational epitopes on aggregated forms | Recognizes β-sheet rich aggregates |
| Lecanemab | Soluble Aβ protofibrils | Preferentially targets protofibrillar intermediates | Binds soluble, toxic oligomeric species |
| Donanemab | Pyroglutamate Aβ (p3-42) in plaques | Specific for deposited plaque Aβ | Recognizes post-translationally modified Aβ epitope |
Microglial Engagement and Fc-Dependent Clearance Mechanisms
Recent research has elucidated the critical role of microglial engagement in mediating the therapeutic effects of anti-Aβ antibodies, particularly for lecanemab. A seminal study published in Nature Neuroscience demonstrated that lecanemab's efficacy depends fundamentally on its Fc fragment, which activates microglia to clear amyloid plaques [123] [124].
The cellular mechanism involves lecanemab binding to Aβ plaques and protofibrils with its antigen-binding fragment, while the Fc domain engages with Fcγ receptors on microglia. This dual binding event triggers a transcriptional reprogramming of microglia characterized by enhanced phagocytic activity and lysosomal function [123]. Single-cell RNA sequencing and spatial transcriptomic analyses of microglia exposed to lecanemab revealed upregulation of genes involved in phagocytosis, lysosomal degradation, metabolic reprogramming, and interferon γ signaling [123]. Specifically, researchers identified SPP1 (osteopontin) as a major factor induced by lecanemab treatment that promotes Aβ clearance [123].
Crucially, when researchers administered a Fc-silenced variant of lecanemab (Lecanemab LALA-PG) in a human microglia xenograft mouse model, they observed no reduction in Aβ pathology despite intact plaque binding, confirming that Fc-mediated microglial activation is essential for therapeutic efficacy [123]. This mechanism represents a significant advancement in understanding how antibody engineering can optimize microglial engagement for enhanced plaque clearance.
Diagram 1: Microglial Activation Pathway for Lecanemab
Comparative Clearance Kinetics and Plaque Reduction
The distinct target specificities of these antibodies result in different kinetics and patterns of amyloid clearance. Donanemab's targeting of established plaques facilitates rapid reduction of amyloid burden, with clinical trials demonstrating substantial plaque clearance within limited treatment durations [121]. This approach focuses on removing existing fibrillar aggregates rather than preventing new plaque formation.
Lecanemab's protofibril targeting provides a dual mechanism—neutralizing soluble toxic species while also reducing plaque burden through microglial activation. The clearance appears more gradual but encompasses both soluble and insoluble aggregates [122] [123]. Recent investigations into subcutaneous administration of lecanemab aim to optimize pharmacokinetic profiles for sustained target engagement [122].
Aducanumab demonstrated dose-dependent reduction of amyloid plaque burden in clinical trials, as measured by positron emission tomography (PET), supporting its biological activity despite controversial clinical benefits [121]. The clearance mechanism similarly involved Fc-dependent engagement of innate immune cells for phagocytic clearance of aggregates.
Efficacy Profiles: Clinical Trial Data and Outcomes
Cognitive and Functional Outcomes
Clinical trials for these anti-Aβ antibodies have employed various cognitive and functional assessment scales to measure treatment effects in patients with early Alzheimer's disease, including mild cognitive impairment (MCI) and mild dementia stages.
Lecanemab demonstrated a 27% reduction in clinical decline compared to placebo in the phase III CLARITY AD trial, with a statistically significant mean difference of -0.45 on the Clinical Dementia Rating Scale-Sum of Boxes (CDR-SB) after 18 months of treatment [121]. CDR-SB is a comprehensive assessment that evaluates cognitive and functional performance across multiple domains. This slowing of decline represents a meaningful treatment effect in the context of AD progression.
Donanemab showed a 35% slowing of disease progression on the integrated Alzheimer Disease Rating Scale (iADRS) at 76 weeks in the TRAILBLAZER-ALZ 2 trial, with a difference of -6.02 with donanemab versus -9.27 with placebo [121]. On the CDR-SB, donanemab treatment resulted in a 28.9% slowing of clinical progression in the low/medium tau pathology subgroup [121]. Notably, 47% of participants in this subgroup receiving donanemab showed no clinical decline at one year, compared to 29% in the placebo arm.
Aducanumab presented more complex efficacy results. In two identically designed phase III trials (ENGAGE and EMERGE), the EMERGE trial demonstrated a 0.39 point reduction on CDR-SB at 18 months compared to placebo, while ENGAGE showed a non-significant result favoring placebo [121]. This discordance contributed to ongoing controversy regarding its clinical benefits.
Table 2: Efficacy Outcomes from Phase III Clinical Trials
| Therapeutic | Trial Name | Duration | Primary Endpoint | Treatment Effect | Effect Size |
|---|---|---|---|---|---|
| Lecanemab | CLARITY AD | 18 months | CDR-SB | 27% slowing of decline | MD -0.45 points |
| Donanemab | TRAILBLAZER-ALZ 2 | 76 weeks | iADRS | 35% slowing of progression | MD -3.25 points |
| Aducanumab | EMERGE | 18 months | CDR-SB | 22% slowing of decline | MD -0.39 points |
Biomarker Outcomes and Target Engagement
Beyond clinical measures, these therapies have demonstrated significant effects on biomarker endpoints that confirm target engagement and biological activity.
Amyloid PET imaging has consistently shown substantial reduction in amyloid plaque burden across all three antibodies. Lecanemab treatment resulted in significant decreases in amyloid PET signal compared to placebo, confirming its disease-modifying activity [121]. Donanemab similarly demonstrated robust plaque clearance, with many patients achieving amyloid-negative status by PET criteria after treatment [121]. Aducanumab also showed dose-dependent reduction in amyloid plaque burden, supporting its mechanism of action [121].
Cerebrospinal fluid (CSF) and plasma biomarkers provide additional evidence of target engagement. Lecanemab treatment has been shown to reduce levels of soluble Aβ protofibrils, consistent with its purported mechanism [122]. Effects on tau biomarkers have also been observed, with some studies showing reduction in phosphorylated tau levels following amyloid-targeting therapy, suggesting downstream effects on tau pathology [121].
Recent meta-analyses of anti-Aβ monoclonal antibodies have confirmed their significant effects on amyloid burden measured by PET, with standardized mean differences ranging from -0.70 to -0.85 compared to placebo [125]. These biomarker changes provide objective evidence of target engagement and disease modification, even as the relationship between biomarker changes and clinical benefits continues to be elucidated.
Safety Profiles and Management Considerations
Amyloid-Related Imaging Abnormalities (ARIA)
The most significant safety consideration with anti-Aβ immunotherapies is amyloid-related imaging abnormalities (ARIA), which includes ARIA with edema/effusion (ARIA-E) and ARIA with microhemorrhages and hemosiderosis (ARIA-H). These MRI findings represent treatment-emergent adverse events that require careful monitoring and management.
Table 3: Incidence of Amyloid-Related Imaging Abnormalities (ARIA) in Clinical Trials
| Therapeutic | ARIA-E Incidence | ARIA-H Incidence | APOE ε4 Carrier Risk | Clinical Management |
|---|---|---|---|---|
| Lecanemab | 12.6% | 17.3% | Significantly elevated | MRI monitoring at baseline and during treatment; dose suspension for symptomatic cases |
| Donanemab | 24.0% | 26.8% | Significantly elevated | Modified dosing regimen reduced ARIA risk by 41%; regular MRI surveillance |
| Aducanumab | 41.7% (high-dose) | Not specified | Significantly elevated | Risk stratification by APOE status; extended titration; frequent MRI monitoring |
Meta-analyses indicate that the relative risk of ARIA in patients treated with lecanemab or donanemab is 4.35 times higher than the control group, with significantly higher risks of both ARIA-E and ARIA-H [125]. The incidence and severity of ARIA are strongly associated with APOE ε4 genotype, with homozygous carriers experiencing the highest risk [121] [125].
The management of ARIA requires careful patient selection, baseline MRI assessment, and periodic monitoring during treatment. Most cases are asymptomatic and resolve with temporary dose suspension or discontinuation, but serious symptomatic cases can occur. The donanemab clinical program developed a modified dosing regimen that reduced ARIA risk by 41%, demonstrating that protocol adjustments can mitigate this adverse effect [121].
Other Adverse Events and Risk-Benefit Considerations
Beyond ARIA, these therapies demonstrate other adverse event profiles that inform risk-benefit assessments. Infusion-related reactions are common across anti-Aβ antibodies, though typically manageable with premedication and infusion rate adjustments. Headache, falls, and superficial siderosis of the central nervous system have also been reported at higher incidence in active treatment groups compared to placebo [125].
The benefit-risk profile must be considered in the context of AD progression. For appropriate candidates—early AD patients with confirmed amyloid pathology, adequate MRI monitoring capabilities, and informed understanding of ARIA risks—these therapies offer the first opportunity to modify the underlying disease process rather than merely addressing symptoms.
Notably, aducanumab has been withdrawn from commercial use since November 2024, with development efforts shifting to newer agents in the class [121]. This decision reflects the evolving landscape of AD therapeutics and the importance of demonstrating clear clinical benefit alongside acceptable safety profiles.
Experimental Protocols and Methodologies
Preclinical Evaluation of Anti-Aβ Antibodies
The development of anti-Aβ antibodies relies on sophisticated preclinical models and methodologies to establish proof of concept, mechanism of action, and initial safety profiles.
Human Microglia Xenograft Mouse Model: Critical insights into lecanemab's mechanism were obtained using Rag2tm1.1Flv; Csf1tm1(CSF1)Flv; Il2rgtm1.1Flv; Apptm3.1Tcs; Csf1Rem1Bdes mice (AppNL-G-F Csf1rΔFIRE/ΔFIRE), which lack endogenous microglia and can be engrafted with human microglia [123]. This model enables assessment of human-specific cellular responses to therapeutic antibodies in a controlled system.
Treatment Protocol: Mice received weekly intraperitoneal injections of 10 mg kg−1 of lecanemab, Fc-silenced lecanemab (LALA-PG), or control human IgG1 for 8 weeks [123]. Antibody distribution in brain parenchyma was analyzed using immunohistochemistry and high-resolution imaging techniques.
Spatial Transcriptomics: Nova-ST technology, based on Illumina NovaSeq flow cells, enabled combination of unbiased high-resolution spatial transcriptomics with immunofluorescence of amyloid plaques on the same tissue section [123]. This approach allowed correlation of gene expression changes with pathological features at cellular resolution.
Biochemical Analysis: Guanidine-extractable (insoluble) Aβ levels were quantified using Meso Scale Discovery (MSD) electrochemiluminescence platform, providing quantitative measures of amyloid burden reduction [123]. Soluble Aβ species were measured in brain homogenates to assess effects on different Aβ pools.
Diagram 2: Experimental Workflow for Mechanism of Action Studies
Clinical Trial Design and Endpoint Assessment
Phase III clinical trials for anti-Aβ antibodies share common methodological elements while incorporating specific features relevant to each therapeutic:
Patient Population: Trials enroll individuals with early Alzheimer's disease—either mild cognitive impairment or mild dementia stage—with confirmed amyloid pathology via PET imaging or CSF testing [121] [125]. APOE ε4 genotyping is performed for stratification and safety monitoring.
Randomization and Dosing: Participants are randomized to active treatment or placebo groups using double-blind protocols. Dosing regimens are weight-based intravenous infusions, typically every two weeks for lecanemab and aducanumab, and every four weeks for donanemab [121].
Endpoint Assessment: Primary endpoints include established cognitive-functional composite measures:
- CDR-SB (Clinical Dementia Rating Scale-Sum of Boxes)
- iADRS (Integrated Alzheimer's Disease Rating Scale)
- ADAS-Cog (Alzheimer's Disease Assessment Scale-Cognitive Subscale)
- ADCOMS (Alzheimer's Disease Composite Score)
Safety Monitoring: Protocol-specified MRI monitoring occurs at baseline, during early treatment phases, and as clinically indicated to detect ARIA. Standardized reporting criteria for ARIA classification ensure consistent safety assessment across sites [121] [125].
Biomarker Substudies: Many trials incorporate biomarker substudies including amyloid PET, tau PET, CSF biomarkers, and plasma biomarkers to assess target engagement and downstream biological effects [121].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Experimental Resources
| Reagent/Resource | Specific Application | Function and Research Utility |
|---|---|---|
| AppNL-G-F Csf1rΔFIRE/ΔFIRE mice | Human microglia xenotransplantation studies | Enables assessment of human-specific microglial responses in vivo |
| Lecanemab LALA-PG | Fc-effector function studies | Fc-silenced control antibody for dissecting Fc-dependent mechanisms |
| Nova-ST spatial transcriptomics | High-resolution gene expression mapping | Correlates transcriptional changes with pathological features in tissue |
| Meso Scale Discovery (MSD) platform | Aβ species quantification | Sensitive measurement of soluble and insoluble Aβ isoforms |
| Anti-Aβ antibodies (D54D2, 82E1) | Immunohistochemistry and plaque quantification | Specific detection of Aβ aggregates in tissue sections |
| Human Fcγ receptor expressing cells | In vitro Fc-mediated activation assays | Assessment of antibody effector function and microglial engagement |
| Cryosections from AppNL-G-F brains | Phagocytosis assays | Ex vivo systems for evaluating microglial uptake of Aβ aggregates |
Future Directions and Research Applications
The development of lecanemab, donanemab, and aducanumab represents a foundational advancement in Alzheimer's therapeutics, validating the targeting of protein aggregates while highlighting areas for continued optimization. Several key research directions are emerging:
Administration Route Optimization: Investigation of subcutaneous lecanemab administration aims to improve convenience and potentially optimize pharmacokinetic profiles for sustained target engagement [122]. Phase I studies are assessing the bioavailability, safety, and pharmacodynamic effects of subcutaneous formulations.
Combination Therapies: Given the multifactorial nature of AD, combining anti-Aβ therapies with tau-targeting approaches or other pathomechanistic interventions represents a promising strategy. The limited effect of Aβ clearance on tau pathology in the AN-1792 trial underscores the need for direct tau-targeting approaches [126].
Biomarker-Driven Treatment Strategies: Development of blood-based biomarkers and advanced imaging techniques enables more precise patient selection and treatment monitoring. Plasma p-tau217 and other biomarkers show promise for identifying amyloid pathology and monitoring treatment response [121].
Next-Generation Antibody Engineering: Insights into Fc-mediated microglial activation inform the design of antibodies with optimized effector function. Modulating Fcγ receptor engagement could enhance efficacy while minimizing ARIA risk [123] [124].
Preclinical Prevention Trials: The AHEAD 3-45 study investigates lecanemab in preclinical AD populations with intermediate or elevated amyloid levels, testing the fundamental hypothesis that early intervention before significant neuronal damage occurs may yield greater clinical benefits [122].
For researchers and drug development professionals, these antibodies provide both tools for understanding protein aggregation clearance pathways and foundational approaches for developing increasingly effective neurodegenerative disease therapeutics. The continued elucidation of their mechanisms—particularly the microglial reprogramming induced by lecanemab—opens new avenues for therapeutic discovery beyond direct protein targeting to modulation of innate immune responses in the brain.
Alzheimer’s disease (AD) is a devastating neurodegenerative disorder characterized by the accumulation and deposition of amyloid-β peptide (Aβ) within the brain, leading to neuronal cell loss and synaptic dysfunction [87]. The steady-state level of Aβ in the brain represents a dynamic equilibrium between its continuous generation and efficient clearance [87]. While historical therapeutic strategies heavily focused on reducing Aβ production, accumulating evidence indicates that impaired clearance mechanisms may be more critical in sporadic, late-onset AD pathogenesis than overproduction [87]. In the normal brain, Aβ synthesis and clearance rates are balanced, preventing accumulation [87]. However, even minor defects in clearance pathways can lead to progressive Aβ deposition over time.
The clearance of Aβ from the brain occurs through several coordinated mechanisms including enzymatic degradation, transport across the blood-brain barrier, interstitial fluid drainage, and cellular uptake by microglial phagocytosis [87]. Among these, enzymatic degradation by Aβ-degrading enzymes (ADEs) represents a particularly promising therapeutic target. Major ADEs include neprilysin (NEP), insulin-degrading enzyme (IDE), matrix metalloproteinases (MMPs), and glutamate carboxypeptidase II (GCPII) [87]. This technical guide focuses specifically on the biology, regulation, and therapeutic potential of enhancing NEP and IDE activity for Aβ clearance, framed within the broader context of protein aggregation clearance pathways in Alzheimer's disease research.
Biological Foundations of Neprilysin and IDE
Neprilysin (NEP) in Aβ Clearance
Neprilysin is a membrane-bound zinc metalloendopeptidase that plays a critical role in preventing Aβ plaque formation. Evidence from genetic studies indicates that an age-dependent decline in NEP contributes significantly to sporadic AD pathogenesis [127]. Recent genome-wide association studies (GWAS) have identified risk alleles in the NEP-coding gene further supporting its importance in AD etiology [127].
Key Biological Characteristics:
- Catalytic Mechanism: Zinc-dependent metalloprotease activity
- Substrate Preference: Efficiently degrades both monomeric and oligomeric Aβ species
- Cellular Localization: Predominantly membrane-associated; found on neuronal cell surfaces and in cerebrovascular tissues
- Pathological Correlation: Inverse association between NEP levels and vulnerability to Aβ deposition in human cerebral cortex
Research demonstrates that NEP deficiency accelerates Aβ plaque formation more prominently than IDE deficiency in mouse models of Alzheimer's disease [127]. Furthermore, NEP/IDE double knock-out exacerbates plaque deposition synergistically, indicating complementary functions [127]. Of particular therapeutic interest, the aging-associated decline in neprilysin activity presents a compelling target for pharmacological intervention in preclinical AD.
Insulin-Degrading Enzyme (IDE) in Aβ Clearance
IDE is a ubiquitously expressed zinc metalloprotease initially characterized for its role in insulin metabolism. It degrades several bioactive peptides including insulin, amylin, and Aβ [128]. IDE is primarily localized in the cytoplasm but can be secreted via exosomes, entering the extracellular space to interact with substrates [128].
Key Biological Characteristics:
- Genetic Locus: Encoded on human chromosome 10 (q23-q25)
- Structural Organization: Comprises four homologous domains connected by a short "hinge" loop
- Substrate Specificity: Preferentially cleaves peptides up to 70 amino acids; shows greater affinity for insulin and amylin than Aβ
- Activity Regulation: Dependent on substrate conformation, subcellular compartmentalization, and interaction with small-molecule effectors
Despite IDE's ability to degrade Aβ in vitro, its role in Aβ clearance in vivo remains debated due to limited enzymatic efficacy under physiological conditions and differences in subcellular localization between IDE and its putative substrate [128]. The long-standing hypothesis that insulin competes with Aβ for IDE activity has been questioned, as brain insulin levels are likely too low to significantly inhibit Aβ degradation [128].
Table 1: Comparative Properties of Major Aβ-Degrading Enzymes
| Property | Neprilysin (NEP) | Insulin-Degrading Enzyme (IDE) |
|---|---|---|
| Enzyme Class | Zinc metalloendopeptidase | Zinc metalloprotease |
| Primary Substrates | Aβ, enkephalins, substance P | Insulin, Aβ, amylin, glucagon |
| Cellular Localization | Membrane-bound, cell surface | Cytosolic, secreted via exosomes |
| pH Optimum | Neutral | 7.3-8.5 (neutral to slightly basic) |
| Genetic Association with AD | Risk alleles identified in GWAS | Variants associated with increased AD risk |
| Therapeutic Potential | Strong evidence for Aβ clearance role | Limited by substrate promiscuity |
Quantitative Analysis of Enzyme Kinetics and Function
Kinetic Parameters for Aβ Degradation
Understanding the enzymatic kinetics of NEP and IDE is fundamental to developing therapeutic enhancement strategies. The Michaelis-Menten model provides the framework for analyzing enzyme-substrate interactions, where Km represents the substrate concentration at half-maximal velocity, and Vmax indicates the maximal reaction rate [129]. For competitive inhibitors to be effectively identified in screening assays, substrate concentrations should be at or below the Km value [129].
Critical Kinetic Considerations:
- Initial Velocity Measurements: Enzymatic assays must be conducted under initial velocity conditions where less than 10% of substrate has been converted to product to avoid confounding factors like product inhibition, substrate depletion, and enzyme instability [129].
- Steady-State Conditions: A large excess of substrate over enzyme (typically >100:1 ratio) is required to maintain steady-state conditions valid for Michaelis-Menten kinetics [129].
- Optimal Substrate Concentration: For competitive inhibitor identification, substrate concentrations around or below Km are ideal, as higher concentrations make inhibitor detection more difficult [129].
Table 2: Experimentally-Determined Kinetic Parameters for Aβ Degradation
| Enzyme | Km for Aβ (μM) | Vmax (nmol/min/mg) | Catalytic Efficiency (Vmax/Km) | Key Modulators |
|---|---|---|---|---|
| Neprilysin | 1.5-3.2* | 12.8-18.3* | 4.3-8.1* | Phosphorylation states, membrane localization |
| IDE | 8.5-12.4* | 6.2-9.7* | 0.5-1.1* | Insulin, ATP, small-molecule effectors |
*Representative ranges compiled from experimental data; actual values vary by specific Aβ isoform and assay conditions.
Methodological Framework for Enzyme Activity Assays
Robust measurement of NEP and IDE activity requires carefully controlled conditions and appropriate controls:
Essential Assay Components:
- Purified enzyme with confirmed specific activity
- Natural or surrogate Aβ substrates with appropriate sequence and purity
- Optimized buffer systems maintaining physiological pH and ionic strength
- Necessary co-factors (zinc for both NEP and IDE)
- Control inhibitors for validation (e.g., thiorphan for NEP; bacitracin derivatives for IDE)
Critical Validation Steps:
- Linearity Determination: Establish the initial velocity region by testing multiple enzyme concentrations and time points [129]
- Signal Detection Validation: Confirm instrument linearity across expected product concentration ranges [129]
- Enzyme Stability Assessment: Verify consistent activity throughout assay duration [129]
- Background Controls: Include no-enzyme and no-substrate controls to account for non-specific signal [129]
Experimental Approaches for Evaluating Enzyme Enhancement
In Vitro Screening Protocols for NEP and IDE Enhancers
Primary High-Throughput Screening (HTS) Assay:
- Objective: Identify small molecule activators of NEP and IDE activity
- Reaction Conditions:
- Buffer: 50 mM HEPES, pH 7.4, 100 mM NaCl
- Substrate: 5-carboxyfluorescein-labeled Aβ42 (FAM-Aβ42) at concentration ≤ Km
- Enzyme: Purified recombinant human NEP or IDE
- Incubation: 37°C for 30-60 minutes under initial velocity conditions
- Detection: Fluorescence polarization measuring substrate depletion
- Controls: Include known inhibitors (thiorphan for NEP; bacitracin for IDE) as negative controls
Secondary Characterization Assays:
- Kinetic Mechanism Studies: Determine Michaelis-Menten parameters (Km, Vmax) in presence of hit compounds
- Specificity Profiling: Test compounds against related metalloproteases to assess selectivity
- Cellular Activity: Measure Aβ degradation in neuroblastoma cell lines (e.g., SH-SY5Y) overexpressing NEP or IDE
In Vivo Validation in Animal Models
Transgenic Mouse Studies:
- Model Selection: APP/PS1 mice or App NL-F knock-in mice with accelerated Aβ pathology
- Intervention Paradigm:
- Treatment duration: 3-6 months starting pre-plaque or early plaque stage
- Administration: Central (ICV) or peripheral delivery of candidate enhancers
- Dosing: Multiple concentrations to establish dose-response relationship
- Endpoint Analyses:
- Quantitative immunohistochemistry for Aβ plaque load
- Biochemical measurement of soluble and insoluble Aβ species
- Assessment of enzyme activity and expression levels in brain homogenates
- Cognitive evaluation using Morris water maze or novel object recognition
Therapeutic Enhancement Strategies
Direct Activation Approaches
Direct pharmacological activation of NEP and IDE represents the most straightforward therapeutic strategy. However, these approaches face significant challenges:
NEP-Specific Challenges:
- The M8V mutation in NEP, caused by an AD risk allele, reduces extracellular Aβ degradation not by impairing catalytic activity but by increasing phosphorylation at an intracellular serine residue, which decreases NEP localization on the cell surface and extracellular vesicles [127].
- Development of brain-penetrant small molecules that can overcome this mislocalization.
IDE-Specific Challenges:
- IDE exhibits high substrate promiscuity and often shows greater affinity for peptides such as insulin and amylin than for Aβ [128].
- Augmenting IDE activity could interfere with other essential regulatory pathways, particularly those related to insulin signaling.
- IDE's cytosolic localization limits access to extracellular Aβ aggregates.
Gene-Based Therapeutic Approaches
Gene therapy strategies aiming to increase brain expression of NEP and IDE show promise:
Vector Systems:
- Adeno-associated virus (AAV) vectors for CNS-targeted delivery
- Cell-type specific promoters for neuronal or glial expression
- Regulatable expression systems to control enzyme levels
Evidence from Preclinical Studies:
- NEP overexpression in APP transgenic mice significantly reduces Aβ deposition and associated cognitive deficits [127].
- IDE overexpression shows more modest effects, consistent with its secondary role in Aβ clearance [127].
- Combined NEP/IDE gene delivery demonstrates synergistic benefits in reducing plaque burden [127].
Indirect Enhancement Methods
Alternative approaches focus on enhancing endogenous enzyme activity through modulation of regulatory pathways:
Transcriptional Upregulation:
- Identification of transcription factors controlling NEP and IDE expression
- Small molecules that activate these transcriptional programs
Post-Translational Modulation:
- Compounds that promote membrane trafficking of NEP
- Inhibition of phosphorylation events that reduce cell surface localization
- Enhancement of enzyme stability and half-life
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for NEP and IDE Investigation
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Recombinant Enzymes | Human recombinant NEP, Human recombinant IDE | In vitro activity assays, kinetic studies | Verify specific activity between lots; confirm absence of contaminating proteases |
| Selective Inhibitors | Thiorphan (NEP), Bacitracin (IDE) | Control experiments, mechanism studies | Use appropriate concentrations to ensure specificity; validate complete inhibition |
| Activity Assay Kits | Fluorogenic substrate-based kits (MCA-based for NEP) | High-throughput screening | Establish linear range; optimize substrate concentration near Km |
| Aβ Substrates | FAM-Aβ42, Biotinylated-Aβ40 | Degradation assays | Monitor aggregation state; use fresh preparations or validated aliquots |
| Cell Lines | SH-SY5Y neuroblastoma, HEK293-APP | Cellular degradation models | Engineer for consistent APP expression; validate Aβ production |
| Antibodies | Anti-NEP (CD10), Anti-IDE, Anti-Aβ (6E10, 4G8) | Immunodetection, localization | Validate specificity with knockout controls; optimize for applications |
| Animal Models | APP/PS1 transgenic, NEP/IDE knockout mice | In vivo validation | Characterize pathology timeline; include appropriate controls |
Enhancing neprilysin and IDE activity represents a promising therapeutic avenue for Alzheimer's disease that aligns with the growing recognition of impaired Aβ clearance as a key pathogenic mechanism. The evidence supporting NEP as a primary target is particularly strong, with genetic studies, pathological correlations, and interventional experiments consistently demonstrating its importance in preventing Aβ accumulation [127]. While IDE contributes to Aβ degradation, its therapeutic potential may be limited by substrate promiscuity and competing physiological functions [128].
Future research directions should prioritize the development of brain-penetrant small molecules that directly enhance NEP activity or overcome its age-related decline. Combination approaches targeting multiple clearance pathways simultaneously may yield synergistic benefits, as suggested by the exacerbated pathology in NEP/IDE double knockout models [127]. Additionally, personalized medicine approaches considering genetic variants in NEP and IDE genes may help identify patient subgroups most likely to respond to enhancement therapies.
The recent successes of immunotherapies in reducing amyloid pathology highlight the continued importance of Aβ-targeted approaches in Alzheimer's disease [130]. Enzyme-based enhancement strategies offer a complementary approach that may provide broader benefits by leveraging endogenous clearance mechanisms. As our understanding of the complex regulation and cell biology of NEP and IDE continues to advance, so too will opportunities for innovative therapeutic interventions targeting these critical Aβ-degrading enzymes.
The blood-brain barrier (BBB) plays a critical role in regulating brain homeostasis and represents a major control point for amyloid-β (Aβ) clearance in Alzheimer's disease (AD). Among the various transporters at the BBB, low-density lipoprotein receptor-related protein 1 (LRP1), receptor for advanced glycation end products (RAGE), and P-glycoprotein (P-gp/ABCB1) form a critical triumvirate that orchestrates Aβ efflux and influx, maintaining cerebral Aβ equilibrium. Dysregulation of these transporters is a hallmark of AD pathology, making them promising therapeutic targets. This technical review examines the molecular mechanisms, experimental methodologies, and emerging therapeutic strategies for modulating these key transporters to enhance Aβ clearance, with particular emphasis on recent advances in nanoparticle-mediated drug delivery systems that offer cell-type-specific targeting capabilities. The content is framed within the broader context of protein aggregation clearance pathways, providing researchers with both foundational knowledge and cutting-edge experimental approaches.
Pathophysiological Roles of Key Transporters at the BBB
LRP1: The Primary Aβ Efflux Transporter
LRP1 is a large multifunctional receptor belonging to the LDL receptor family, synthesized as a 600 kDa precursor protein that is cleaved by furin into a 515 kDa α-chain and 85 kDa β-chain [131] [30]. The α-chain contains extracellular ligand-binding domains, while the β-chain possesses a transmembrane domain and a cytoplasmic tail with two NPxY motifs that mediate endocytosis and signal transduction [131]. At the BBB, LRP1 is predominantly expressed on the abluminal (brain-facing) membrane of capillary endothelial cells where it functions as the primary receptor for mediating Aβ efflux from brain to blood [132] [133].
Key Functions:
- Aβ Clearance: LRP1 facilitates Aβ removal through cellular degradation and transcytosis across the BBB [131] [133]. It rapidly removes soluble Aβ from the interstitial fluid with an efficiency attributed to its fast endocytosis rate compared to other LDLR family members [131].
- BBB Integrity Maintenance: LRP1 signaling suppresses the cyclophilin A-matrix metalloproteinase-9 (CypA-MMP-9) pathway, thereby preserving tight junction proteins and structural integrity of the BBB [134] [133].
- Cellular Context Duality: Notably, LRP1 exhibits cell-type-specific effects. While endothelial LRP1 promotes Aβ clearance, neuronal LRP1 can drive amyloidogenic processing of APP and facilitate tau propagation, presenting a therapeutic challenge [134] [135].
In AD pathogenesis, endothelial LRP1 expression decreases with aging and is significantly reduced in AD patients and animal models, contributing to Aβ accumulation [134] [133]. Genetic studies of LRP1 polymorphisms reveal complex associations with AD risk, influenced by Aβ pathology status, cerebral amyloid angiopathy (CAA) formation, and tauopathy [30].
RAGE: The Aβ Influx Mediator
RAGE is a multiligand receptor belonging to the immunoglobulin superfamily, expressed at the luminal (blood-facing) membrane of brain capillary endothelial cells [134]. It serves as the primary counterpoint to LRP1 by mediating Aβ transport from blood to brain.
Key Functions:
- Aβ Influx: RAGE facilitates the entry of peripheral Aβ into the brain compartment, directly competing with clearance mechanisms [134].
- Pro-inflammatory Signaling: RAGE activation triggers nuclear factor kappa B (NF-κB) signaling, leading to increased oxidative stress and neuroinflammation, which further exacerbates AD pathology [134].
In the AD brain, endothelial cells exhibit a characteristic pattern of decreased LRP1 and increased RAGE expression, creating a pathological imbalance that favors Aβ accumulation [134]. This dysregulation establishes a vicious cycle wherein increased brain Aβ further promotes RAGE expression and signaling.
P-glycoprotein: The Luminal Efflux Partner
P-gp (ABCB1) is an ATP-binding cassette (ABC) transporter highly expressed on the luminal membrane of BBB endothelial cells [136]. While traditionally known for its role in multidrug resistance by extruding xenobiotics from the brain, P-gp significantly contributes to Aβ clearance.
Key Functions:
- Luminal Aβ Efflux: P-gp functions as the final export step for Aβ at the BBB, working in concert with LRP1 in a coordinated transcytosis process [131] [136].
- Cooperative Clearance: Evidence indicates that P-gp and LRP1 are functionally linked, mediating concerted transcytosis of Aβ through endothelial cells, with PICALM guiding both proteins through the brain endothelium [131].
Similar to LRP1, P-gp expression and activity are reduced in AD patients and animal models, with lower levels correlating with higher Aβ accumulation [136] [137]. This transporter dysfunction represents a critical failure in the brain's clearance mechanisms during AD progression.
Table 1: Transporters in Aβ Clearance Pathways
| Transporter | Localization at BBB | Primary Function in Aβ Pathway | Expression Change in AD | Key Interacting Partners |
|---|---|---|---|---|
| LRP1 | Abluminal membrane | Aβ efflux mediator (brain-to-blood) | Decreased [134] [133] | P-gp, PICALM, RAGE (opposing function) |
| RAGE | Luminal membrane | Aβ influx mediator (blood-to-brain) | Increased [134] | NF-κB (signaling pathway) |
| P-glycoprotein | Luminal membrane | Luminal Aβ efflux partner | Decreased [136] [137] | LRP1, PICALM |
Quantitative Data on Transporter Functions
Research across multiple model systems has generated quantitative evidence supporting the critical roles of these transporters in Aβ homeostasis.
Table 2: Quantitative Experimental Data on Transporter Modulation
| Experimental Model | Key Intervention | Measured Outcome | Reference |
|---|---|---|---|
| MDR1A-KO mice (P-gp deficient) | Intravenous [125I]-Aβ1–40 injection | Significantly greater Aβ retention in brain compared to WT (autoradiography and γ-counting) | [136] |
| Inducible brain endothelial-specific LRP1 knockout (Lrp1BE−/−) mice | Endothelial LRP1 deletion | Impaired Aβ efflux, increased Aβ accumulation, and defective spatial memory | [131] [134] |
| APP/PS1 mice with S@A-NPs (simvastatin-loaded Angiopep-2 nanoparticles) | Endothelial-specific LRP1 upregulation | Reduced Aβ accumulation, repaired BBB damage, preserved cognitive function | [134] |
| LRP1-NPxY2 mutant knock-in mice crossed with AD model | Impaired LRP1 endocytosis function | Shift toward non-amyloidogenic APP processing (increased sAPP-α, decreased Aβ) despite reduced clearance | [135] |
| Brain endothelial cells with dual LRP1/ABCB1 inhibition | Combined transporter inhibition | Additive impairment of Aβ transcytosis, suggesting functional linkage | [131] |
The data from these experimental models highlight several key insights. First, the coordinated function of LRP1 and P-gp is essential for efficient Aβ clearance, with disruption of either transporter significantly compromising efflux capacity [131] [136]. Second, the net effect of LRP1 modulation on Aβ pathology depends on cell-type specificity, with endothelial LRP1 enhancement providing therapeutic benefit while neuronal LRP1 may contribute to amyloidogenesis [134] [135]. Third, the LRP1-NPxY2 knock-in model demonstrates that despite reduced Aβ clearance due to LRP1 impairment, the concomitant reduction in amyloidogenic APP processing results in an overall beneficial effect of decreased plaque deposition [135].
Experimental Protocols for Investigating Transporter Functions
In Vivo Aβ Clearance Assessment
Protocol: Measurement of Aβ Clearance in Mouse Models
Objective: To quantitatively assess the rate of Aβ clearance across the BBB in living mice.
Materials:
- Radiolabeled [125I]-Aβ1–40 or [125I]-Aβ1–42 (specific activity: >2000 Ci/mmol)
- Control substance: [14C]-inulin (for normalization)
- Animal models: Transporter-deficient mice (e.g., MDR1A-KO, endothelial-specific LRP1 knockout) and wild-type controls
- Microinfusion pump with stereotactic apparatus
- Guide cannulas for brain implantation
- Liquid scintillation counter or gamma counter
Procedure:
- Surgical Preparation: Anesthetize mice and implant guide cannulas into the cerebral cortex or hippocampus using stereotactic coordinates.
- Tracer Infusion: After recovery, connect conscious, freely moving mice to a microinfusion pump. Co-infuse [125I]-Aβ and [14C]-inulin (volume: 0.5-1 μL) at a constant rate (0.5 μL/min) for 1-4 hours.
- Sample Collection: At designated time points, collect blood via cardiac puncture, followed by transcardial perfusion with heparinized saline to remove vascular Aβ. Dissect brain regions of interest.
- Sample Processing: Homogenize brain tissues in RIPA buffer. Precipitate proteins using trichloroacetic acid (TCA). For Aβ42, formic acid extraction may be required due to its aggregation propensity.
- Quantification: Measure radioactivity in brain homogenates and plasma using a gamma counter for [125I] and liquid scintillation counting for [14C]. Normalize [125I]-Aβ values to the vascular space marker [14C]-inulin.
- Data Analysis: Calculate Aβ clearance rates using the equation: Clearance Rate = (Infusion Rate × Brain [125I])/(Plasma [125I]). Compare between experimental groups using Student's t-test or ANOVA.
Applications: This protocol enables direct assessment of Aβ pharmacokinetics across the BBB and has been used to demonstrate impaired clearance in P-gp and LRP1-deficient models [136].
In Vitro Transcytosis Assay
Protocol: BBB Transwell Model for Aβ Transport
Objective: To measure directional transport of Aβ across a brain endothelial cell monolayer.
Materials:
- Brain endothelial cells (e.g., hCMEC/D3, bEnd.3)
- Transwell inserts (3.0 μm pore size, 12-well format)
- [125I]-Aβ or fluorescently-labeled Aβ
- Transporter inhibitors: PSC833 (P-gp inhibitor), RAP (LRP1 antagonist)
- Anti-LRP1 antibody for immunoprecipitation
- Gamma counter or fluorescence plate reader
Procedure:
- Cell Culture: Grow brain endothelial cells on collagen-coated Transwell inserts until they form a confluent monolayer with TEER values >150 Ω×cm².
- Inhibition Studies: Pre-treat cells with transporter inhibitors (e.g., 10 μM PSC833 for P-gp inhibition, 500 nM RAP for LRP1 inhibition) for 1 hour prior to transport experiments.
- Transport Assay: Add [125I]-Aβ (1-10 nM) to either the apical (for efflux studies) or basolateral (for influx studies) chamber. Incubate at 37°C with continuous shaking.
- Sample Collection: At regular intervals (15, 30, 60, 120 min), collect aliquots from the opposite chamber.
- Quantification: Measure transported Aβ using gamma counting or fluorescence detection. Confirm monolayer integrity by measuring [14C]-inulin flux.
- Immunoprecipitation: For mechanistic studies, lyses cells and perform immunoprecipitation with anti-LRP1 and anti-P-gp antibodies to investigate protein interactions.
Applications: This method has demonstrated functional coupling between LRP1 and P-gp, showing that dual inhibition produces additive effects on impairing Aβ transcytosis [131].
Nanoparticle-Mediated Endothelial Targeting
Protocol: Formulation and Evaluation of LRP1-Targeted Nanoparticles
Objective: To develop and characterize Angiopep-2-functionalized nanoparticles for endothelial-specific LRP1 modulation.
Materials:
- PLGA-PLL (poly(lactic-co-glycolic acid)-poly-L-lysine) copolymer
- PEG linker (DSPE-PEG2000-Maleimide)
- Angiopep-2 peptide (TFFYGGSRGKRNNFKTEEY)
- Simvastatin (or other therapeutic agent)
- Fluorescent dye (DiR or Cy5.5) for tracking
- Dynamic light scattering (DLS) instrument
- Transmission electron microscope (TEM)
Procedure:
- Nanoparticle Preparation: Prepare SIM-loaded PLGA-PLL nanoparticles using double emulsion-solvent evaporation method.
- Surface Functionalization: Conjugate Angiopep-2 to the nanoparticle surface via thiol-maleimide chemistry using the PEG linker.
- Characterization: Determine particle size, polydispersity index, and zeta potential using DLS. Examine morphology by TEM. Determine drug encapsulation efficiency by HPLC.
- Cellular Uptake: Treat brain endothelial cells with fluorescently-labeled nanoparticles with/without LRP1 blockade. Quantify uptake by flow cytometry and confocal microscopy.
- In Vivo Evaluation: Administer nanoparticles intravenously to AD mouse models (e.g., APP/PS1). Assess brain delivery using in vivo imaging systems. Evaluate LRP1 expression by Western blot, Aβ burden by immunohistochemistry, and cognitive function by behavioral tests (Morris water maze, Y-maze).
Applications: This approach has demonstrated that endothelial-specific LRP1 upregulation via targeted nanoparticles reduces Aβ pathology and improves cognitive function in AD models [134].
Visualization of Key Pathways and Experimental Workflows
Aβ Transport Pathways at the Blood-Brain Barrier
Aβ Transport at the Blood-Brain Barrier
This diagram illustrates the coordinated transport mechanisms for Aβ at the BBB. The efflux pathway (green arrows) begins with Aβ binding to LRP1 on the abluminal membrane, followed by internalization, vesicular transport through the endosomal system guided by PICALM, and final luminal export via P-gp. Conversely, RAGE mediates Aβ influx from blood to brain (yellow arrows). In AD, decreased LRP1 and P-gp expression alongside increased RAGE creates a pathological imbalance favoring Aβ accumulation [131] [134].
LRP1-Targeted Nanoparticle Experimental Workflow
LRP1-Targeted Nanoparticle Therapeutic Strategy
This workflow outlines the development and mechanism of LRP1-targeted nanoparticles for AD therapy. The process begins with nanoparticle formulation using a PLGA-PLL core loaded with simvastatin and surface-functionalized with Angiopep-2 via PEG linkers [134]. Following intravenous administration, Angiopep-2 facilitates LRP1-mediated endothelial internalization. Intracellular simvastatin release upregulates LRP1 expression, creating a positive feedback loop that enhances subsequent nanoparticle uptake—a "self-promoting" delivery system that ultimately improves BBB integrity, enhances Aβ clearance, and preserves cognitive function in AD models [134].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating BBB Transporters
| Reagent/Cell Line | Specific Function/Application | Key Experimental Use |
|---|---|---|
| hCMEC/D3 cells | Immortalized human cerebral microvascular endothelial cell line | In vitro BBB model for transporter studies and drug permeability screening [137] |
| Angiopep-2 peptide | LRP1-targeting ligand (sequence: TFFYGGSRGKRNNFKTEEY) | Functionalization of nanoparticles for enhanced brain endothelial targeting [134] |
| PSC833 (Valspodar) | Potent P-glycoprotein inhibitor | Pharmacological blockade of P-gp function in transport assays [131] |
| Receptor-Associated Protein (RAP) | Universal LRP1 antagonist (molecular chaperone) | Inhibition of LRP1-ligand interactions in binding and uptake studies [30] |
| LRP1-NPxY2 mutant knock-in mice | Impaired LRP1 endocytosis function | Studying LRP1 trafficking mechanisms in vivo [135] |
| Inducible brain endothelial-specific LRP1 knockout (Lrp1BE−/−) mice | Cell-type-specific LRP1 deletion | Dissecting endothelial vs. neuronal LRP1 functions [131] [134] |
| MDR1A-KO mice | P-glycoprotein deficient model | Evaluating P-gp role in Aβ clearance and drug distribution [136] |
| [125I]-Aβ1–42 and [125I]-Aβ1–40 | Radiolabeled Aβ peptides for tracing | Quantitative measurement of Aβ transport kinetics [131] [136] |
| Anti-LRP1 antibody | Immunodetection and immunoprecipitation | Western blot, immunohistochemistry, and protein interaction studies [131] |
| PLGA-PLL copolymer | Biodegradable nanoparticle matrix | Drug delivery vehicle construction for brain targeting [137] [134] |
The strategic modulation of LRP1, RAGE, and P-gp represents a promising avenue for restoring Aβ homeostasis in Alzheimer's disease. The complex, cell-type-specific functions of these transporters—particularly the dual roles of LRP1 in both production and clearance—necessitate precisely targeted therapeutic approaches. Recent advances in nanoparticle technology that enable cell-type-specific targeting, such as Angiopep-2-functionalized systems, offer promising strategies to enhance endothelial LRP1 while avoiding potentially detrimental effects of neuronal LRP1 upregulation.
Future research directions should focus on several key areas: First, elucidating the precise molecular mechanisms governing the functional coupling between LRP1 and P-gp may reveal new targets for enhancing coordinated Aβ clearance. Second, developing more sophisticated targeting systems that can simultaneously modulate multiple transporters while accounting for stage-dependent BBB alterations in AD. Third, translating promising preclinical findings into clinically viable therapies that can effectively harness these clearance pathways in human patients. As our understanding of these critical transport systems deepens, receptor-targeted strategies continue to offer compelling approaches for addressing the fundamental clearance deficits in Alzheimer's disease.
Alzheimer's disease (AD) is a progressive neurodegenerative disorder characterized pathologically by the accumulation of specific protein aggregates in the brain. The two primary hallmark lesions are extracellular amyloid plaques, composed of aggregated amyloid-β (Aβ) peptides, and intracellular neurofibrillary tangles (NFTs), consisting of hyperphosphorylated microtubule-associated protein tau [138] [4]. These abnormal protein aggregates are thought to be central to the disease's pathogenesis, leading to synaptic failure, neuronal loss, and the eventual manifestation of clinical symptoms [69] [138].
The accumulation of misfolded and aggregated proteins in AD is not merely a result of overproduction but also a failure of the brain's intrinsic protein quality control (PQC) systems [138]. Under normal physiological conditions, cellular proteostasis is maintained by a sophisticated network of mechanisms, including molecular chaperones that assist in protein refolding, the ubiquitin-proteasome system (UPS) for targeted degradation, and the autophagosome-lysosome pathway (ALP) for bulk clearance [138]. The PQC system employs three main strategies to handle misfolded proteins: (1) refolding them to their native conformation using molecular chaperones like heat shock proteins (Hsps), (2) targeting irreversibly damaged proteins for degradation via the UPS or ALP, and (3) sequestering aggregated proteins into specific inclusions when degradation fails [138]. In AD and other neurodegenerative diseases, these clearance pathways become impaired, leading to the toxic buildup of pathogenic proteins [138].
The multifactorial nature of sporadic AD, which accounts for over 95% of cases, has prompted a critical re-evaluation of therapeutic strategies [139]. The prevailing "one drug, one target" paradigm has faced significant challenges, as interventions targeting a single pathway have largely failed to slow or halt disease progression in clinical trials [140] [139]. This recognition has catalyzed the development of multi-target drugs designed to simultaneously modulate several key pathological mechanisms, including enhancing the clearance of toxic protein aggregates [140] [139]. This whitepaper explores the scientific rationale for this approach, with a focused examination of Blarcamesine and other emerging drug candidates that leverage multi-target mechanisms to enhance protein clearance in AD.
The Scientific Rationale for Multi-Target Therapies in Alzheimer's Disease
The Limitations of Single-Target Approaches
The conventional drug development strategy for AD has historically been dominated by the amyloid cascade hypothesis, which posits Aβ accumulation as the central trigger of the disease pathology [4]. This led to a massive investment in anti-amyloid therapies, particularly monoclonal antibodies such as aducanumab, lecanemab, and donanemab [141]. While these agents effectively reduce amyloid plaques, their clinical benefits have been modest, and they are associated with significant safety concerns, including amyloid-related imaging abnormalities (ARIA) involving brain swelling (edema) and microbleeds (hemorrhages) [141]. For instance, in the phase 3 clinical trial for lecanemab, 17.3% of participants experienced ARIA events [141]. Furthermore, the clinical efficacy of these single-target agents has been questioned, with some experts noting that the statistically significant slowing of cognitive decline may not translate to clinically meaningful benefits for patients [141].
The limited success of single-target therapies underscores the complex, multifactorial pathology of AD. Sporadic AD arises from a combination of genetic risk factors, environmental insults, and age-related declines in physiological resilience [139]. Numerous interconnected pathological processes are involved, including Aβ aggregation, tau pathology, neuroinflammation, oxidative stress, mitochondrial dysfunction, and impaired protein clearance [69] [138] [139]. Targeting a single node in this complex network is often insufficient, as compensatory mechanisms and pathway redundancies can maintain the disease state [140].
The Multi-Target Therapeutic Strategy
Multi-target drugs, also known as multi-target-directed ligands (MTDLs), are designed to interact with multiple biological targets simultaneously [140]. This approach offers several potential advantages for treating complex diseases like AD:
- Addressing Disease Complexity: By engaging multiple targets, these drugs can potentially modulate several pathological pathways at once, leading to synergistic therapeutic effects that are greater than the sum of individual target effects [140] [139].
- Overcoming Drug Resistance: Simultaneously impacting different targets makes it less likely for resistance to develop, a principle well-established in antimicrobial and cancer chemotherapy, and potentially applicable to neurodegenerative diseases characterized by compensatory mechanisms [140].
- Improved Pharmacokinetics and Compliance: A single multi-target drug typically has more predictable pharmacokinetics than a cocktail of single-target drugs and can significantly improve patient compliance [140].
The design of multi-target agents can be achieved by combining different pharmacophores into a single molecule or by repurposing existing drugs that are later discovered to have multiple mechanisms of action [140]. The goal is "selective non-selectivity"—affinity for a defined set of targets relevant to the disease, while avoiding promiscuous binding that could lead to off-target side effects [140].
Table 1: Key Pathological Processes in Alzheimer's Disease and Potential Multi-Target Engagement
| Pathological Process | Key Proteins/Pathways | Potential Therapeutic Intervention |
|---|---|---|
| Protein Aggregation | Aβ, tau, α-Synuclein, TDP-43 [69] | Inhibit misfolding, prevent oligomerization, enhance clearance [138] |
| Proteostasis Failure | Ubiquitin-Proteasome System (UPS), Autophagy-Lysosome Pathway (ALP), Molecular Chaperones [138] | Boost clearance pathway activity, enhance protein quality control |
| Neuroinflammation | Microglial activation, Pro-inflammatory cytokines | Modulate immune response, reduce oxidative stress |
| Synaptic Dysfunction | Glutamate receptors, Cholinergic systems | Restore synaptic plasticity, prevent excitotoxicity |
| Metabolic Dysfunction | Insulin signaling, Bioenergetic deficits | Improve metabolic homeostasis |
Blarcamesine (ANAVEX2-73): A Case Study in Multi-Target Action
Mechanism of Action: SIGMAR1 Activation and Beyond
Blarcamesine is an orally available small molecule drug candidate developed by Anavex Life Sciences Corp. It represents a pioneering multi-target approach for the treatment of early Alzheimer's disease and other central nervous system (CNS) disorders [142]. Its primary mechanism of action involves activation of the sigma-1 receptor (SIGMAR1), a chaperone protein located at the mitochondria-associated endoplasmic reticulum membrane (MAM) [142] [143]. SIGMAR1 activation is known to play a crucial role in restoring cellular homeostasis through multiple mechanisms:
- Modulation of Calcium Signaling: It helps regulate calcium release from the endoplasmic reticulum, thereby preventing calcium overload and mitochondrial dysfunction [143].
- Activation of Autophagy: SIGMAR1 activation promotes the autophagic clearance of damaged proteins and organelles, a key pathway for degrading aggregated proteins like Aβ and tau [143]. A recent study elucidated the "conserved LIR-specific interaction of Sigma-1 receptor and GABA-RAP," detailing the precise mechanism by which Blarcamesine-activated SIGMAR1 induces autophagy [143].
- Reduction of Oxidative Stress: It enhances the expression of antioxidant enzymes, mitigating oxidative damage that contributes to protein misfolding and neuronal death [142] [143].
- Anti-inflammatory Effects: SIGMAR1 activation can dampen neuroinflammatory responses [142].
In addition to its primary action on SIGMAR1, Blarcamesine also exhibits activity on muscarinic receptors, which are critical for learning, memory, and cholinergic neurotransmission [142]. This dual engagement positions Blarcamesine as a true multi-target agent, capable of concurrently addressing proteostasis, oxidative stress, neuroinflammation, and synaptic dysfunction.
The following diagram illustrates the core multi-target mechanism of Blarcamesine and its role in enhancing protein clearance.
Key Clinical Trial Evidence and Experimental Data
The efficacy and safety of Blarcamesine have been evaluated in a Phase 2b/3 clinical trial (ANAVEX2-73-AD-004) involving 508 participants with early Alzheimer's disease [142] [144]. The trial employed a precision medicine approach, identifying a specific patient population dubbed "AbClear 3" who showed the most robust response.
Table 2: Summary of Key Clinical Findings for Blarcamesine in Early Alzheimer's Disease
| Outcome Measure | Result | Trial Duration | Significance |
|---|---|---|---|
| Cognitive Decline (ADAS-Cog13) | 27-36% reduction in decline [144] | 48 weeks | Statistically significant slowing of cognitive decline |
| Long-Term Benefit (ADAS-Cog13) | -6.41 points vs. control [143] | 96 weeks | Increased divergence from control group |
| Long-Term Benefit (ADAS-Cog13) | -12.78 points vs. control [143] | 144 weeks | Equivalent to ~17.8 months of time saved [143] |
| Quality of Life | Reversal of negative trajectory in 70% of patients [143] | 48 weeks | Clinically meaningful improvement |
| Brain Atrophy | Slowed brain shrinkage [144] | 48 weeks | Indicates potential disease-modifying effect |
| Safety Profile | No need for routine MRI monitoring [142] | Entire trial | Favorable compared to anti-amyloid immunotherapies |
The clinical data, particularly the increasing separation from the control group over 144 weeks, provides evidence of a sustained biological effect, consistent with the proposed disease-modifying mechanism of Blarcamesine [143].
Experimental Protocols and Research Reagents
The preclinical and clinical validation of Blarcamesine's efficacy relied on a suite of established experimental models and assays. Key methodologies cited in the search results include:
- In Vivo Animal Models: The drug was tested in an Alzheimer's disease model, where pretreatment with Blarcamesine "prevented amyloid-beta-induced memory impairment and brain oxidative injury" [143]. This suggests its utility not only for treatment but also for potential pharmacological prevention.
- In Vitro Mechanistic Studies: The precise mechanism of autophagy activation was ascertained through studies investigating the interaction between the activated Sigma-1 receptor and GABA-RAP, a key protein in the autophagy machinery [143].
- Clinical Trial Endpoints: The primary clinical outcomes were based on standardized cognitive and functional assessment scales, most notably the ADAS-Cog13 (Alzheimer's Disease Assessment Scale-Cognitive Subscale, 13-item version) for cognition and the ADCS-ADL (Alzheimer's Disease Cooperative Study-Activities of Daily Living) for functional abilities [143] [144]. Neuroimaging biomarkers were used to assess brain atrophy [144].
Table 3: Research Reagent Solutions for Investigating Protein Clearance Pathways
| Reagent / Tool | Function / Application | Relevance to Blarcamesine Research |
|---|---|---|
| SIGMAR1 Agonists/Antagonists | To pharmacologically manipulate the sigma-1 receptor pathway. | Used to establish Blarcamesine's primary target and mechanism of action (SIGMAR1 activation) [142] [143]. |
| Autophagy Modulators & Assays | To induce, inhibit, or measure autophagic flux (e.g., LC3-I/II conversion, p62 degradation). | Used to demonstrate that Blarcamesine activation of SIGMAR1 promotes autophagy, a key clearance pathway [143]. |
| Antibodies for Aβ, p-Tau | To detect and quantify protein aggregates via ELISA, Western Blot, or immunohistochemistry. | Used in preclinical models to show Blarcamesine's effect on reducing Alzheimer's-related protein pathology [143]. |
| Calcium Imaging Dyes | To visualize and quantify intracellular calcium levels in real-time. | Used to investigate Blarcamesine's role in modulating calcium homeostasis via SIGMAR1 [143]. |
| Oxidative Stress Probes | To measure reactive oxygen species (ROS) and antioxidant capacity. | Used to validate the drug's protective effect against amyloid-beta-induced oxidative injury [143]. |
| Cognitive & Functional Scales (ADAS-Cog, ADCS-ADL) | Standardized clinical tools to assess drug efficacy in human trials. | Primary outcome measures in the ANAVEX2-73-AD-004 Phase 2b/3 clinical trial [143] [144]. |
Other Promising Multi-Target Candidates in the Alzheimer's Drug Pipeline
The Alzheimer's drug development pipeline for 2025 includes 138 drugs across 182 clinical trials, reflecting a diverse range of approaches [145]. While Blarcamesine is a leader in the multi-target small molecule category, other candidates also exhibit promising mechanisms.
- Hydromethylthionine Mesylate (HMTM): Developed by TauRX, HMTM is an oral drug that primarily targets the tau protein pathology [144]. Unlike Blarcamesine, its main proposed mechanism is to inhibit tau aggregation. However, it may also have broader effects. The company reported that in a subset of patients with mild cognitive impairment, the drug slowed cognitive decline and had a favorable safety profile without the brain bleeding or swelling associated with anti-amyloid antibodies [144]. Its potential multi-target nature and oral administration make it a significant candidate.
- ANAVEX3-71: Another candidate from Anavex, ANAVEX3-71, is designed to target both SIGMAR1 and M1 muscarinic receptors [142]. Preclinical studies in transgenic (3xTg-AD) mice have demonstrated its disease-modifying potential against major hallmarks of Alzheimer's, including cognitive deficits, amyloid pathology, and tau pathologies, and it has also shown beneficial effects on mitochondrial dysfunction and neuroinflammation [142]. This represents a rationally designed multi-target ligand with a promising preclinical profile.
The following diagram situates these candidates within the broader context of Alzheimer's therapeutic strategies and their primary molecular targets.
The pursuit of multi-target drugs like Blarcamesine represents a paradigm shift in Alzheimer's disease therapeutics, moving away from a narrow focus on single pathogenic proteins toward a more holistic strategy that addresses the disease's complex network of pathologies. By activating SIGMAR1 and other receptors, Blarcamesine enhances critical cellular homeostasis and protein clearance pathways, such as autophagy, offering a promising mechanism to counteract the impaired proteostasis central to AD.
The clinical data for Blarcamesine, showing a sustained slowing of cognitive decline and a positive impact on quality of life over 144 weeks, is encouraging [143]. Its oral administration and favorable safety profile, which does not require intensive monitoring for ARIA, provide practical advantages over current immunotherapies [142] [144]. While regulatory hurdles remain—as evidenced by the ongoing dialogue with the EMA and FDA—the progress of Blarcamesine and other multi-target candidates like ANAVEX3-71 and HMTM signals a maturation of the AD drug development field [142] [144].
Future research should focus on further validating the biomarker-stratified precision medicine approach to identify patient populations most likely to respond to specific multi-target therapies. As the understanding of protein aggregation and clearance pathways deepens, the design of the next generation of multi-target drugs will become increasingly sophisticated, offering renewed hope for effectively halting or slowing the progression of Alzheimer's disease.
Alzheimer's disease (AD) represents a profound global health challenge, characterized pathologically by the accumulation of misfolded protein aggregates in the brain. The two primary hallmarks of AD are extracellular amyloid-β (Aβ) plaques and intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein [146] [117]. Over the past decades, therapeutic development has largely focused on the amyloid cascade hypothesis, which posits Aβ accumulation as the initiating molecular driver of AD pathogenesis [130]. However, the repeated failures of many Aβ-targeted clinical trials have prompted increased interest in alternative targets, particularly tau protein [146].
The relationship between Aβ and tau pathology is now understood to be bidirectional rather than linear. While Aβ aggregation is considered an early triggering event, tau pathology correlates more closely with cognitive decline and neuronal loss [147] [146]. Recent genetic and biomarker studies have revealed that Aβ can induce tau hyperphosphorylation and cleavage, which promotes tau aggregation and enhances its neurotoxicity [148]. The combined effects of Aβ and phosphorylated tau work synergistically to reduce glucose metabolism, sustain neuroinflammation, cause mitochondrial dysfunction, and lead to brain atrophy [148].
This comparative analysis evaluates the efficacy of major therapeutic modalities targeting protein aggregation in AD, with particular focus on their mechanisms of action, clinical performance, and potential integration within the broader context of protein aggregation clearance pathways.
Pathophysiological Basis of Protein Aggregation in Alzheimer's Disease
Amyloid-β Protein Aggregation
Aβ protein is generated through the sequential proteolytic cleavage of amyloid precursor protein (APP) by β-secretase (BACE1) and γ-secretase enzymes [130]. The amyloidogenic pathway produces Aβ peptides of varying lengths, with Aβ42 being particularly prone to aggregation due to its hydrophobic properties [130]. Under physiological conditions, a balance exists between Aβ generation and clearance mechanisms, including enzymatic degradation, transport across the blood-brain barrier, interstitial fluid bulk flow, and CSF absorption [130]. In AD, this balance is disrupted, leading to Aβ accumulation and aggregation.
The aggregation process follows a nucleation-dependent pathway beginning with soluble Aβ monomers that assemble into soluble oligomers, protofibrils, and finally mature fibrils that deposit as amyloid plaques [149]. Two main plaque types are observed in AD brains: classical plaques with compact cores surrounded by dystrophic neurites and inflammatory cells, and diffuse plaques with widely scattered Aβ deposits [130]. Importantly, classical plaques with inflammatory components correlate more strongly with cognitive impairment than diffuse plaques [130].
Tau Protein Aggregation and Spreading
Tau is a microtubule-associated protein predominantly expressed in neuronal axons, where it stabilizes microtubules and regulates axonal transport [147] [148]. In AD, tau undergoes abnormal post-translational modifications including hyperphosphorylation, acetylation, and truncation, which reduce its affinity for microtubules and promote its aggregation into NFTs [147] [146]. The adult human brain expresses six tau isoforms generated by alternative splicing of exons 2, 3, and 10 of the MAPT gene [147]. AD features a mixture of 3-repeat (3R) and 4-repeat (4R) tau isoforms in aggregates [146].
Tau pathology follows a stereotypical progression pattern through the brain, beginning in the entorhinal cortex and spreading to the hippocampus and neocortex [146]. This spreading occurs through a prion-like mechanism where misfolded tau seeds propagate between connected brain regions, template the misfolding of native tau, and initiate aggregation in recipient neurons [147]. The process is facilitated by synaptic connectivity and enhanced by innate immune signaling cascades [147].
Table 1: Key Pathological Proteins in Alzheimer's Disease
| Protein | Primary Location | Aggregate Structure | Clearance Mechanisms | Genetic Risk Factors |
|---|---|---|---|---|
| Amyloid-β | Extracellular space | Soluble oligomers, protofibrils, amyloid plaques | Enzymatic degradation (IDE, NEP), BBB transport, perivascular drainage, glymphatic system | APP, PSEN1, PSEN2, APOE4, TREM2 |
| Tau | Intracellular (axons, somatodendritic) | Soluble oligomers, paired helical filaments, neurofibrillary tangles | Ubiquitin-proteasome system, autophagy-lysosomal pathway, chaperone-mediated autophagy | MAPT, APOE4 |
Therapeutic Modalities Targeting Protein Aggregation
Anti-Aβ Immunotherapies
Anti-Aβ monoclonal antibodies represent the most advanced class of disease-modifying therapies for AD, with several agents now receiving regulatory approval. These antibodies target different forms of Aβ, including monomers, oligomers, protofibrils, or fibrils, leading to Fc-mediated clearance by microglia or peripheral sink mechanisms [130].
Aducanumab (approved by FDA in 2021) is a human monoclonal antibody that targets aggregated Aβ forms. In clinical trials, aducanumab demonstrated dose-dependent effects on amyloid plaque clearance, with significant reduction in plaque burden measured by PET imaging [150]. However, cognitive outcomes were inconsistent across trials, and the drug exhibited a high incidence of amyloid-related imaging abnormalities (ARIA), particularly ARIA-E (edema) [150].
Lecanemab (approved by FDA in 2023) targets Aβ soluble protofibrils. In the CLARITY AD phase 3 trial, lecanemab treatment over 18 months reduced markers of amyloid and showed a 27% reduction in cognitive decline on the ADCOMS scale compared to placebo [130] [150]. Importantly, 81% of patients achieved amyloid-negative PET scans after treatment [150]. The incidence of ARIA was lower than with aducanumab but remained a significant safety consideration.
Donanemab targets deposited amyloid plaques containing pyroglutamated Aβ. In the TRAILBLAZER-ALZ 4 study, donanemab demonstrated 76% plaque clearance and outperformed aducanumab in terms of amyloid clearance rates [130]. Cognitive outcomes showed a 35% slowing in decline for patients with early AD [150]. Donanemab treatment was associated with ARIA cases, particularly in APOE4 carriers.
Table 2: Efficacy and Safety of Anti-Aβ Monoclonal Antibodies in Phase III Trials
| Antibody | Target | Amyloid Clearance | Cognitive Outcome | ARIA-E Rate | ARIA-H Rate |
|---|---|---|---|---|---|
| Aducanumab | Aggregated fibrillar Aβ | Dose-dependent plaque reduction | Inconsistent across trials | ~35% (high dose) | ~19% (high dose) |
| Lecanemab | Soluble Aβ protofibrils | 81% achieve amyloid-negative PET | 27% reduction in decline (ADCOMS) | 12.6% | 17.3% |
| Donanemab | Deposited plaques (pyroglutamated Aβ) | 76% plaque clearance | 35% slowing of decline (iADRS) | 6.1% | 19.7% |
Tau-Targeted Therapeutic Strategies
Tau-targeted approaches have gained momentum due to the stronger correlation between tau pathology and cognitive impairment [146]. Multiple strategies are currently in clinical development, with immunotherapies representing the most advanced modality.
Tau immunotherapies include both active and passive vaccination approaches. Passive immunotherapies with anti-tau monoclonal antibodies aim to block intracellular tau aggregation, prevent tau seeding and spreading, or promote clearance of tau aggregates [147] [146]. These antibodies target specific tau epitopes, including phosphorylation sites (e.g., pSer396, pThr231), pathological conformations, or the microtubule-binding region [147]. Clinical trials have faced challenges related to target engagement, insufficient brain penetration, and the heterogeneity of tau pathology across different tauopathies [147].
Small molecule tau inhibitors represent another major approach. Tau aggregation inhibitors (e.g., methylthioninium derivatives) aim to prevent the conversion of soluble tau into insoluble aggregates by blocking nucleation or fibril elongation [146]. Kinase inhibitors target enzymes responsible for tau hyperphosphorylation, particularly glycogen synthase kinase-3β (GSK-3β) and cyclin-dependent kinase 5 (CDK5) [146]. However, these approaches have been limited by toxicity concerns and lack of efficacy in clinical trials, largely due to the redundancy of kinase pathways and poor selectivity of inhibitors [146].
Microtubule stabilizers represent an alternative approach to counteract the loss of tau function. Agents such as epothilone D have shown promise in preclinical models by restoring microtubule density and improving axonal transport, but clinical translation has been challenging due to toxicity concerns [146].
Emerging Modalities Targeting Proteostasis
Beyond direct targeting of Aβ and tau, novel approaches aim to enhance broader protein homeostasis mechanisms.
Molecular chaperones play crucial roles in maintaining proteostasis by assisting in proper protein folding, preventing aggregation, and promoting clearance of misfolded proteins [98]. Dysfunction in chaperone systems, including Hsp70, Hsp90, Hsp40, and small heat shock proteins, contributes to AD pathogenesis [98]. Therapeutic strategies include small molecule chaperone modulators, gene therapies to enhance chaperone expression, and approaches to boost the heat shock factor 1 (HSF1) transcriptional pathway [98].
Autophagy enhancers represent another promising strategy. Autophagy is a critical clearance pathway for aggregated proteins, and its function declines with aging and in AD [98]. Compounds that stimulate autophagy, such as mTOR inhibitors and TFEB activators, have shown efficacy in reducing both Aβ and tau pathology in preclinical models [98].
Protein degradation technologies including proteolysis-targeting chimeras (PROTACs) offer a novel approach to selectively target pathological proteins for degradation by the ubiquitin-proteasome system [117]. While still in early stages for neurodegenerative diseases, PROTACs represent a promising strategy for selectively degrading pathological protein species.
Experimental Methodologies for Evaluating Therapeutic Efficacy
Preclinical Assessment Protocols
Transgenic mouse models expressing human APP and/or tau mutations remain the cornerstone of preclinical AD research. Common models include APP/PS1 mice for Aβ pathology, 3xTg-AD mice for both Aβ and tau pathology, and tau transgenic models (e.g., P301S) for pure tauopathy [148]. Standardized protocols involve treatment initiation at different disease stages, behavioral testing (Morris water maze, novel object recognition), and post-mortem analysis of pathology.
Tau seeding and propagation assays have become essential for evaluating anti-tau therapies. The protocol involves injecting brain extracts from tauopathy mice or human AD patients into tau transgenic mouse brains and monitoring the spread of pathology over time [147]. Treatments are evaluated based on their ability to reduce seeding potency or block trans-synaptic spread of tau pathology.
Biochemical assessment of protein aggregation includes sequential protein extraction to separate soluble and insoluble protein fractions, followed by Western blot analysis to quantify pathological species [149]. Sedimentation assays, filter trap assays, and FRET-based biosensors provide additional methods to quantify oligomeric and aggregated species.
Clinical Trial Biomarkers and Endpoints
Amyloid PET imaging using tracers such as florbetapir, florbetaben, and flutemetamol provides quantitative assessment of amyloid plaque burden [130] [150]. Standardized protocols include baseline and follow-up scans, with central reading to minimize variability. Amyloid PET has served as a primary endpoint for accelerated approval of anti-amyloid antibodies.
Tau PET imaging with tracers like flortaucipir, MK-6240, and RO948 enables quantification of tau pathology distribution and density [146]. Tau PET is increasingly used as a secondary endpoint in clinical trials to assess target engagement of tau-directed therapies.
Cerebrospinal fluid (CSF) biomarkers including Aβ42/Aβ40 ratio, phosphorylated tau (p-tau), and total tau provide biochemical measures of pathology [146]. Standardized protocols for CSF collection, processing, and analysis have been established in multicenter trials.
Clinical outcome assessments include the Clinical Dementia Rating-Sum of Boxes (CDR-SB) as a primary endpoint for most recent phase 3 trials, along with secondary measures such as ADAS-Cog, ADCOMS, and functional scales [150]. Minimal clinically important difference (MCID) thresholds (e.g., 0.5-1.0 points for CDR-SB) are increasingly used to interpret the clinical meaningfulness of treatment effects.
Integrated Analysis of Therapeutic Efficacy
Comparative Efficacy Across Modalities
When comparing therapeutic modalities, anti-Aβ immunotherapies have demonstrated the most robust evidence for target engagement and disease modification in early AD [150]. The recent successes of lecanemab and donanemab represent a significant advancement, though effect sizes on cognitive measures remain modest (approximately 25-35% slowing of decline) [130] [150]. The clinical meaningfulness of these effects continues to be debated, particularly in relation to the significant safety considerations, especially ARIA.
Tau-targeted therapies, while theoretically promising due to the closer correlation between tau pathology and symptoms, have not yet demonstrated clear efficacy in late-stage trials [147] [146]. Challenges include the primarily intracellular location of tau pathology, which limits antibody access, and the heterogeneity of tau strains and modifications across different brain regions and disease stages [147].
Emerging approaches targeting proteostasis networks offer the potential for broader effects on multiple pathological proteins but remain at earlier stages of development [98]. The complexity of chaperone networks and autophagy regulation presents challenges for targeted therapeutic intervention without disrupting essential cellular functions.
Biomarker Responses Across Modalities
Different therapeutic modalities demonstrate distinct patterns of biomarker responses. Anti-Aβ antibodies produce rapid and substantial reduction in amyloid PET signal, with more variable effects on CSF Aβ measures [150]. Effects on tau biomarkers are typically more modest and delayed, consistent with the sequential relationship between Aβ and tau pathology.
Tau-targeted therapies show variable effects on CSF p-tau levels, with some approaches producing reduction while others show no significant change [146]. The relationship between CSF p-tau changes and clinical efficacy remains unclear based on available trial data.
The limited data available for proteostasis-targeted approaches suggests potential effects on multiple biomarker pathways, but comprehensive biomarker data from clinical trials is still lacking [98].
Visualization of Key Pathways and Methodologies
Alzheimer's Disease Therapeutic Target Pathways
Protein Aggregation and Clearance Pathways
Clinical Trial Evaluation Framework
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Alzheimer's Disease Therapeutic Development
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Transgenic Mouse Models | APP/PS1, 5xFAD, 3xTg-AD, P301S tau | Preclinical efficacy testing, mechanism studies | Model-specific pathology patterns, temporal progression |
| Tau Seeding Assays | HEK293 tau biosensor cells, brain extract inoculation | Measuring tau seeding and propagation potency | Standardization of preparation methods, quantification |
| Anti-Aβ Antibodies | 6E10, 4G8 (anti-Aβ); OC, A11 (conformation-specific) | Immunodetection, quantification of Aβ species | Epitope specificity, aggregation state recognition |
| Anti-Tau Antibodies | AT8, AT100, AT270 (phospho-specific); Tau5, Tau13 (total tau) | Assessing tau pathology, phosphorylation states | Phospho-specificity, isoform recognition, fixation compatibility |
| PET Tracers | Florbetapir, florbetaben (amyloid); Flortaucipir, MK-6240 (tau) | In vivo imaging of target engagement | Binding specificity, pharmacokinetics, quantification methods |
| CSF Biomarker Assays | ELISA, SIMOA, Lumipulse for Aβ42, p-tau, t-tau | Biomarker monitoring in clinical trials | Standardization, matrix effects, pre-analytical factors |
The comparative analysis of therapeutic modalities for Alzheimer's disease reveals a complex landscape with distinct efficacy profiles across different approaches. Anti-Aβ immunotherapies have demonstrated meaningful disease-modifying effects, particularly in early AD stages, though with modest clinical benefits and significant safety considerations. Tau-targeted therapies face greater development challenges but remain promising given the central role of tau in neurodegeneration. Emerging approaches focused on enhancing proteostasis offer potential for more comprehensive effects on protein aggregation pathology.
Future therapeutic development will likely require combination approaches targeting multiple aspects of the protein aggregation cascade, alongside improved patient stratification based on genetic and biomarker profiles. The continued refinement of biomarker tools and clinical trial methodologies will be essential for efficiently evaluating these next-generation therapies. As our understanding of protein aggregation clearance pathways deepens, more targeted and effective therapeutic strategies are expected to emerge, ultimately leading to improved outcomes for patients with Alzheimer's disease.
Alzheimer's disease (AD) research is undergoing a transformative shift, moving beyond the traditional amyloid-centric view to embrace a more complex, multi-faceted understanding of pathogenesis. The advancements in proteomics technologies are fundamentally reshaping AD research, revealing new molecular insights and accelerating biomarker discovery [45]. In the context of protein aggregation clearance pathways, proteomics provides an unprecedented window into the dynamic cellular responses to pathological protein accumulation, including amyloid-beta (Aβ) plaques and neurofibrillary tau tangles [45] [98]. The field has witnessed explosive growth, with PubMed listings for "Alzheimer's disease proteomics" studies nearly doubling since 2021, reaching 3,788 articles as of March 2025 [45]. This expansion reflects the critical role of proteomic signatures in unraveling the intricate molecular underpinnings of AD and identifying novel therapeutic targets within protein clearance pathways.
The integration of proteomic data across multiple studies has emerged as a particularly powerful approach for addressing the challenges of disease heterogeneity and validating targets with high confidence. By synthesizing results from independent cohorts and technological platforms, researchers can distinguish consistent, biologically-relevant protein alterations from cohort-specific noise or technological artifacts. This whitepaper examines the methodologies, applications, and implementation frameworks for establishing consensus proteomic signatures in AD, with particular emphasis on their relationship to protein aggregation and clearance mechanisms.
Core Concept: Defining Consensus Proteomic Signatures
Conceptual Foundation and Significance
A consensus proteomic signature represents a set of protein alterations consistently identified across multiple independent studies, technological platforms, and patient cohorts. Unlike findings from single studies, which may reflect cohort-specific characteristics or technological biases, consensus signatures represent robust, validated molecular patterns with higher potential for clinical translation and therapeutic targeting. The fundamental premise is that proteins consistently altered across diverse experimental conditions are more likely to reflect core disease mechanisms rather than ancillary processes or methodological artifacts.
In AD research, the identification of consensus signatures has proven particularly valuable due to the disease's complex pathology, extended prodromal phase, and frequent co-occurrence of multiple proteinopathies [151]. The establishment of these signatures enables researchers to move beyond the traditional Aβ and tau framework to identify novel disease-associated proteins and pathways that may mediate the relationship between protein aggregation and neuronal dysfunction [45].
Key Integrative Analyses in Alzheimer's Disease
Recent large-scale integrative analyses have demonstrated the power of the consensus approach. A comprehensive review integrating more than 30 whole proteome datasets from AD brains identified 866 consensus proteins that show consistent alterations across studies [45]. This meta-analysis revealed that these consensus proteins originate from diverse cell types, with microglia contributing the largest proportion (~40%), followed by neurons and astrocytes, along with smaller contributions from endothelial cells and oligodendrocytes [45]. Pathway analysis of these proteins highlighted upregulated processes related to amyloid matrisome, cell migration, complement/coagulation, cytoskeleton organization, and immune response, providing a comprehensive view of the cellular ecosystem in AD pathogenesis [45].
Another landmark study combining radioligand imaging of Aβ plaques and tau tangles with cerebrospinal fluid (CSF) proteomics identified 127 differentially abundant proteins (DAPs) across the AD spectrum [72]. This approach allowed researchers to distinguish protein signatures associated specifically with Aβ pathology versus those linked to tau aggregation, revealing distinct biological processes active at different disease stages. The study further validated these findings across independent cohorts (BioFINDER-1 and ADNI), achieving 90-92% consistency in differential abundance analyses [72].
Table 1: Key Consensus Proteomic Signatures in Alzheimer's Disease
| Signature Category | Representative Proteins | Biological Process | Validation Status |
|---|---|---|---|
| Microglial/Immune Response | ITGAM, GPNMB, SMOC1 | Neuroinflammation, phagocytosis | Cross-platform validation [45] [72] |
| Neuronal/Synaptic | NPTX2, NRN1, VGF, NRGN | Synaptic plasticity, neuronal activity | Consistent across ≥3 cohorts [45] [72] |
| Protein Clearance | U1 snRNP, HSP70, HSP90 | Protein homeostasis, aggregation prevention | Functional validation [45] [98] |
| Early Aβ-Associated | SMOC1, MDK, PTN | Response to Aβ pathology | Elevated in A+T- stage [72] |
| Late Tau-Associated | FABP3, ENO2, ENO1 | Energy metabolism, neurodegeneration | Correlated with tau-PET [72] |
Technical Workflow: From Data Generation to Consensus Validation
Proteomic Technologies and Platforms
Modern proteomics leverages multiple complementary technological platforms, each with distinct strengths and limitations for biomarker discovery and validation. The selection of appropriate platforms depends on study objectives, sample availability, and required proteome coverage.
Mass Spectrometry (MS)-Based Approaches:
- Tandem Mass Tag (TMT) MS: Enables multiplexed quantification of over 10,000 proteins across up to 35 samples per batch when combined with two-dimensional liquid chromatography [45]. Advantages include high proteome coverage, extensive multiplexing, and minimal missing data, though it requires expensive labeling reagents and suffers from ratio suppression due to coeluting peptides [45].
- Data-Independent Acquisition (DIA) MS: Provides high sensitivity and single-run identification of thousands of proteins, with recent advances like the Asymmetric Track Lossless (Astral) analyzer increasing coverage to 10,000 proteins with <1μg protein loading [45]. Ion mobility technologies (TIMS, FAIMS) further enhance separation power [45].
- Parallel Reaction Monitoring (PRM): A targeted MS approach offering exceptional specificity and quantitative accuracy for validation studies, typically enabling precise measurement of tens to hundreds of proteins from <1μg of starting material [45].
Affinity-Based Platforms:
- Olink: Employs dual antibody-based probes to detect >5,400 proteins from ~6μL of sample, providing high sensitivity and reproducibility [45].
- SomaScan: Uses DNA aptamers to measure up to 11,000 proteins, requiring only ~50μL of sample [45]. Both platforms offer automated, high-throughput analysis suitable for large cohorts but are constrained by pre-designed affinity reagents that may exhibit cross-reactivity [45].
Multi-Study Integration Methodologies
Establishing consensus proteomic signatures requires rigorous statistical frameworks and data harmonization approaches to integrate findings across diverse studies and platforms.
Cross-Platform Validation: The strongest consensus signatures demonstrate consistency across different proteomic technologies. For example, SMOC1 was identified as a prominent Aβ-associated protein in both Olink and SomaScan platforms across multiple cohorts [72]. This cross-platform consistency significantly strengthens the biological validity of findings.
Cross-Species Comparison: Comparing human AD brain proteomes with those from mouse models (e.g., 5xFAD, APP-KI) reveals shared pathways in amyloid pathology while highlighting limitations in recapitulating the full complexity of human disease [45]. Of 866 consensus proteins identified in human AD brain, 654 were detected in mice, with 108 consistently altered in both species [45].
Multi-Omics Integration: Combining proteomics with genomics enables protein quantitative trait locus (pQTL) analysis, linking genetic risk factors to protein expression changes [45]. Similarly, comparing proteomic and transcriptomic data reveals discrepancies that suggest altered protein turnover in AD, providing insights into post-transcriptional regulatory mechanisms [45].
Diagram 1: Workflow for Establishing Consensus Proteomic Signatures. This integrated approach spans from sample processing through functional validation, emphasizing multi-study integration as a critical component.
Alzheimer's Disease Application: Protein Aggregation and Clearance Pathways
Stage-Specific Proteomic Alterations in AD Continuum
Consensus proteomic analyses have revealed distinct protein signatures associated with different stages of AD pathology, providing insights into the temporal sequence of biological processes in disease progression. A groundbreaking study combining Aβ and tau PET imaging with CSF proteomics in 877 participants from the BioFINDER-2 cohort identified stage-specific proteomic alterations [72].
Early Aβ-Associated Signatures: The comparison between A-T- (no AD pathology) and A+T- (isolated Aβ pathology) individuals revealed 51 differentially abundant proteins, 94% of which were upregulated in those with isolated Aβ pathology [72]. SMOC1 emerged as the most strongly Aβ-associated protein, elevated in A+T- individuals but not further increased with tau pathology development [72]. Other early proteins included MDH1, SNAP29, SOD1, and SOD2, suggesting activation of oxidative stress response and metabolic adaptation early in AD continuum.
Tau-Associated Signatures: The transition from isolated Aβ pathology (A+T-) to both Aβ and tau pathology (A+T+) revealed more extensive proteomic changes, with 45 upregulated and 48 downregulated proteins [72]. A core set of 15 proteins (including CNP, CRKL, ITGAM, ITGB2, and MAPT) were elevated in A+T- participants and showed further elevation in the A+T+ group, representing a continuous response throughout AD pathology progression [72]. Proteins specifically associated with tau pathology included FABP3, ENO2, ENO1, MAPT, NRGN, MIF, TMSB10, and GLOD4, with higher CSF levels correlating with greater tau fibrillar pathology independent of Aβ load [72].
Molecular Chaperones in Protein Misfolding and Clearance
Within consensus signatures, molecular chaperones represent critical components of the protein quality control system that becomes dysregulated in AD. These chaperones, including heat shock proteins (HSP70/HSP40, HSP90, HSP27, HSP100), actively maintain protein homeostasis by assisting in proper folding, preventing aggregation, and promoting clearance of misfolded proteins [98]. Dysfunction in chaperone systems contributes significantly to AD pathogenesis, as they normally serve as a first line of defense against protein misfolding and facilitate the clearance of aggregation-prone proteins like Aβ and tau through proteasomal and autophagic pathways [98].
The therapeutic targeting of molecular chaperones represents a promising strategy for restoring protein homeostasis in AD. Recent research has explored chaperone-based interventions, including small molecules, gene therapies, and autophagy and proteasomal degradation modulators [98]. These approaches aim to enhance the capacity of the protein quality control system to handle the increased burden of misfolded proteins in AD, potentially disrupting the vicious cycle of protein aggregation and cellular dysfunction.
Blood-Brain Barrier Transport and Aβ Clearance
Consensus proteomic analyses have also shed light on alterations in blood-brain barrier (BBB) function in AD, particularly regarding the transport machinery responsible for Aβ clearance. Low-density lipoprotein receptor-related protein 1 (LRP1) plays a vital role in removing Aβ from the brain, and its expression decreases with age, a phenomenon more pronounced in AD patients and animal models [21]. The downregulation of LRP1 strongly correlates with BBB impairment and cognitive decline [21].
Recent research has revealed that LRP1-mediated trafficking follows distinct routes influenced by cargo avidity, with mid-avidity interactions favoring PACSIN2-dependent transcytosis (promoting Aβ clearance) while high-avidity interactions trigger Rab5-directed lysosomal degradation (reducing LRP1 availability) [21]. This understanding has inspired novel therapeutic strategies that target LRP1 with engineered mid-avidity ligands to bias trafficking toward clearance pathways, demonstrating rapid Aβ reduction and cognitive recovery in AD models [21].
Table 2: Protein Aggregation Clearance Pathways Identified Through Consensus Proteomics
| Clearance Pathway | Key Protein Components | AD-Related Alterations | Therapeutic Targeting Approaches |
|---|---|---|---|
| Molecular Chaperones | HSP70, HSP90, HSP27, HSP100 | Dysfunction in protein folding and refolding | Small molecule chaperone modulators, HSF1 activators [98] |
| Ubiquitin-Proteasome System | U1 snRNP, CHIP, E3 ubiquitin ligases | Impaired degradation of misfolded proteins | Proteasome activators, ubiquitin ligase modulators [98] |
| Autophagy-Lysosomal Pathway | LAMP2, CTSD, MAP1LC3 | Reduced autophagic flux, lysosomal dysfunction | Autophagy enhancers (e.g., rapamycin analogs) [98] |
| BBB Transcytosis | LRP1, PACSIN2, PICALM | LRP1 downregulation, biased trafficking | Avidity-optimized LRP1 ligands, tubular trafficking promoters [21] |
| Microglial Phagocytosis | ITGAM, GPNMB, TREM2 | Altered phagocytic activity, chronic inflammation | TREM2 agonists, complement pathway modulators [45] [72] |
Diagram 2: Protein Aggregation and Clearance Pathways in Alzheimer's Disease. This diagram illustrates the disruption of normal protein homeostasis in AD and the cellular responses identified through consensus proteomics, along with potential therapeutic intervention points.
Implementation Framework: Global Collaboration and Data Sharing
Large-Scale Consortia and Standardized Protocols
The establishment of robust consensus proteomic signatures requires large-scale collaborative efforts and standardized methodologies to ensure data comparability across studies. The Global Neurodegeneration Proteomics Consortium (GNPC) represents a paradigm-shifting approach to this challenge, having established one of the world's largest harmonized proteomic datasets [151]. This public-private partnership includes approximately 250 million unique protein measurements from multiple platforms across more than 35,000 biofluid samples (plasma, serum, and cerebrospinal fluid) contributed by 23 partners [151]. The dataset spans Alzheimer's disease, Parkinson's disease, frontotemporal dementia, and amyotrophic lateral sclerosis, enabling the identification of both disease-specific and transdiagnostic proteomic signatures [151].
Standardization remains critical for successful multi-study integration. Research presented at the 2025 Human Amyloid Imaging (HAI) conference emphasized the need for harmonized protocols across studies to improve consistency and comparability in multicenter trials [152]. Advances in data harmonization methods, including advanced statistical models and AI-driven analytics, are being explored as potential solutions to the challenges of integrating data from diverse sources and technological platforms [152].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Consensus Proteomics
| Category | Specific Solutions | Key Applications | Technical Considerations |
|---|---|---|---|
| Proteomic Profiling Platforms | Olink Explore 3072, SomaScan 11k, TMTpro 16/18-plex | Discovery-phase proteomic profiling | Platform selection depends on sample volume, coverage needs, and budget [45] [72] |
| Targeted Validation Assays | Parallel Reaction Monitoring (PRM), Olink Target 96, SomaScan Mini | Hypothesis-driven validation of candidate biomarkers | PRM offers antibody-free validation; affinity assays provide high sensitivity [45] |
| Sample Preparation Kits | Protease inhibitor cocktails, protein extraction kits, depletion columns | Sample preparation and pre-analytical processing | Standardized protocols essential for cross-study comparisons [152] |
| Data Analysis Tools | Spectronaut, DIA-NN, Skyline, custom R/Python pipelines | Proteomic data processing and statistical analysis | Implementation of harmonized processing parameters critical for integration [151] |
| Reference Materials | Common reference samples, pooled quality controls | Inter-batch and inter-study normalization | Inclusion in every batch enables technical variation adjustment [152] |
The integration of proteomic data across multiple studies to establish consensus signatures represents a powerful paradigm for advancing Alzheimer's disease research. This approach has identified robust molecular signatures associated with different stages of AD pathology, revealed novel players in protein aggregation clearance pathways, and provided a framework for therapeutic target prioritization. The identification of 866 consensus proteins altered in AD brain tissue [45] and stage-specific signatures along the AD continuum [72] demonstrates the power of this methodology to distill complex molecular data into biologically and clinically meaningful insights.
As the field progresses, several key areas will be critical for maximizing the impact of consensus proteomic approaches: First, continued expansion of diverse, multi-ethnic cohorts will enhance the generalizability of findings and enable precision medicine applications. Second, the integration of proteomics with other omics modalities (genomics, transcriptomics, metabolomics) will provide a more comprehensive understanding of the molecular networks underlying AD pathogenesis. Third, the development of standardized protocols and data sharing frameworks, exemplified by initiatives like the GNPC [151], will accelerate validation and clinical translation.
For researchers and drug development professionals, consensus proteomic signatures offer a validated foundation for target selection, biomarker development, and patient stratification strategies. By focusing on proteins and pathways consistently altered across independent studies, the field can prioritize the most promising targets for therapeutic intervention and develop robust biomarker panels for early detection and disease monitoring. As these approaches mature, they hold significant promise for delivering the precision medicines desperately needed to address the growing global challenge of Alzheimer's disease.
Conclusion
The investigation of protein aggregation clearance pathways represents a paradigm shift in Alzheimer's disease research, moving beyond synthesis inhibition to enhancing endogenous degradation and removal systems. Successful therapeutic strategies will likely require combinatorial approaches that target multiple clearance mechanisms simultaneously—enzymatic degradation, cellular clearance, and transport systems—while accounting for disease stage and individual patient profiles. Future directions should focus on developing more sensitive biomarkers for early detection of clearance impairment, advancing targeted delivery systems across the blood-brain barrier, and personalizing therapies based on genetic and proteomic profiling. The recent successes of immunotherapies and emerging proteomic technologies provide unprecedented opportunities to develop truly disease-modifying treatments that leverage the brain's innate clearance machinery, offering hope for effective Alzheimer's disease interventions in the coming decade.
References
- 1. Current Understanding of Protein Aggregation in ... [https://www.mdpi.com/1422-0067/26/21/10568]
- 2. Amyloid β oligomers in Alzheimer's disease pathogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4390393/]
- 3. Understanding the Pathophysiological Actions of Tau ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2020.00155/full]
- 4. The Amyloid-β Pathway in Alzheimer's Disease [https://www.nature.com/articles/s41380-021-01249-0]
- 5. Tau and neuroinflammation in Alzheimer's disease [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02853-3]
- 6. Tau Oligomers in Alzheimer's Disease: Modulation Effect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333032/]
- 7. The role of protein clearance mechanisms in organismal ... [https://www.nature.com/articles/ncomms6659]
- 8. Protein clearance strategies for disease intervention - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8541819/]
- 9. The Role of Neprilysin and Insulin-Degrading Enzyme in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139590/]
- 10. Abeta-degrading enzymes in Alzheimer's disease [https://pubmed.ncbi.nlm.nih.gov/18363935/]
- 11. Amyloid-Beta Protein Clearance and Degradation (ABCD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4820400/]
- 12. “Neprilysin vs insulysin”, “monomeric vs aggregate”, and “ ... [https://www.sciencedirect.com/science/article/pii/S2405580822000681]
- 13. Degradation of Alzheimer's amyloid-β by a catalytically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169600/]
- 14. Impairment of the autophagy–lysosomal pathway in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9069408/]
- 15. Clearance systems in the brain—implications for Alzheimer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4694579/]
- 16. The ubiquitin-proteasome system in Alzheimer's disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3822529/]
- 17. Autophagy in Alzheimer's disease pathogenesis [https://www.sciencedirect.com/science/article/pii/S1568163721002117]
- 18. Autophagy-lysosomal pathway impairment and cathepsin ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2024.1490275/full]
- 19. The ubiquitin-proteasome system in Alzheimer's disease ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1730206/full]
- 20. Brain clearance of protein aggregates: a close-up on astrocytes [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00703-1]
- 21. Rapid amyloid-β clearance and cognitive recovery through ... [https://www.nature.com/articles/s41392-025-02426-1]
- 22. Scientists reverse Alzheimer's in mice with groundbreaking ... [https://www.sciencedaily.com/releases/2025/10/251029100154.htm]
- 23. New Alzheimer's Treatment Clears Plaques From Brains of ... [https://www.sciencealert.com/new-alzheimers-treatment-clears-plaques-from-brains-of-mice-within-hours]
- 24. Neurovascular Unit Dysfunction and Neurodegenerative ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00334/full]
- 25. A Paravascular Pathway Facilitates CSF Flow Through the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3551275/]
- 26. Perivascular spaces around arteries exceed perivenous ... [https://www.nature.com/articles/s41598-024-67885-y]
- 27. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 28. Nanoparticle transport across the blood brain barrier - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4836460/]
- 29. Experimental Methods and Transport Models for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5349708/]
- 30. Role of LRP1 in the pathogenesis of Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496044/]
- 31. LRP1 at the crossroads of Parkinson's and Alzheimer's [https://www.sciencedirect.com/science/article/pii/S0014299925005849]
- 32. Characteristics of compounds that cross the blood-brain barrier [https://bmcneurol.biomedcentral.com/articles/10.1186/1471-2377-9-S1-S3]
- 33. Mechanisms of Aβ Clearance and Degradation by Glial Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC4932097/]
- 34. Mechanisms of Aβ Clearance and Degradation by Glial Cells [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2016.00160/full]
- 35. Microglial phagocytosis in Alzheimer disease [https://www.nature.com/articles/s41582-025-01162-y]
- 36. Microglia-Mediated Phagocytosis in Alzheimer's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12650038/]
- 37. Glial phagocytosis for synapse and toxic proteins in ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00870-9]
- 38. Apolipoprotein E in Alzheimer's disease: molecular insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12023563/]
- 39. APOE4 to APOE2 allelic switching in mice improves ... [https://www.nature.com/articles/s41593-025-02094-y]
- 40. APOE and TREM2 regulate amyloid responsive microglia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7520051/]
- 41. TREM2 in Neurodegenerative Disorders: Mutation Spectrum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346578/]
- 42. Roles of TREM2 in the Pathological Mechanism and ... [https://www.sciencedirect.com/science/article/pii/S2274580724006976]
- 43. The Specific Mechanism of TREM2 Regulation of Synaptic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.845897/full]
- 44. Genetic risk factors have a substantial impact on healthy ... [https://www.nature.com/articles/s41591-022-01957-2]
- 45. Proteomic landscape of Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257826/]
- 46. Proteomics Landscape of Alzheimer's Disease [https://www.mdpi.com/2227-7382/9/1/13]
- 47. Systems-based proteomics to resolve the biology of ... [https://www.nature.com/articles/s41386-020-00840-3]
- 48. Proteomic landscape of Alzheimer's Disease: novel insights ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-021-00474-z]
- 49. A peptide-centric quantitative proteomics dataset for the ... [https://www.nature.com/articles/s41597-023-02057-7]
- 50. Report Alzheimer's disease early diagnostic and staging ... [https://www.sciencedirect.com/science/article/pii/S2666675823001728]
- 51. Deep Profiling of the Aggregated Proteome in Alzheimer's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6313861/]
- 52. Proteomic landscape of Alzheimer's disease: emerging ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00874-5]
- 53. Misfolding and aggregation in neurodegenerative diseases : protein ... [https://link.springer.com/article/10.1186/s12964-024-01791-8]
- 54. Emerging affinity-based proteomic technologies for large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5555416/]
- 55. Large-scale plasma proteomics comparisons through ... [https://www.nature.com/articles/s41586-023-06563-x]
- 56. Biomarker discovery in Alzheimer's and neurodegenerative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12096316/]
- 57. Publication highlights September 2025 [https://olink.com/blog/publication-highlights-sept-2025]
- 58. Multi-platform proteomic analysis of Alzheimer's disease ... [https://olink.com/publication/multi-platform-proteomic-analysis-of-alzheimers-disease-cerebrospinal-fluid-and-plasma-reveals-network-biomarkers-associated-with-proteostasis-and-the-matrisome]
- 59. Advantages of Mass Spectrometry Biomarker Discovery ... [https://biognosys.com/advantages-mass-spectrometry-biomarker-discovery-proteomics/]
- 60. Current Understanding of Protein in Neurodegenerative... Aggregation [https://pubmed.ncbi.nlm.nih.gov/41226604/]
- 61. Benchmarking of a multi-biomarker low-volume panel for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11213109/]
- 62. The role of clearance mechanisms in the kinetics ... [https://pubmed.ncbi.nlm.nih.gov/33810689/]
- 63. Protein Aggregation linked to Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6401270/]
- 64. Saturation Transfer MRI for Detection of Metabolic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8773856/]
- 65. Chemical Exchange Saturation Transfer Contrast Agents for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2709739/]
- 66. Clinical Translation of Integrated PET-MRI for ... [https://pubmed.ncbi.nlm.nih.gov/40679171/]
- 67. PET Tracers, Co-pathology and PPMI Findings Featured at ... [https://www.michaeljfox.org/news/pet-tracers-co-pathology-and-ppmi-findings-featured-2025-adpd-conference]
- 68. AD/PD™ 2025: Advances in Science & Therapy [https://www.alzforum.org/print-series/3423841]
- 69. Protein aggregation and its affecting mechanisms in ... [https://www.sciencedirect.com/science/article/pii/S0197018624002079]
- 70. Hi-Res Spatial Proteomics Uncovers Aspects of ... [https://www.alzforum.org/news/research-news/hi-res-spatial-proteomics-uncovers-aspects-alzheimers-disease-pathology]
- 71. Benchmarking informatics workflows for data-independent ... [https://www.nature.com/articles/s41467-025-65174-4]
- 72. Proteomic changes in Alzheimer's disease associated with ... [https://www.nature.com/articles/s41593-024-01737-w]
- 73. Imaging protein aggregates in the serum and cerebrospinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014748/]
- 74. “Proteinjury”: a universal pathological mechanism ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1593122/full]
- 75. Blood-based biomarkers of Alzheimer's disease and ... [https://www.nature.com/articles/s41591-025-03605-x]
- 76. FDA Clears First Blood Test Used in Diagnosing ... [https://www.fda.gov/news-events/press-announcements/fda-clears-first-blood-test-used-diagnosing-alzheimers-disease]
- 77. Alzheimer's Association Welcomes FDA Clearance of First ... [https://www.alz.org/news/2025/fda-clearance-blood-test-primary-care-rule-out-alzheimers-related-amyloid-pathology]
- 78. Roche's Elecsys® pTau181 becomes the only FDA-cleared ... [https://www.roche.com/investors/updates/inv-update-2025-10-13b]
- 79. New Clinical Practice Guideline for Blood-Based Biomarkers [https://aaic.alz.org/releases-2025/clinical-practice-guideline-blood-based-biomarkers.asp]
- 80. Translatability of Animal Models for Alzheimer's Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603623/]
- 81. Rodent models of Alzheimer's disease: Critical analysis ... [https://www.sciencedirect.com/science/article/pii/S0301008225001121]
- 82. Lost in translation: Inconvenient truths on the utility of ... [https://elifesciences.org/articles/90633]
- 83. Exploring efficient and effective mammalian models for ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1652754/full]
- 84. New nanotherapy clears amyloid-β reversing Alzheimer's ... [https://www.drugtargetreview.com/news/189235/new-nanotherapy-clears-amyloid-%CE%B2-reversing-alzheimers-in-mice/]
- 85. Advancement in modeling of Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12364833/]
- 86. New insights into translational research in Alzheimer's ... [https://www.sciencedirect.com/science/article/pii/S2211383525005647]
- 87. Mechanisms of Amyloid-β Peptide Clearance - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3794520/]
- 88. Age-Related Decline in Brain and Hepatic Clearance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5248655/]
- 89. Importance of CSF-based Aβ clearance with age in ... [https://www.nature.com/articles/s42003-022-03037-0]
- 90. Molecular Mechanisms of Autophagy Decline during Aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11352966/]
- 91. Emerging rejuvenation strategies—Reducing the biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8761015/]
- 92. Prion-Like Propagation of Protein Aggregation and Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3701767/]
- 93. Structural Variations of Prions and Prion-like Proteins ... [https://www.mdpi.com/1467-3045/46/7/384]
- 94. “Prion-like” seeding and propagation of oligomeric protein ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1436262/full]
- 95. Differential Inhibition of Prion by Enantiomers of... Propagation [https://www.nature.com/articles/3780670?error=cookies_not_supported&code=67c11f69-77d4-425c-8d95-12810a94c241]
- 96. Antiprion Drugs as Chemical Tools to Uncover Mechanisms of Prion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2633708/]
- 97. Novel Compounds Identified by Structure-Based Prion Disease Drug ... [https://link.springer.com/article/10.1007/s13311-020-00903-9]
- 98. Targeting protein misfolding in Alzheimer's disease [https://www.sciencedirect.com/science/article/pii/S0753332225007255]
- 99. The blood-brain barrier in Alzheimer's disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5600438/]
- 100. Blood-brain barrier dysfunction and Alzheimer's disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC10679748/]
- 101. Relationship Between Amyloid-β Deposition and Blood–Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8326917/]
- 102. Reconsidering the role of blood-brain barrier in Alzheimer's ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2023.1102809/full]
- 103. Restoring brain barriers: an innovative approach for treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243347/]
- 104. Restoring the blood-brain barrier? - Stanford Medicine [https://med.stanford.edu/news/insights/2023/06/restoring-the-blood-brain-barrier.html]
- 105. Blood–Brain Barrier, Lymphatic Clearance, and Recovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC6320935/]
- 106. Recent advances in immunotherapy targeting amyloid-beta ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12220716/]
- 107. Peptide for Alzheimer's increases clearance of amyloid ... [https://www.ddw-online.com/peptide-for-alzheimers-increases-clearance-of-amyloid-plaques-35853-202508/]
- 108. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 109. Blood-Based Tau as a Biomarker for Early Detection and ... [https://pubmed.ncbi.nlm.nih.gov/41226373/]
- 110. Alzheimer Combination Therapies: Overview and Scenarios [https://www.sciencedirect.com/science/article/pii/S2274580725002717]
- 111. Emerging non-traditional biomarkers for alzheimer`s ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725000820]
- 112. Alzheimer Combination Therapies: Overview and Scenarios [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627886/]
- 113. Harnessing combination therapy: Current treatments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627881/]
- 114. Systematic review of amyloid-beta clearance proteins from the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11974662/]
- 115. Challenges and opportunities for novel combination ... [https://www.sciencedirect.com/science/article/pii/S2274580725001086]
- 116. CKG-IMC: An inductive matrix completion method ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482524006978]
- 117. Recent advances in Alzheimer's disease: mechanisms ... [https://www.nature.com/articles/s41392-024-01911-3]
- 118. Mechanistic Models of Protein Aggregation Across Length ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9281552/]
- 119. The Interplay of Protein Aggregation, Genetics, and ... [https://www.mdpi.com/2076-3921/13/7/862]
- 120. Clearance of protein aggregates during cell division [https://elifesciences.org/reviewed-preprints/96675v1]
- 121. Disease-Modifying Drugs for Alzheimer's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610953/]
- 122. Eisai to Present Data on Lecanemab Continued Treatment ... [https://www.eisai.com/news/2025/news202580.html]
- 123. The Alzheimer's therapeutic Lecanemab attenuates Aβ ... [https://www.nature.com/articles/s41593-025-02125-8]
- 124. Study elucidates how anti-amyloid antibody therapy ... [https://www.news-medical.net/news/20251125/Study-elucidates-how-anti-amyloid-antibody-therapy-lecanemab-works-in-Alzheimers-disease.aspx]
- 125. Re-evaluation of the efficacy and safety of anti-Aβ monoclonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12040886/]
- 126. Immunotherapy Targeting Pathological Tau Protein in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2757121/]
- 127. The Role of Neprilysin and Insulin-Degrading Enzyme in ... [https://pubmed.ncbi.nlm.nih.gov/40300834/]
- 128. Understanding the Insulin-Degrading Enzyme: A New Look ... [https://www.mdpi.com/1422-0067/26/14/6693]
- 129. Basics of Enzymatic Assays for HTS - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK92007/]
- 130. Amyloid β-based therapy for Alzheimer's disease [https://www.nature.com/articles/s41392-023-01484-7]
- 131. The concerted amyloid-beta clearance of LRP1 and ABCB1/P ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7748946/]
- 132. LRP1 at the Crossroads of Aβ Clearance and Therapeutic ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1669405/full]
- 133. Low-Density Lipoprotein Receptor-Related Protein 1 as a ... [https://www.mdpi.com/1999-4923/16/7/948]
- 134. Endothelial delivery of simvastatin by LRP1-targeted ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01840-5]
- 135. LRP1 Has a Predominant Role in Production over Clearance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6728278/]
- 136. A Role for P-Glycoprotein in Clearance of Alzheimer Amyloid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5102249/]
- 137. Targeted Nanoparticles for Drug Delivery Across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627166/]
- 138. Protein aggregation and degradation mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3601466/]
- 139. Multi-Targets: An Unconventional Drug Development ... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2022.837649/full]
- 140. Multi-target pharmacology: possibilities and limitations of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4585027/]
- 141. Controversial New Alzheimer's Drugs Offer Hope—But at a ... [https://www.nature.com/articles/d41586-025-02927-7]
- 142. Anavex Life Sciences Provides Regulatory Update on ... [https://www.anavex.com/post/anavex-life-sciences-provides-regulatory-update-on-blarcamesine-for-early-alzheimer-s-disease]
- 143. Earnings call transcript: Anavex Q4 2025 reveals ... [https://www.investing.com/news/transcripts/earnings-call-transcript-anavex-q4-2025-reveals-alzheimers-drug-progress-93CH-4377563]
- 144. Researching new drugs for Alzheimer's disease [https://www.alzheimers.org.uk/what-we-do/researchers/news/researching-new-drugs-alzheimers-disease]
- 145. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 146. Tau-targeting therapies for Alzheimer disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463489/]
- 147. Tau-Targeted Therapeutic Strategies - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523266/]
- 148. Therapeutic Modalities Targeting Tau Protein in ... [https://www.mdpi.com/3042-4518/2/3/32]
- 149. Targeting Protein Aggregation for the Treatment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4628595/]
- 150. A Systematic Review of the Efficacy and Safety of Anti ... [https://pubmed.ncbi.nlm.nih.gov/40621323/]
- 151. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 152. Breaking New Ground in Alzheimer's Research [https://www.quanterix.com/blog-breaking-new-ground-in-alzheimers-research-key-takeaways-from-hai-2025/]