Targeting Protein Misfolding in Hypoxic Tumors: Mechanisms, Therapeutic Strategies, and Clinical Implications
This article provides a comprehensive analysis of protein misfolding mechanisms within the hypoxic tumor microenvironment, a critical yet underexplored hallmark of cancer.
Targeting Protein Misfolding in Hypoxic Tumors: Mechanisms, Therapeutic Strategies, and Clinical Implications
Abstract
This article provides a comprehensive analysis of protein misfolding mechanisms within the hypoxic tumor microenvironment, a critical yet underexplored hallmark of cancer. Tailored for researchers, scientists, and drug development professionals, it explores the foundational biology linking hypoxia to endoplasmic reticulum stress and the unfolded protein response (UPR). The content details current methodological approaches for modeling and detecting misfolding in vitro and in vivo, discusses key challenges and optimization strategies in therapeutic development, and validates these approaches through comparative analysis of emerging pharmacological agents. The synthesis offers a roadmap for translating mechanistic insights into novel cancer therapeutics that exploit tumor-specific proteostatic vulnerability.
The Hypoxic Nexus: How Low Oxygen Triggers Protein Misfolding and ER Stress in Solid Tumors
Technical Support Center: Troubleshooting Experimental Challenges
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My western blot for HIF-1α in hypoxic cell lysates shows weak or no signal. What could be wrong? A: This is a common issue. Follow this checklist:
- Sample Preparation: HIF-α subunits are rapidly degraded under normoxia. Ensure you are using fresh lysates prepared directly in the hypoxia workstation or by rapid lysis with inhibitors. Use a complete protease inhibitor cocktail and specific proteasome inhibitors (e.g., MG-132) to stabilize HIF-α before protein extraction.
- Hypoxia Validation: Confirm your hypoxia chamber/workspace is correctly calibrated. Use an independent chemical hypoxia mimic (e.g., CoCl₂ at 100-200 µM for 4-6 hours) as a positive control.
- Antibody Specificity: Validate your antibody with a known positive control (e.g., lysate from cells treated with DMOG, a PHD inhibitor) and check for cross-reactivity with HIF-2α. Running both normoxic and hypoxic samples side-by-side is critical.
Q2: How can I accurately measure oxygen gradients and heterogeneity in my 3D tumor spheroid model? A: Oxygen gradients are inherent in spheroids >~500 µm in diameter.
- Issue: Bulk measurements mask heterogeneity.
- Solution: Implement hypoxia probes with different sensing ranges.
- Pimonidazole HCl: Administer to cultures pre-harvest. It forms adducts in cells with pO₂ < 10 mmHg (~1.3% O₂). Detect via immunofluorescence (IF) or flow cytometry.
- Fluorescent Reporters: Use lentiviral constructs with Hypoxia Response Elements (HRE) driving GFP or other fluorophores. This allows live imaging of gradient formation.
- Quantitative Mapping: For fixed samples, combine pimonidazole IF with staining for CA9 (Carbonic Anhydrase IX), a robust HIF-1 target, to visualize the hypoxic gradient and its functional output.
Q3: I need to distinguish the specific roles of HIF-1α versus HIF-2α in my tumor model. What is the best experimental approach? A: Specific knockdown/rescue is the standard.
- Problem: Non-specific siRNA/shRNA or overlapping functions.
- Protocol:
- Validation of Specificity: Use qPCR with isoform-specific primers for known target genes (e.g., CA9 and BNIP3 for HIF-1α; OCT-4 and VEGF can be regulated by both, context-dependent).
- CRISPR-Cas9 Knockout: Create single or double knockout cell lines. Validate by western blot and functional assays.
- Rescue Experiments: Transfect knockout cells with plasmid vectors expressing ODD-domain mutated HIF-α isoforms (resistant to degradation under normoxia) to confirm phenotype reversal. Always include an empty vector control.
Q4: My immunofluorescence for HIF-α shows unexpectedly high nuclear signal in normoxic controls. A: This is likely an artifact of fixation and permeabilization.
- Troubleshooting Steps:
- Fixation: Use fresh 4% PFA for 10-15 minutes at room temperature. Avoid over-fixation.
- Permeabilization: Titrate your detergent (Triton X-100, Tween-20). High concentrations can cause nuclear leakage and non-specific antibody binding.
- Antibody Validation: Include a no-primary-antibody control and a genuine hypoxic positive control on the same slide. Consider using a cell line with HIF-α knockout as a negative control.
- Blocking: Increase blocking time with serum from the secondary antibody host species (e.g., 5% normal goat serum for 1 hour).
Key Experimental Protocols
Protocol 1: Generating and Validating a Hypoxic Gradient in Multicellular Tumor Spheroids (MCTS)
- Method: Use the liquid overlay method (cells on agarose-coated plates) or bioprinting to form spheroids.
- Hypoxia Induction: Culture spheroids for 5-7 days until diameter exceeds 500 µm. Place in a modular incubator chamber flushed with a certified gas mixture (e.g., 1% O₂, 5% CO₂, balance N₂) for 24-48 hours.
- Validation:
- Add 100 µM pimonidazole to media for the final 2 hours of hypoxia.
- Fix spheroids, embed in OCT, and cryosection.
- Perform immunofluorescence for pimonidazole adducts and a perfusion marker (e.g., CD31 if co-cultured with endothelial cells).
- Quantify fluorescence intensity from periphery to core to map the gradient.
Protocol 2: Co-Immunoprecipitation (Co-IP) to Study HIF-α Interaction Partners in Hypoxia
- Purpose: To identify proteins interacting with HIF-1α/HIF-2α (e.g., p300/CBP, ARNT/HIF-1β).
- Detailed Steps:
- Lysis: Harvest hypoxic cells in NP-40 or RIPA lysis buffer supplemented with fresh protease/phosphatase inhibitors. Do not freeze-thaw lysates; proceed immediately.
- Pre-clearing: Incubate 500 µg lysate with 20 µL protein A/G beads for 30 minutes at 4°C. Pellet beads, keep supernatant.
- Immunoprecipitation: Incubate supernatant with 2-4 µg of anti-HIF-1α antibody (or IgG control) overnight at 4°C with gentle rotation.
- Capture: Add 30 µL protein A/G beads for 2 hours.
- Washing: Pellet beads, wash 4x with ice-cold lysis buffer.
- Elution: Elute bound proteins in 2X Laemmli buffer by heating at 95°C for 5 minutes.
- Analysis: Run eluate on SDS-PAGE. Probe by western blot for suspected interactors (e.g., p300, HIF-1β).
Summarized Quantitative Data
Table 1: Characteristic Features of HIF-α Isoforms in Solid Tumors
| Feature | HIF-1α | HIF-2α |
|---|---|---|
| Primary Regulation | Post-translational (PVDH degradation) & Transcriptional | Post-translational (PVDH degradation) & Transcriptional |
| Key Target Genes | CA9, BNIP3, GLUT1, PDK1 | OCT-4, VEGF, Cyclin D1, TGF-α |
| Common Tumor Context | Early-stage tumors, acute hypoxia | Advanced carcinomas, chronic hypoxia |
| Impact on Misfolding Stress | Upregulates chaperones (HSP70, GRP78); promotes autophagy via BNIP3. | Can promote ER stress adaptation; linked to aggressive phenotype. |
| Typical pO₂ Threshold for Stabilization | < 5% O₂ (~40 mmHg) | < 3% O₂ (~24 mmHg) |
Table 2: Common Reagents for Manipulating and Monitoring Hypoxia In Vitro
| Reagent | Mechanism of Action | Typical Working Concentration |
|---|---|---|
| Dimethyloxalylglycine (DMOG) | Competitive inhibitor of PHD enzymes, stabilizing HIF-α. | 0.5 - 1.0 mM |
| CoCl₂ (Cobalt Chloride) | Mimics hypoxia by displacing Fe²⁺ in PHDs, inhibiting their activity. | 100 - 200 µM |
| Deferoxamine (DFO) | Iron chelator, inhibits PHD activity by Fe²⁺ depletion. | 100 - 300 µM |
| Pimonidazole HCl | Forms protein adducts in hypoxic cells (pO₂ < 10 mmHg). | 100 µM (incubate 2-4h) |
| Roxadustat (FG-4592) | Clinical PHD inhibitor, stabilizes HIF-α. | 10 - 50 µM |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Example Product/Catalog # |
|---|---|---|
| Hypoxia Chamber | Creates a controlled low-oxygen environment for cell culture. | Billups-Rothenberg Modular Incubator Chamber |
| Portable Oxygen Meter | Validates O₂ levels inside chambers and workstations. | Extech DO600 Dissolved Oxygen Meter |
| Anti-HIF-1α Antibody (ChIP-grade) | For chromatin immunoprecipitation to identify HIF-1 binding sites. | Novus Biologicals NB100-479 |
| Anti-HIF-2α/EPAS1 Antibody | For specific detection of HIF-2α by western blot or IF. | Cell Signaling Technology #7096 |
| Pimonidazole HCl | Chemical probe for immunohistochemical detection of hypoxia. | Hypoxyprobe Kit (HP2-100Kit) |
| HIF-1α/HIF-2α siRNA Set | For isoform-specific gene knockdown experiments. | Santa Cruz Biotechnology sc-35561 & sc-35332 |
| HRE Reporter Lentivirus | For stable generation of hypoxia-sensing cell lines. | System Biosciences HRE-GFP Luciferase (LR012PA-1) |
| Proteasome Inhibitor (MG-132) | Stabilizes HIF-α proteins during cell lysis. | Sigma-Aldrich C2211 |
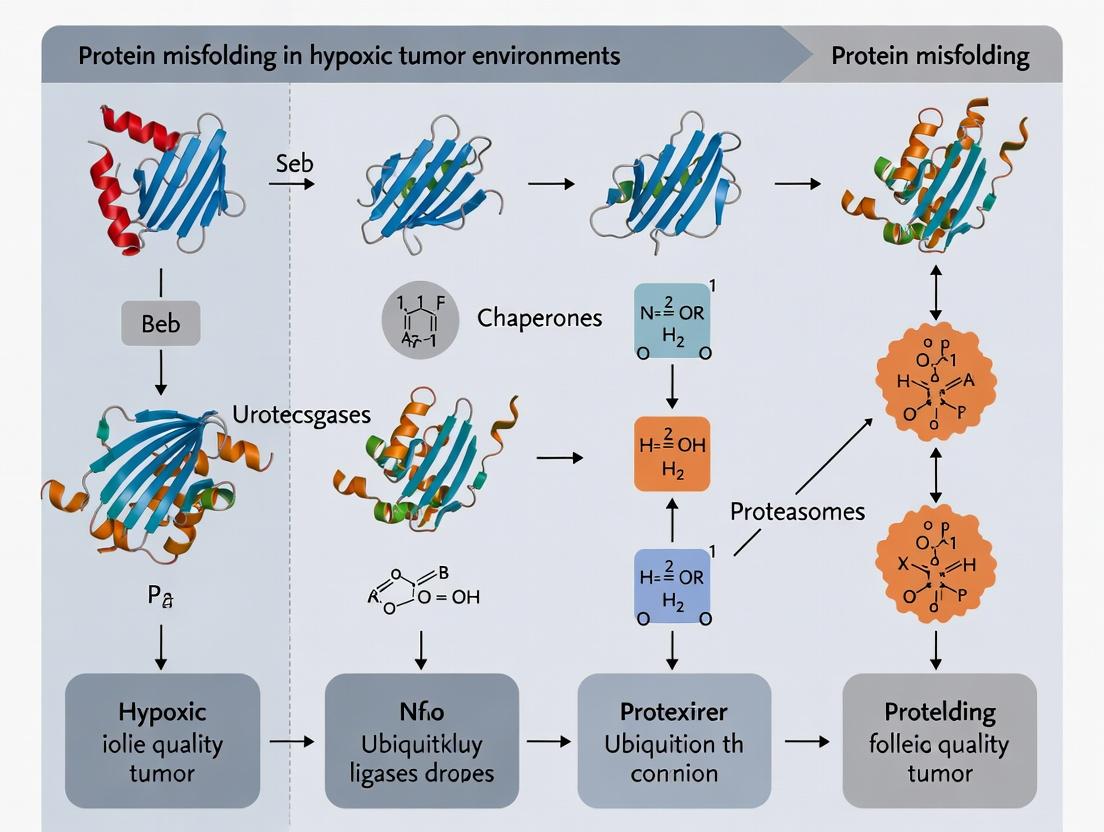
Pathway and Workflow Diagrams
Technical Support Center
Welcome to the ER Stress & Hypoxia Research Support Center. This resource provides troubleshooting guidance for common experimental challenges in studying protein folding and ER function in hypoxic environments, specifically within the context of Addressing protein misfolding in hypoxic tumor environments.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My hypoxia chamber (or hypoxia mimetic) isn't inducing consistent UPR marker expression across cell lines. What could be wrong? A: Inconsistent UPR induction is common. First, verify your hypoxia system. For chambers, ensure proper gas calibration (e.g., 1% O₂) and chamber seal integrity. For chemical mimetics like CoCl₂ or DFO, perform a dose-response (e.g., 50-400 µM CoCl₂, 100-300 µM DFO) and time-course (4-24h) to identify optimal conditions for each line, as sensitivity varies. Confirm hypoxia via HIF-1α western blot (stabilization peaks ~4-8h). Tumor cell lines with pre-adapted mutations may have attenuated UPR; consider using more physiologically relevant models like patient-derived organoids.
Q2: I'm not detecting PERK or IRE1α activation via phosphorylation, despite clear HIF-1α stabilization. What should I check? A: Phospho-specific antibodies are notoriously tricky. Ensure you are using positive controls (e.g., Thapsigargin or Tunicamycin for ER stress). Lyse cells in RIPA buffer with fresh phosphatase and protease inhibitors. Load ample protein (30-50 µg). For p-PERK (Thr980), run a longer gel to improve separation from its heavy chain. For p-IRE1α, consider an in vitro kinase assay as an alternative functional readout. Remember, chronic hypoxia may lead to adaptive dephosphorylation; measure downstream outputs like CHOP mRNA or XBP1 splicing.
Q3: My XBP1 splicing assay (RT-PCR) shows a faint or smeared product. How can I optimize it? A: XBP1 splicing is a key IRE1α output. Use high-quality RNA (RNase-free conditions). The PCR product difference is only 26bp. Use a high-resolution agarose gel (3-4%) or, preferably, capillary electrophoresis. Primers must flank the IRE1α cleavage site. Include a no-RT control to rule out genomic DNA contamination. For quantification, use qPCR with splice-specific probes or analyze gel band intensity with dedicated software. Consider that hypoxia may induce a slower, more nuanced splicing response compared to potent ER stress inducers.
Q4: When quantifying secreted proteins (e.g., VEGF) under hypoxia, my ELISA results are highly variable. How to improve consistency? A: Hypoxia dramatically alters secretion rates. Key steps: 1) Normalize carefully: Use cell count, total cellular protein, or a constitutively secreted reference protein (e.g., Clusterin) for normalization. 2) Conditioned media collection: Wash cells gently with warm PBS before adding fresh, serum-free (or low-serum) media for the hypoxia period to avoid serum protein interference. 3) Inhibit degradation: Include protease inhibitors in the collection media. 4) Concentrate samples if needed: Use centrifugal concentrators. Run technical duplicates/triplicates.
Experimental Protocols
Protocol 1: Assessing the Integrated ER Stress Response in Hypoxic Cells Objective: To simultaneously evaluate UPR arm activation and apoptotic commitment. Method:
- Hypoxia Treatment: Seed cells in 6-well plates. At 70% confluence, place in a pre-equilibrated hypoxia chamber (1% O₂, 5% CO₂, balance N₂) for desired timepoints (e.g., 8h, 16h, 24h). Include normoxic (21% O₂) and Thapsigargin (1µM, 6h) controls.
- Protein Extraction: Lyse cells directly in 1x Laemmli buffer to preserve phosphorylation states. Sonicate briefly to shear DNA, then boil for 5 min.
- Western Blotting: Run 30µg lysate on 10% SDS-PAGE gels. Transfer to PVDF. Probe with the following antibodies sequentially (after stripping): HIF-1α, p-PERK, total PERK, CHOP, BiP/GRP78, Cleaved Caspase-3, and β-Actin loading control.
- RNA Analysis (Parallel Sample): Extract RNA. Perform RT-qPCR for XBP1s, ATF4, CHOP, and GRP78. Use GAPDH for normalization.
Protocol 2: Monitoring ER Client Protein Secretion Efficiency Objective: To evaluate the impact of hypoxia on ER processing and secretion flux. Method (Pulse-Chase for a Model Secreted Protein):
- Starve and Pulse: Culture cells in 10cm dishes. Pre-equilibrate to normoxia or hypoxia (1% O₂) for 4h. Rinse with methionine/cysteine-free media. Incubate in this media (hypoxic/normoxic) for 30 min. Add EasyTag EXPRESS 35S Protein Labeling Mix (100-200 µCi/mL) for 20 min ("pulse").
- Chase: Aspirate labeling media, wash, and add complete media with excess unlabeled methionine/cysteine. Return plates to respective conditions. Harvest cells and media at chase timepoints (e.g., 0, 30, 60, 120 min).
- Immunoprecipitation: At each timepoint, collect media (with protease inhibitors) and lyse cells. Immunoprecipitate your protein of interest (e.g., a monoclonal antibody against your model client) from both lysate (intracellular) and media (secreted) fractions.
- Analysis: Resolve immunoprecipitates by SDS-PAGE, dry gel, and expose to a phosphor screen. Quantify band intensity for intracellular vs. secreted protein over time to calculate secretion efficiency and rate.
Table 1: Common Hypoxia Mimetics and Their Effects on ER Stress Markers
| Mimetic | Typical Working Concentration | Mechanism | Key ER Stress/UPR Outputs (Timeframe) | Notes |
|---|---|---|---|---|
| Cobalt Chloride (CoCl₂) | 100 - 300 µM | Inhibits HIF-α prolyl hydroxylases | BiP ↑ (8-24h), CHOP ↑ (12-24h), XBP1 splicing ↑ (4-12h) | Can induce cytotoxicity independent of HIF; use dose-response. |
| Desferrioxamine (DFO) | 100 - 300 µM | Iron chelator, inhibits PHDs | HIF-1α stabilization (2-4h), moderate BiP/CHOP induction (12h+) | Slower, more gradual inducer than CoCl₂. |
| Dimethyloxalylglycine (DMOG) | 0.5 - 1 mM | Competitive 2-OG antagonist, inhibits PHDs | Broad HIF target activation, mild UPR induction. | Pan-hydroxylase inhibitor; effects are not specific to HIF-PHDs. |
Table 2: Quantifying UPR Activation in Tumor Cell Lines Under 1% O₂
| Cell Line | HIF-1α Peak Stabilization | Significant p-IRE1α Detection | CHOP Protein Induction Threshold | Notable Adaptive Response |
|---|---|---|---|---|
| MCF-7 (Breast Ca) | 4-6 hours | 8-12 hours | >16 hours | Strong ATF6 cleavage; resistant to apoptosis. |
| U87 (Glioblastoma) | 2-4 hours | 6-8 hours | 12 hours | High basal GRP78; PERK pathway dominant. |
| PC-3 (Prostate Ca) | 4-8 hours | Weak/Variable | >24 hours | Low UPR; relies on autophagy for hypoxia survival. |
Pathway & Workflow Diagrams
Title: Hypoxia-Induced ER Stress and UPR Signaling Pathways
Title: Pulse-Chase Workflow for Secretion Analysis Under Hypoxia
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Hypoxia/ER Research |
|---|---|
| Hypoxia Chamber / Workstation | Provides precise, controlled low-oxygen environment (e.g., 0.1-5% O₂) for physiologically relevant cell culture. Essential for chronic hypoxia studies. |
| Chemical Hypoxia Mimetics (CoCl₂, DFO, DMOG) | Induces HIF stabilization in standard incubators. Useful for screening but requires validation against true hypoxia due to off-target effects. |
| Thapsigargin | SERCA pump inhibitor; induces potent, rapid ER stress by depleting luminal Ca²⁺. Critical positive control for UPR activation assays. |
| Tunicamycin | N-linked glycosylation inhibitor; induces ER stress by causing accumulation of unglycosylated proteins. Positive control for UPR. |
| Phospho-Specific Antibodies (p-PERK, p-eIF2α) | Detect activation of UPR sensor kinases. Crucial for mechanistic studies. Require careful protocol optimization. |
| HIF-1α Antibody | Western blot probe to confirm hypoxia induction. Distinguish between stabilized (hypoxic) and basal (normoxic, often undetectable) levels. |
| XBP1 Splicing Primers | For RT-PCR detection of IRE1α endonuclease activity. Gold-standard functional readout for the IRE1α-XBP1 arm. |
| 4μ8C (IRE1α RNase Inhibitor) | Pharmacologic inhibitor of IRE1α's RNase domain. Used to dissect the role of XBP1 splicing vs. RIDD in cellular responses. |
| ISRIB (Integrated Stress Response Inhibitor) | Reverses p-eIF2α-mediated translation arrest. Used to test the functional role of PERK/eIF2α signaling in hypoxia adaptation. |
| 35S Methionine/Cysteine (EasyTag) | Radioactive amino acids for metabolic pulse-chase labeling to dynamically track protein synthesis, ER processing, and secretion rates. |
| ER-Tracker Dyes (Live Cell) | Fluorescent dyes (e.g., ER-Tracker Green) that selectively stain the ER in live cells. Can monitor ER morphology changes under hypoxia. |
| CHOP/Luciferase Reporter Plasmid | Allows dynamic, quantifiable reporting of the terminal, pro-apoptotic UPR output. Useful for high-throughput drug screening. |
Technical Support Center: Troubleshooting UPR Experiments in Hypoxic Cancer Research
FAQs & Troubleshooting Guides
Q1: In our hypoxic chamber experiments (0.5-1% O₂), we are not detecting increased phosphorylation of PERK (p-PERK) via western blot in our pancreatic cancer cell line, despite clear induction of BiP/GRP78. What could be the issue?
A: This is a common issue. Potential causes and solutions:
- Antibody Specificity: The p-PERK antibody (Thr980) may not be suitable for your specific cell line or may require different fixation/lysis conditions. Solution: Validate with a PERK kinase activity assay (e.g., in vitro kinase assay using recombinant eIF2α as substrate) as a functional readout alongside western blot.
- Rapid Feedback & Phosphatase Activity: PERK autophosphorylation can be transient. Hypoxia might also regulate specific phosphatases. Solution: Treat cells with a phosphatase inhibitor (e.g., calyculin A, 10 nM for 30 min) prior to lysis. Shorten hypoxic exposure times (e.g., check at 30 min, 2h, 4h).
- Alternative Lysis Buffer: Use a rigorous RIPA buffer supplemented with 1x protease and phosphatase inhibitor cocktails. Ensure quick lysis while cells are still in the hypoxic workstation if possible.
Q2: Our ATF6 cleavage assay (via western blot for the 50 kDa N-terminal fragment) shows inconsistent results between replicates during hypoxia/reoxygenation cycles. How can we improve reliability?
A: ATF6 processing is highly sensitive to ER stress intensity and timing.
- Protocol Refinement: Use a positive control (e.g., 5 μg/mL Tunicamycin for 4h) in every experiment. For hypoxia, ensure precise and rapid harvesting. The cleaved fragment is nuclear; consider preparing nuclear extracts using a commercial kit instead of whole-cell lysates to enrich the signal.
- Timing is Critical: Perform a detailed time course (e.g., 1h, 2h, 4h, 8h of hypoxia and 1h after reoxygenation). The cleaved fragment may appear only in a narrow window.
- Blocking Step: Use 5% non-fat dry milk in TBST for blocking and antibody incubation to reduce background.
Q3: When measuring IRE1α RNase activity via XBP1 splicing, our RT-PCR products show smearing or multiple bands. What are the optimal conditions?
A: This indicates suboptimal PCR conditions or RNA degradation.
- Updated Protocol:
- RNA Isolation: Use a column-based method with on-column DNase I treatment.
- RT-PCR: Use gene-specific primers for XBP1 and a high-fidelity polymerase.
- PCR Cycle Optimization: Reduce cycle number (25-28 cycles) to stay in the linear amplification range.
- Restriction Digest Confirmation: Digest PCR products with PstI restriction enzyme. Unspliced XBP1 (uXBP1) has a PstI site that is lost upon splicing (sXBP1). This clarifies ambiguous bands.
Q4: In our 3D spheroid model of hypoxic tumors, pharmacological inhibition of IRE1 (e.g., with 4μ8C) does not recapitulate the growth phenotype seen in IRE1-knockdown cells. Why?
A: This highlights a key technical consideration.
- Compound Penetration: The inhibitor may not penetrate the core of the spheroid effectively. Solution: Pre-treat dissociated cells for 24h before spheroid formation, or use a higher concentration validated for 3D culture (e.g., 10-20 μM 4μ8C). Always measure a direct output (e.g., XBP1 splicing) in the treated spheroids to confirm target engagement.
- Off-target Effects: Genetic knockdown may have effects distinct from acute pharmacological inhibition. Consider using multiple, structurally distinct inhibitors (e.g., MKC-3946) to confirm phenotype.
Key Quantitative Data in UPR-Hypoxia Cancer Studies
Table 1: Common Hypoxic Conditions & UPR Activation Timelines in Cancer Cell Models
| Cell Line/Tumor Type | Hypoxic Condition | Key UPR Marker Activated | Time to Peak Activation | Typical Functional Readout |
|---|---|---|---|---|
| Glioblastoma (U87MG) | 1% O₂ | p-PERK, ATF4 | 4-8 hours | Increased cell viability assay (MTT) |
| Breast Cancer (MCF-7) | 0.5% O₂ | XBP1 splicing, BiP | 2-4 hours | Spheroid formation assay |
| Colorectal Carcinoma (HCT116) | 0.1% O₂ | ATF6 cleavage, CHOP | 8-12 hours | Annexin V/PI flow cytometry |
| Pancreatic Cancer (MiaPaCa-2) | 0.5% O₂, Cyclic (8h on/16h off) | All three arms | 4h (IRE1/PERK), 8h (ATF6) | Invasion assay (Matrigel) |
Table 2: Common Pharmacologic Modulators of UPR in Hypoxic Research
| Reagent | Target | Common Working Concentration | Primary Effect | Note for Hypoxia Experiments |
|---|---|---|---|---|
| Tunicamycin | N-linked glycosylation | 1-5 μg/mL | Potent general ER stress inducer | Use as a positive control, not hypoxic-specific. |
| Thapsigargin | SERCA pump | 0.1-1 μM | ER calcium depletion, UPR induction | Strong PERK/ATF6 activator. |
| 4μ8C | IRE1 RNase domain | 10-100 μM | Inhibits XBP1 splicing | Check solubility in prolonged hypoxic cultures. |
| GSK2606414 | PERK kinase | 0.1-1 μM | Inhibits eIF2α phosphorylation | Can induce compensatory IRE1 activation. |
| Ceapins | ATF6 | 1-10 μM | Inhibits ATF6 cleavage/processing | Useful for isolating ATF6-specific functions. |
| ISRIB | eIF2B | 100-200 nM | Reverses p-eIF2α-mediated translation halt | Rescues PERK effects; tests translational recovery. |
Detailed Experimental Protocols
Protocol 1: Assessing IRE1-XBP1 Activation in Hypoxic Spheroids
- Objective: To measure the adaptive IRE1 arm in a 3D, hypoxic tumor model.
- Materials: Ultra-low attachment plates, hypoxia chamber (0.5% O₂, 5% CO₂, 94.5% N₂), TRIzol reagent, XBP1 primers.
- Steps:
- Spheroid Formation: Seed 2000 cells/well in a 96-well U-bottom plate. Centrifuge at 300g for 3 min. Incubate normoxically for 72h to form compact spheroids.
- Hypoxic Treatment: Place the entire plate in a pre-equilibrated hypoxic chamber for desired times (e.g., 24h, 48h). Include normoxic controls in a separate incubator.
- RNA Extraction: Carefully aspirate medium. Directly add 500μL TRIzol to 3-5 pooled spheroids per condition. Homogenize by pipetting. Proceed with standard RNA isolation.
- XBP1 Splicing Assay: Perform RT-PCR using primers: F: 5'-CCTGGTTGCTGAAGAGGAGG-3', R: 5'-CCATGGGGAGATGTTCTGGAG-3'. PCR product: uXBP1=289bp, sXBP1=263bp. Run on a 3% agarose gel.
- Validation: Digest products with PstI (37°C, 2h) to confirm splicing.
Protocol 2: Monitoring PERK-eIF2α-ATF4 Axis via Immunoblotting
- Objective: To analyze the translational regulatory arm during acute hypoxia.
- Materials: Hypoxia workstation, RIPA buffer + phosphatase inhibitors, antibodies for p-eIF2α (S51), total eIF2α, ATF4.
- Steps:
- Treatment: Culture adherent cells in dishes. Place dishes in the hypoxia workstation (0.1-1% O₂). For time points <4h, perform lysis inside the workstation if possible.
- Rapid Lysis: At each time point, quickly move dishes to ice, aspirate medium, and add 150μL of ice-cold RIPA buffer with inhibitors. Scrape cells on ice.
- Sample Preparation: Sonicate lysates briefly (10 sec), centrifuge at 14,000g for 15 min at 4°C. Collect supernatant.
- Western Blot: Load 20-30μg protein. Use 10% Bis-Tris gel. Transfer to PVDF membrane. Block with 5% BSA in TBST for 1h. Incubate with primary antibodies (p-eIF2α 1:1000, ATF4 1:500) in blocking buffer overnight at 4°C.
- Quantification: Normalize p-eIF2α signal to total eIF2α, and ATF4 to a loading control (e.g., β-Actin). Compare fold-change over normoxic control.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for UPR-Hypoxia Research
| Reagent / Kit | Supplier Examples | Function in UPR/Hypoxia Research |
|---|---|---|
| Hypoxia Chamber / Workstation | Baker, BioSpherix | Provides precise, regulated low-oxygen environment for cell culture. |
| pO₂/Hypoxia Probe (e.g., Image-iT) | Thermo Fisher | Live-cell imaging of intracellular oxygen levels. |
| Phospho-specific IRE1 (S724) Antibody | Abcam, Cell Signaling | Detects activated IRE1 via phosphorylation. |
| ATF6 (N-terminal) Antibody | BioLegend, Novus | Specifically detects the cleaved, active fragment of ATF6. |
| XBP1 Splicing RT-PCR Kit | Takara, Bio-Rad | All-in-one solution for detecting XBP1u and XBP1s mRNA. |
| ER-Tracker Green Dye | Thermo Fisher | Live-cell staining of the endoplasmic reticulum morphology. |
| CHOP/GADD153 Reporter Cell Line | Various (e.g., ATCC) | Stable reporter for monitoring sustained ER stress/PERK pathway output. |
| Proteostat Aggresome Detection Kit | Enzo Life Sciences | Detects protein aggregates formed due to misfolding in hypoxia. |
| Viability/Cytotoxicity Kit (Multi-parameter) | Promega (CellTiter-Glo) | Assess cell health under hypoxic ER stress; preferable to MTT in low metabolism. |
Visualizations
Technical Support Center
Troubleshooting Guides & FAQs
Q1: My hypoxic chamber (e.g., InvivO2 400) is not maintaining the target low oxygen tension (e.g., 0.5-1% O₂). What could be wrong? A: Verify the following:
- Gas Supply: Ensure the N₂/CO₂ gas tank is not empty and the regulator is functioning. Check all tubing connections for leaks using a soap solution.
- Sensor Calibration: The oxygen sensor requires regular calibration. Perform a two-point calibration (0% and 21% O₂) using certified calibration gas or an anaerobic chamber (0%) and ambient air (21%).
- Seal Integrity: Inspect the chamber gasket for cracks or deformities. Apply a thin layer of silicone grease if recommended by the manufacturer. Ensure the door is closed securely.
- Catalyst: If using a palladium-based catalyst to scavenge oxygen, ensure it is not exhausted (indicated by a color change). Reactivate or replace as needed.
Q2: I observe high cell death in my control normoxic cultures during prolonged hypoxia-mimicking drug (e.g., CoCl₂, DFO) treatment. How can I optimize the dose? A: This indicates drug toxicity. Perform a dose-response and time-course assay.
- Prepare a serial dilution of the hypoxia mimetic (e.g., CoCl₂ from 50 µM to 400 µM).
- Treat cells for 4, 12, 24, and 48 hours.
- Assess viability using an ATP-based assay (e.g., CellTiter-Glo) and a membrane integrity assay (e.g., LDH release) to distinguish cytotoxic from cytostatic effects.
- Use the highest dose and longest time that maintains >80% viability in normoxia for your specific cell line. Common optimal ranges: CoCl₂: 100-200 µM; DFO: 100-300 µM.
Q3: My filter trap assay for protein aggregates shows a high background signal in normoxic samples. How can I reduce non-specific binding? A: High background is often due to inadequate washing or lysis conditions.
- Lysis Buffer Optimization: Include 1% Triton X-100 or 1% N-Lauroylsarcosine in your RIPA buffer. Do not use SDS at this stage as it will dissolve aggregates.
- Benzonase Treatment: Add Benzonase (25 U/mL) to the lysate and incubate for 30 min at 37°C post-lysis to degrade nucleic acids that can trap non-specifically.
- Washing Stringency: After sample filtration, wash the membrane 5-7 times with 500 µL of lysis buffer containing 1% Triton X-100. Use a syringe for controlled, gentle pressure.
- Blocking: Block the membrane with 5% non-fat milk in TBS-T for 1 hour at room temperature before antibody incubation.
Q4: Immunofluorescence for protein aggregates (e.g., using p62/SQSTM1 or ubiquitin antibodies) shows diffuse staining instead of puncta. What are possible causes? A: This suggests aggregates are not forming or are being degraded.
- Hypoxia Duration: Protein aggregation is time-dependent. Extend hypoxia treatment to 48-72 hours.
- Proteasome Inhibition: Co-treat with a low dose of proteasome inhibitor (e.g., MG-132, 5 µM) for the final 6-8 hours of hypoxia to prevent aggregate clearance via the UPS.
- Fixation: Use fresh, ice-cold 100% methanol for 10 min at -20°C instead of PFA. Methanol better preserves protein structures and aggregate morphology.
- Antibody Validation: Ensure your antibody is validated for IF. Use a positive control (e.g., cells treated with proteasome inhibitor + oxidative stress inducer).
Q5: My Thioflavin T (ThT) aggregation kinetics assay in hypoxic cell lysates shows no fluorescence increase over time. A: ThT requires specific conditions for binding to amyloid-like aggregates.
- pH Check: ThT fluorescence is optimal at pH >7.0. Ensure your aggregation assay buffer (e.g., PBS or Hepes) is at pH 7.4-8.5.
- Aggregation Induction: Hypoxia-induced aggregates may be amorphous. Supplement lysates with 2M urea or 0.01% SDS to induce partial denaturation and expose amyloidogenic cores.
- Dye Concentration: The final ThT concentration should be 20-50 µM.
- Control: Include a positive control (e.g., pre-formed Aβ42 fibrils) to confirm ThT reactivity.
Key Experimental Protocols
Protocol 1: Induction and Validation of Cellular Hypoxia Objective: To establish a stable hypoxic environment for tumor cells and validate the hypoxic response. Method:
- Seed cells in culture dishes suitable for your hypoxic chamber.
- Place dishes in a modular hypoxic chamber (e.g., Billups-Rothenberg).
- Flush the chamber for 10-15 minutes with a pre-mixed gas containing 1% O₂, 5% CO₂, balanced with N₂.
- Seal the chamber and incubate at 37°C for desired durations (typically 24-72h).
- Validation: Harvest a parallel sample for immunoblotting of HIF-1α (Cat# 36169, Cell Signaling Technology). Normoxic samples should show minimal HIF-1α, while hypoxic samples should show a strong band at ~120 kDa.
Protocol 2: Sequential Detergent Extraction for Protein Aggregates Objective: To fractionate and isolate insoluble protein aggregates from cells. Method:
- Lyse cell pellets in Triton X-100 Buffer (50 mM Tris pH 7.5, 150 mM NaCl, 1% Triton X-100, 1x protease/phosphatase inhibitors) on ice for 30 min.
- Centrifuge at 16,000 x g for 20 min at 4°C.
- Collect supernatant as the "Soluble Fraction".
- Wash the pellet gently with 1 mL of Triton X-100 Buffer and centrifuge again. Discard wash.
- Resuspend the pellet in SDS-Urea Buffer (50 mM Tris pH 7.5, 1% SDS, 6M Urea) and sonicate briefly (3 x 5 sec pulses).
- Centrifuge at 16,000 x g for 20 min at 22°C.
- Collect supernatant as the "Insoluble/Aggregate-Enriched Fraction".
- Analyze both fractions by immunoblot for your protein of interest and an aggregate marker like p62.
Protocol 3: Filter Trap Assay for Insoluble Aggregates Objective: To quantify the amount of large, insoluble protein aggregates. Method:
- Prepare cell lysates in a 1% Sarkosyl-containing buffer (do not sonicate).
- Dilute protein lysates to equal concentrations (e.g., 1 µg/µL).
- Assemble a dot-blot apparatus with a 0.22 µm cellulose acetate membrane pre-wet in PBS.
- Load 100 µL of diluted lysate per well. Apply gentle vacuum.
- Wash each well 5x with 200 µL of PBS containing 1% Sarkosyl.
- Disassemble, block the membrane (5% milk), and probe with primary antibody overnight at 4°C.
- Detect using chemiluminescence. The signal intensity correlates with aggregate load.
Table 1: Common Hypoxia Models & Their Effects on Protein Aggregation Markers
| Model | O₂ Concentration | Treatment Duration | Key Molecular Readout (Fold Change vs. Normoxia) | Common Cell Lines Used |
|---|---|---|---|---|
| Gas-Controlled Chamber | 0.5 - 1% O₂ | 24 - 72 h | HIF-1α: >10x | U87-MG, HCT116, MDA-MB-231 |
| Chemical Mimetic (CoCl₂) | N/A (Ambient) | 24 - 48 h | HIF-1α: 5-8x; p62: 2-4x | HeLa, HEK293, MCF-7 |
| Chemical Mimetic (DFO) | N/A (Ambient) | 24 - 48 h | HIF-1α: 4-7x; LC3-II: 2-3x | PC3, A549, HepG2 |
| Three-Dimensional Spheroids | Core: <0.5% O₂ | 5 - 7 days | HIF-1α: >20x; Ubiquitin: 3-5x | Patient-derived organoids |
Table 2: Reagents for Detecting & Quantifying Protein Aggregates
| Assay | Target | Key Reagent (Example) | Function & Rationale |
|---|---|---|---|
| Immunoblot (Sarkosyl Fractionation) | Insoluble Protein | N-Lauroylsarcosine (Sarkosyl) | Ionic detergent that solubilizes membranes and monomers but leaves large aggregates insoluble for separation by centrifugation. |
| Filter Trap Assay | Large Aggregates | Cellulose Acetate Membrane (0.2 µm pore) | Physically traps aggregates >0.2 µm while allowing monomers to pass through, enabling specific detection of large complexes. |
| Immunofluorescence | Aggregate Morphology | Proteasome Inhibitor (MG-132) | Blocks degradation of ubiquitinated proteins by the proteasome, allowing visualization of accumulating aggregates. |
| Fluorescent Dye Binding | Amyloid-like Structure | Thioflavin T (ThT) | Binds to cross-beta-sheet structures common in amyloid fibrils, resulting in a fluorescent signal shift (Ex/Em ~440/482 nm). |
| Proximity Ligation Assay (PLA) | Protein-Protein Interactions in Aggregates | Duolink PLA Probes | Detects close proximity (<40 nm) between two proteins (e.g., p62 and ubiquitin), visualizing early aggregation events in situ. |
Diagrams
Diagram 1: Hypoxia-Induced Aggregate Formation Pathway
Diagram 2: Experimental Workflow for Aggregate Analysis
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application in Hypoxia/Aggregation Research |
|---|---|
| Hypoxia Chamber (Modular) | Creates a physiologically relevant low-oxygen environment (0.1-2% O₂) for cell culture. Essential for studying HIF signaling and chronic hypoxic stress. |
| Hypoxia-Inducible Factor (HIF) Stabilizers (CoCl₂, DFO) | Chemical mimetics that inhibit HIF-1α prolyl hydroxylases (PHDs), leading to HIF stabilization under normoxic conditions. Useful for rapid screening. |
| Proteasome Inhibitor (MG-132, Bortezomib) | Blocks the 26S proteasome, preventing degradation of ubiquitinated misfolded proteins. Used to "trap" and amplify aggregation signals. |
| Autophagy Inhibitor (Chloroquine, Bafilomycin A1) | Inhibits autophagic flux by raising lysosomal pH or blocking fusion. Used to determine the role of autophagy in aggregate clearance under hypoxia. |
| Sarkosyl (N-Lauroylsarcosine) | Ionic detergent used in sequential extraction protocols to solubilize cellular components while leaving large protein aggregates insoluble for analysis. |
| Aggregate-Specific Dyes (Thioflavin T, Proteostat) | Fluorescent dyes that selectively bind to protein aggregates with cross-β-sheet structure (ThT) or general aggregates (Proteostat), enabling detection in vitro and in cells. |
| p62/SQSTM1 Antibody | Key marker for protein aggregates. p62 binds ubiquitinated proteins and targets them to autophagosomes; its accumulation indicates impaired aggregate clearance. |
| Benzonase Nuclease | Degrades DNA/RNA in cell lysates to prevent nucleic acid-mediated clogging of membranes in filter trap assays and reduce non-specific antibody binding. |
| Proximity Ligation Assay (PLA) Kit | Amplifies signal from two proximal (<40 nm) proteins, allowing visualization of specific protein-protein interactions within aggregates (e.g., mutant p53-ubiquitin) via microscopy. |
| HIF-1α ELISA Kit | Provides a quantitative, high-throughput method to validate hypoxia induction and measure HIF-1α protein levels across many samples. |
Technical Support Center: Experimental Troubleshooting
This technical support center is framed within a thesis on Addressing protein misfolding in hypoxic tumor environments. It provides solutions to common experimental challenges.
FAQ & Troubleshooting Guides
Q1: In our hypoxia-mimetic experiments using CoCl₂, we observe high cell death, confounding our analysis of the unfolded protein response (UPR). How can we titrate the stress to study adaptive UPR rather than apoptosis?
A: Excessive CoCl₂ concentration is a common issue. The goal is to induce sustained ER stress without triggering immediate apoptosis.
- Solution: Perform a dose-response (50-300 µM) and time-course (4-24h) experiment. Monitor adaptive vs. apoptotic UPR markers simultaneously.
- Adaptive UPR Markers: Phospho-eIF2α, BiP/GRP78, XBP1 splicing (sXBP1).
- Apoptotic UPR Markers: CHOP, cleaved caspase-3, phospho-JNK.
- Protocol: Seed cells in 12-well plates. Treat with CoCl₂ (e.g., 0, 100, 150, 200 µM) for 8h and 16h. Perform Western blotting for the markers above. The optimal condition is the lowest concentration/timepoint yielding strong adaptive markers with minimal apoptotic markers.
Q2: Our immunofluorescence for BiP/GRP78 in hypoxic cells shows weak and diffuse signal, making it difficult to visualize ER localization and stress. What are the best fixation and staining practices?
A: Poor signal can stem from suboptimal fixation or antibody penetration.
- Solution: Use fresh, ice-cold methanol fixation for ER-resident proteins.
- Protocol:
- Culture cells on chamber slides under hypoxia (1% O₂) or CoCl₂ treatment.
- Aspirate media, rinse gently with PBS.
- Fix with 100% ice-cold methanol for 10 minutes at -20°C.
- Permeabilize and block with 0.1% Triton X-100, 5% BSA in PBS for 1 hour.
- Incubate with primary anti-BiP antibody (1:200 in blocking buffer) overnight at 4°C.
- Use a highly cross-adsorbed secondary antibody (e.g., Alexa Fluor 568 or 647) at 1:500 for 1h at RT. Include ER-Tracker Green as a co-stain for validation.
- Mount and image using a confocal microscope.
Q3: When assessing XBP1 splicing as a UPR marker via RT-PCR, our gels often show smeared bands or poor separation of unspliced (uXBP1) and spliced (sXBP1) variants. How can we improve resolution?
A: This is critical for accurately measuring IRE1α activity.
- Solution: Optimize PCR cycle number and use a high-resolution agarose gel.
- Protocol: Extract total RNA from stressed cells. Use primers flanking the XBP1 splice site.
- Primers (Human): F: 5′-AAACAGAGTAGCAGCTCAGACTGC-3′, R: 5′-TCCTTCTGGGTAGACCTCTGGGAG-3′.
- PCR Cycles: Limit to 28-30 cycles to prevent plateau-phase smearing.
- Gel: Use a 3-3.5% high-resolution agarose gel (e.g., MetaPhor agarose) in 0.5x TBE buffer, run at 100V for 90 minutes. sXBP1 is 26bp shorter than uXBP1.
Q4: Our experiments with proteasome inhibitors (e.g., MG-132) to induce proteostatic stress lead to rapid and complete cell death, preventing study of downstream pro-tumorigenic signaling. What alternatives exist?
A: MG-132 is a potent pan-proteasome inhibitor. Consider subtler or specific perturbations.
- Solution: Use lower doses, shorter pulses, or inhibit specific proteasome subunits or regulatory particles. Alternatively, induce protein misfolding directly.
- Protocol - Tunicamycin Pulse:
- Treat cells with a low dose of Tunicamycin (0.5 - 2 µg/mL), a glycosylation inhibitor that induces ER protein misfolding.
- Pulse for 2-4 hours, then wash out and replace with fresh media.
- Assay for downstream effects (e.g., VEGF secretion, NF-κB activation, EMT markers) at 24, 48, and 72h post-stress initiation. This models a recoverable stress event that may mimic tumor microenvironment conditions.
Table 1: Impact of Hypoxia-Induced Proteostatic Stress on Key Tumorigenic Parameters
| Tumorigenic Process | Experimental Model | Key Metric Change vs. Normoxia | Proposed Primary UPR Arm Mediating Effect |
|---|---|---|---|
| Angiogenesis | Breast Cancer Xenografts (Hypoxic) | VEGF secretion ↑ 3.5-fold | PERK/p-eIF2α/ATF4 |
| Metastasis (Invasion) | Melanoma Cells (CoCl₂, 150µM, 24h) | Matrigel Invasion ↑ 220% | IRE1α/XBP1s |
| Therapy Resistance (Cisplatin) | NSCLC Cells (1% O₂, 48h) | IC₅₀ for Cisplatin ↑ 4.2-fold | PERK & IRE1α (Synergistic) |
| Autophagy Flux | Glioblastoma Cells (DFO, 100µM, 12h) | LC3-II/I ratio ↑ 5.1-fold; p62 degradation ↑ 80% | PERK/ATF4/CHOP |
| EMT Induction | Prostate Cancer Cells (Hypoxia 0.5% O₂, 72h) | E-cadherin ↓ 90%; Vimentin ↑ 8-fold | IRE1α/XBP1s & ATF6 |
Detailed Experimental Protocol: Assessing UPR-Mediated Angiogenic Factor Secretion
Title: Protocol for Linking Hypoxic UPR to Angiogenesis In Vitro. Objective: To quantify the secretion of angiogenesis-related factors from tumor cells following hypoxic proteostatic stress and identify the mediating UPR pathway. Materials: See "Research Reagent Solutions" below. Procedure:
- Cell Preparation: Seed triple-negative breast cancer cells (e.g., MDA-MB-231) in 6-well plates (2.5 x 10⁵ cells/well) in complete growth medium. Incubate overnight.
- Hypoxic Stress & Pharmacological Inhibition: Pre-treat cells for 1h with:
- Group 1: DMSO vehicle control.
- Group 2: GSK2606414 (PERKi, 1 µM).
- Group 3: 4µ8C (IRE1α RNase inhibitor, 50 µM).
- Group 4: AEBSF (ATF6 inhibitor, 100 µM).
- Induce Hypoxia: Transfer all plates to a hypoxic chamber (1% O₂, 5% CO₂, 37°C) for 24 hours. Maintain inhibitors in media.
- Conditioned Media Collection: After 24h, collect media from each well. Centrifuge at 1000xg for 5 min to remove cell debris. Aliquot and store supernatant at -80°C.
- Cell Lysate Collection: Lyse cells in RIPA buffer for Western blot validation of UPR inhibition (p-eIF2α for PERKi, XBP1s for 4µ8C, cleaved ATF6 for AEBSF).
- Angiogenic Factor Quantification: Use a multiplex ELISA (e.g., Luminex) or individual ELISAs to measure concentrations of VEGF, IL-6, IL-8, and PGE2 in the conditioned media. Normalize data to total cellular protein from the lysate.
- Data Analysis: Compare factor secretion in hypoxic DMSO vs. normoxic control (baseline), and then assess the reduction caused by each UPR inhibitor.
Signaling Pathway & Experimental Workflow Diagrams
Title: UPR Signaling in Hypoxic Tumors Links Stress to Aggressive Traits
Title: Workflow: Measuring UPR-Driven Angiogenic Secretion
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Hypoxic Proteostasis Experiments
| Reagent / Material | Function & Application in Research | Example Catalog # / Vendor |
|---|---|---|
| Cobalt(II) Chloride Hexahydrate (CoCl₂) | Chemical hypoxia mimetic; stabilizes HIF-1α and induces ER stress. Used for rapid, reproducible stress induction. | 232696 / Sigma-Aldrich |
| GSK2606414 | Potent and selective PERK inhibitor. Used to dissect the role of the PERK-eIF2α-ATF4 arm of the UPR. | 1338810-24-5 / Cayman Chemical |
| 4µ8C | IRE1α RNase domain inhibitor. Blocks XBP1 splicing and RIDD, used to probe IRE1α-specific signaling. | 14003-96-4 / Tocris Bioscience |
| AEBSF Hydrochloride | Serine protease inhibitor that blocks ATF6 cleavage/activation. Used to inhibit the ATF6 arm. | 30827-99-7 / MedChemExpress |
| Human VEGF Quantikine ELISA Kit | Gold-standard immunoassay for precise quantification of VEGF-A in cell culture supernatants. | DVE00 / R&D Systems |
| ER-Tracker Green (BODIPY FL Glibenclamide) | Live-cell fluorescent dye that selectively labels the endoplasmic reticulum. For IF/confocal validation. | E34251 / Thermo Fisher |
| MetaPhor Agarose | High-resolution agarose for optimal separation of similar-length DNA fragments (e.g., uXBP1 vs. sXBP1). | 50181 / Lonza |
| Hypoxia Chamber / Workstation | Controlled atmosphere chamber (e.g., 0.1-5% O₂) for physiologically relevant hypoxic cell culture. | C-274 / Baker Ruskinn |
Tools and Techniques: Modeling Hypoxic Misfolding and Developing Targeted Interventions
Technical Support Center: Troubleshooting & FAQs
FAQ Context: These questions and answers are designed to support researchers in the field of Addressing protein misfolding in hypoxic tumor environments. They address practical experimental hurdles encountered when modeling hypoxia to study ER stress, unfolded protein response (UPR), and protein aggregation.
Troubleshooting Guides
Topic 1: Hypoxic Chamber Systems
- Q1: Our tri-gas incubator maintains the correct low O₂ percentage (e.g., 1%), but our HIF-1α western blot results are inconsistent. What could be wrong?
- A: Verify chamber equilibration time. After opening, the chamber can take >30 minutes to re-stabilize at the set O₂ level. Place a standalone O₂ sensor inside your culture plate to monitor the actual cell-level O₂ tension. Ensure the incubator’s CO₂ and temperature sensors are calibrated, as fluctuations here affect medium pH and cell metabolism, confounding hypoxic responses.
- Q2: We observe increased cell death in our control (normoxic) plates when a hypoxic run is ongoing in the same incubator. Is there cross-contamination of gases?
- A: This indicates a seal integrity failure in the chamber. Check the gaskets and door seal for cracks. Use an incubator exclusively for hypoxic work if possible. Alternatively, use separate, self-contained modular chambers (e.g., C-chambers) for hypoxic and normoxic samples to prevent gas exchange.
Topic 2: Chemical Hypoxia Mimetics (e.g., CoCl₂, DFO)
- Q3: We use Cobalt Chloride (CoCl₂) at 200 µM for 24 hours, but our cell viability drops below 70%, making subsequent protein misfolding assays unreliable. How can we adjust the protocol?
- A: CoCl₂ toxicity is batch- and cell-type-dependent. Perform a dose-response (50-300 µM) and time-course (6-48h) experiment measuring both HIF-1α stabilization (via western blot) and viability (via ATP-based assay). Aim for a condition that yields strong HIF-1α signal with >85% viability. Consider switching to Dimethyloxallylglycine (DMOG, 1 mM), which is often less acutely toxic.
- Q4: Desferrioxamine (DFO) isn’t inducing GRP78/BiP expression in our breast cancer spheroids, even at 100 µM. What are we missing?
- A: DFO is iron-chelating and acts slower. For 3D spheroids, penetration is key. Pre-mix DFO into the agarose/matrix when forming spheroids. Extend treatment time to 48-72 hours. Always include a positive control (e.g., Tunicamycin for ER stress) to confirm your UPR readout system is functional.
Topic 3: 3D Spheroid Cultures under Hypoxia
- Q5: The core of our spheroids becomes necrotic before hypoxic treatment, confounding the analysis of hypoxia-induced cell death. How do we prevent this?
- A: This indicates spheroids have grown too large (>500 µm diameter) for diffusion. Optimize the seeding cell number and growth period to form spheroids of a consistent, smaller size (200-400 µm). Use ultra-low attachment plates with clear, round bottoms for uniform shape. Consider using a perfusion bioreactor system for long-term hypoxic spheroid culture to enhance nutrient/waste exchange.
- Q6: How do we reliably extract protein from hypoxic spheroids for analyzing protein aggregation or UPR markers without losing insoluble aggregates?
- A: Standard RIPA may lose insoluble aggregates. Use a sequential extraction protocol:
- Lysis Buffer 1 (Soluble): Mild detergent to extract cytosolic/nuclear proteins. Centrifuge.
- Pellet Resuspension in Buffer 2 (Insoluble): Buffer with urea (e.g., 8M urea, 2% CHAPS) or mild SDS to solubilize aggregates. Analyze both fractions separately via western blot for targets like HIF-1α (soluble) and protein ubiquitination (insoluble fraction).
- A: Standard RIPA may lose insoluble aggregates. Use a sequential extraction protocol:
Key Experimental Protocols
Protocol 1: Validating Chemical Hypoxia Mimetics in 2D Culture
- Seed cells in 12-well plates.
- Treat with vehicle, CoCl₂ (150 µM), DFO (200 µM), or DMOG (1 mM) for 24h.
- Lyse cells in RIPA buffer with protease inhibitors.
- Perform Western Blot for HIF-1α (≈120 kDa) and a loading control (e.g., β-actin). Include a normoxic and chamber-induced hypoxic (1% O₂, 24h) sample as benchmarks.
- Quantify band intensity to confirm mimetic efficacy.
Protocol 2: Establishing & Treating 3D Spheroids for Hypoxic Stress
- Spheroid Formation: Use a 96-well ultra-low attachment plate. Seed 1000-3000 cells/well in 100 µL complete medium. Centrifuge plates at 300 x g for 3 min to aggregate cells. Culture for 72h to form compact spheroids.
- Hypoxic Treatment: For chambers: Transfer entire plate to a pre-equilibrated hypoxic chamber (1% O₂, 5% CO₂, 37°C). For mimetics: Carefully aspirate 50 µL medium from each well and add 50 µL of 2x concentrated drug (e.g., 2 mM DMOG).
- Viability Assessment (Post-treatment): Use a resazurin-based 3D viability assay. Add 10% (v/v) resazurin stock to each well. Incubate for 4-6h at 37°C. Measure fluorescence (Ex560/Em590).
- Analysis: Fix for imaging (IHC for HIF-1α, GRP78) or process for protein/RNA extraction as described in FAQ Q6.
Table 1: Comparison of Common Hypoxia-Inducing Methods
| Method | Typical Conditions | Time to Stabilize HIF-1α | Key Advantages | Key Limitations | Approx. Cost per Experiment |
|---|---|---|---|---|---|
| Tri-Gas Incubator | 1% O₂, 5% CO₂, 37°C | 4-8 hours | Most physiologically accurate, long-term studies possible. | High equipment cost, slower O₂ equilibration after opening. | $$$$ (Equipment) |
| Modular Chamber | Chamber flushed with 1% O₂, 5% CO₂, Balance N₂ | 1-2 hours | Flexible, fits in standard incubator, good for short interventions. | Small workspace, potential for leaks, gas consumption. | $$ |
| Cobalt Chloride | 100-200 µM in culture medium | 4-12 hours | Inexpensive, easy to use, highly potent. | Off-target toxic effects, not physiological (Co²⁺ vs. O₂). | $ |
| Dimethyloxallylglycine | 0.5-1 mM in culture medium | 8-24 hours | Inhibits HIF-PHDs directly, more stable than DMOG. | Broad prolyl hydroxylase inhibition, metabolic effects. | $$ |
Table 2: Troubleshooting 3D Spheroid Hypoxia Experiments
| Problem | Possible Cause | Solution |
|---|---|---|
| High size variability | Inconsistent seeding number or plate condition. | Use cell counter for accuracy; pre-coat plates with anti-adherence solution. |
| Spheroids disintegrate | Cell line is non-adherent (e.g., some leukemias). | Use hanging drop method or spheroid micro-molds. |
| No HIF-1α signal in core | Spheroid too small (<150 µm) or hypoxia too brief. | Increase seeding number for larger spheroids; extend hypoxic exposure to >48h. |
| Excessive central necrosis | Spheroid too large (>500 µm) or nutrient-deficient medium. | Reduce seeding number; change medium more frequently or use perfusion. |
Diagrams
Diagram 1: Hypoxia-Induced ER Stress & UPR Signaling
(Title: Hypoxia to UPR Signaling Pathway)
Diagram 2: Experimental Workflow for Hypoxic Protein Misfolding Study
(Title: Hypoxic Stress Experiment Workflow)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Hypoxic Protein Misfolding Research
| Item | Function/Application | Example Product/Assay |
|---|---|---|
| Hypoxia Chamber | Creates a physiologically accurate low-oxygen environment for cells. | Billups-Rothenberg modular chamber, Coy Lab vinyl chamber. |
| Portable O₂ Meter | Validates O₂ concentration at the cell culture level inside chambers. | PreSens Fibox 4, OM-CP-PRTTiO2. |
| Chemical Mimetics | Induces HIF stabilization in standard incubators; for screening. | CoCl₂ (Sigma 232696), DMOG (Cayman 71210). |
| Ultra-Low Attachment Plates | Enables formation of uniform 3D spheroids via forced aggregation. | Corning Costar 7007, Nunclon Sphera. |
| HIF-1α Antibody | Key validation tool for hypoxic response via WB/IHC. | Cell Signaling Technology #36169 (WB). |
| UPR Antibody Panel | Detects ER stress pathways (PERK, IRE1, ATF6 branches). | Antibodies for p-eIF2α, CHOP, XBP1s, GRP78/BiP. |
| Protein Aggregation Dye | Detects insoluble protein aggregates in cells/spheroids. | ProteoStat Aggresome Detection Kit (Enzo). |
| 3D Cell Viability Assay | Measures metabolic activity in spheroids (ATP/resazurin). | CellTiter-Glo 3D (Promega), AlamarBlue. |
| Sequential Extraction Kit | Separates soluble and insoluble protein fractions. | Insoluble Protein Extraction Kit (Millipore). |
Troubleshooting Guide & FAQs
FAQ 1: Why am I detecting no signal in my Western blot for BiP/GRP78 (a key UPR marker) in hypoxic tumor cell lysates?
- Potential Causes & Solutions:
- Hypoxia Level/Duration: The UPR may not be robustly activated. Extend hypoxia exposure time (e.g., 24-48 hours at 0.5-1% O₂) and verify hypoxia via HIF-1α staining.
- Sample Preparation: Use a strong RIPA buffer containing protease inhibitors. For aggregate-prone proteins, a sonication step may be necessary to solubilize proteins.
- Antibody Specificity: Validate antibody in a positive control (e.g., cells treated with 2-5 µM thapsigargin or 10 µg/mL tunicamycin for 6-16 hours under normoxia).
- Loading Control: Re-probe membrane for a stable loading control (e.g., β-Actin, COX IV). Degradation can occur during ER stress.
FAQ 2: My proteasome activity assay (fluorogenic substrate) shows inconsistent or low activity in hypoxic samples.
- Potential Causes & Solutions:
- Cell Lysis for Activity Assays: Use a gentle, non-denaturing lysis buffer (e.g., 50 mM Tris-HCl, pH 7.5, 5 mM MgCl₂, 1 mM DTT, 10% glycerol). Avoid detergents like SDS. Keep samples on ice.
- Assay Interference: Hypoxic cells have altered metabolism. Clear lysates by high-speed centrifugation (16,000 x g, 20 min, 4°C) to remove aggregates/debris. Include a BSA protein assay to normalize activity to total protein.
- Inhibitor Controls: Always run parallel reactions with a proteasome inhibitor (e.g., 10 µM MG-132 for chymotrypsin-like activity). Subtract this background from your readings.
- Oxidative Stress: Hypoxia can induce ROS. Include antioxidants (e.g., 1 mM DTT) in the assay buffer to protect the proteasome.
FAQ 3: Aggregate load assays (filter retardation or solubility fractionation) yield high background or no trapped protein.
- Potential Causes & Solutions:
- Membrane Blocking: For filter retardation assays, use 5% non-fat dry milk in PBS for at least 2 hours. Wash stringently with PBS containing 0.1% SDS.
- Aggregate Solubility: Ensure the lysis buffer for solubility assays is detergent-free for the "insoluble" fraction. The sequential extraction buffer series is critical:
- Soluble Fraction: Mild buffer (e.g., Tris-buffered saline with 1% NP-40).
- Membrane-Bound/Organelle Fraction: Buffer with 1% Triton X-100.
- Insoluble Aggregate Fraction: Buffer containing 2% SDS or urea.
- Positive Control: Include a cell model expressing a known aggregation-prone protein (e.g., mutant huntingtin fragment).
FAQ 4: How do I distinguish between the three UPR arms (IRE1, PERK, ATF6) in my hypoxia experiments?
- Solution: Use a combination of specific markers and pharmacological/inhibitor approaches. See Table 1 for key assays and controls.
Table 1: Quantitative Markers for UPR Arms in Hypoxic Stress
| UPR Arm | Key Marker | Assay Type | Typical Hypoxic Induction (Fold Change vs. Normoxia)* | Common Positive Control |
|---|---|---|---|---|
| IRE1α | XBP1 splicing | RT-PCR (gel shift) / qPCR | 2.5 - 5.0 fold | Thapsigargin (2 µM, 6h) |
| p-IRE1α (Ser724) | Western Blot | 3 - 8 fold | Tunicamycin (10 µg/mL, 4h) | |
| PERK | p-PERK (Thr980) | Western Blot | 4 - 10 fold | Thapsigargin (2 µM, 2h) |
| p-eIF2α (Ser51) | Western Blot | 3 - 6 fold | Tunicamycin (10 µg/mL, 2h) | |
| ATF4 | Western Blot / qPCR | 2 - 4 fold | ||
| ATF6 | Cleaved ATF6 (p50) | Western Blot | 2 - 3 fold | DTT (5 mM, 2h) |
| Integrated | BiP/GRP78 | Western Blot / qPCR | 2 - 6 fold | Thapsigargin/Tunicamycin |
| CHOP (DDIT3) | Western Blot / qPCR | 5 - 20+ fold | Prolonged Hypoxia (>24h) |
*Induction levels are cell line and context-dependent.
Table 2: Proteasome Activity Assay Comparison
| Assay Type | Target Activity | Substrate Example (Fluorogenic) | Typical Excitation/Emission (nm) | Hypoxia-Specific Consideration |
|---|---|---|---|---|
| Chymotrypsin-like | β5 subunit | Suc-LLVY-AMC | 380 / 460 | Often most significantly modulated in hypoxia. |
| Trypsin-like | β2 subunit | Boc-LRR-AMC | 380 / 460 | |
| Caspase-like | β1 subunit | Z-LLE-AMC | 380 / 460 | |
| Live-Cell Assay | All active sites | Proteasome-Glo (luciferin-based) | Luminescence | Accounts for cellular ATP levels, which are low in hypoxia. |
Experimental Protocols
Protocol 1: Sequential Detergent Extraction for Protein Aggregates (from Hypoxic Cells)
- Culture & Treatment: Grow cells on plates. Expose to hypoxia (e.g., 0.5% O₂, 37°C) for desired time.
- Harvest: Wash cells with ice-cold PBS. Scrape into PBS and pellet (500 x g, 5 min).
- Fractionation:
- Soluble Fraction: Lyse pellet in 100 µL of Buffer A (50 mM Tris-HCl pH 7.5, 150 mM NaCl, 1% NP-40, 1 mM EDTA, protease/phosphatase inhibitors) on ice for 20 min. Centrifuge at 16,000 x g, 30 min, 4°C. Collect supernatant (Soluble Fraction).
- Insoluble/ Aggregate Fraction: Wash the remaining pellet gently with Buffer A. Resuspend in 100 µL of Buffer B (50 mM Tris-HCl pH 7.5, 150 mM NaCl, 1% Triton X-100, 1% Sodium Deoxycholate, 1% SDS, protease/phosphatase inhibitors). Sonicate on ice (3 pulses of 10 sec). Incubate on ice 30 min. Centrifuge at 16,000 x g, 30 min, 20°C. Collect supernatant (Insoluble/Aggregate Fraction).
- Analysis: Run equal protein amounts from each fraction on SDS-PAGE and Western blot for your protein of interest. Aggregates will be enriched in the insoluble fraction.
Protocol 2: Fluorometric Proteasome Activity Assay (Cell Lysate)
- Lysate Prep: Lyse hypoxic/normoxic control cells in Assay Lysis Buffer (50 mM HEPES pH 7.5, 5 mM EDTA, 150 mM NaCl, 1% Triton X-100, 2 mM ATP). Clear by centrifugation (16,000 x g, 20 min, 4°C). Determine protein concentration.
- Reaction Setup: In a black 96-well plate, mix:
- 10-20 µg of total protein lysate.
- Assay Buffer (final: 50 mM HEPES pH 7.5, 5 mM EDTA, 0.05% NP-40).
- Fluorogenic substrate (e.g., Suc-LLVY-AMC for chymotrypsin-like activity) to a final concentration of 50 µM.
- Bring total volume to 100 µL.
- Controls: Set up wells with lysate + substrate + inhibitor (10 µM MG-132), and substrate-only blanks.
- Incubation & Read: Incubate at 37°C for 30-60 min. Measure fluorescence (Ex/Em: 380/460 nm) in a plate reader.
- Calculation: Subtract the average signal from the inhibitor control (non-proteasomal hydrolysis) from sample readings. Normalize to total protein and express as fold-change over normoxic control.
Pathway & Workflow Diagrams
Title: The Integrated Unfolded Protein Response (UPR) Signaling Network
Title: Workflow for Analyzing Protein Aggregates from Hypoxic Cells
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application | Example / Note |
|---|---|---|
| Hypoxia Chamber/Workstation | Maintains precise low-oxygen environment for cell culture. | InvivO₂ 400 (Baker) or C-Chamber (BioSpherix). Calibrate regularly. |
| HIF-1α Stabilizer (Chemical Hypoxia Mimetic) | Induces hypoxic response under normoxic conditions for controls. | Cobalt Chloride (CoCl₂, 100-200 µM) or Dimethyloxalylglycine (DMOG, 1 mM). |
| ER Stress Inducers (Positive Controls) | Pharmacologically induces ER stress/UPR activation. | Thapsigargin (SERCA inhibitor), Tunicamycin (N-glycosylation blocker). |
| Proteasome Inhibitors | Controls for proteasome-specific activity in assays. | MG-132 (reversible, cell-permeable), Bortezomib (clinical grade). |
| Fluorogenic Proteasome Substrates | Measure specific proteasome catalytic activities in lysates. | Suc-LLVY-AMC (Chymotrypsin-like). Use fresh DMSO stocks. |
| SDS-Resistant Antibodies for UPR | Detect key phosphorylated or cleaved UPR markers. | Anti-p-PERK (Thr980), Anti-p-eIF2α (Ser51), Anti-XBP1s (spliced). |
| Filter Retardation Assay Kit | Semi-quantify amyloid-like aggregates. | Includes cellulose acetate membrane and dot-blot apparatus. |
| ATP Detection Reagent (Luminescent) | Normalize proteasome activity in live-cell assays (Proteasome-Glo). | Accounts for low ATP in hypoxic cells. |
| Detergent Kits for Solubility Fractionation | Pre-mixed buffers for sequential extraction of aggregates. | Simplify the process and improve reproducibility. |
| qPCR Primers for UPR Target Genes | Quantify transcriptional output of UPR arms. | Primers for BiP, CHOP, XBP1s, ATF4, EDEM1. |
Technical Support & Troubleshooting Center
IRE1α Inhibitors
Q1: My IRE1α RNase inhibitor (e.g., 4μ8C, MKC-3946) is not reducing XBP1s splicing in my hypoxic cancer cell line. What could be wrong? A: Common issues include: 1) Hypoxia Optimization: Ensure hypoxia is properly established (use an anaerobic chamber or gas controller; verify with pimonidazole staining). IRE1α activation can be transient; perform a time-course (e.g., 2h, 8h, 24h). 2) Inhibitor Solubility & Stability: 4μ8C is DMSO-soluble but degrades in aqueous buffer. Prepare fresh stock for each experiment. 3) Off-Target Effects: Use a positive control like tunicamycin to confirm UPR induction. Consider combining genetic knockdown (siRNA against IRE1α) with pharmacological inhibition for validation.
Q2: I observe high cell death upon combining IRE1α inhibitors with hypoxia, making results uninterpretable. How can I adjust the protocol? A: This indicates potentiated ER stress. Titrate the inhibitor concentration downwards (start at 50% of literature IC50). Pre-treat cells with the inhibitor under normoxia for 2-4 hours before inducing hypoxia to ensure target engagement before severe stress onset. Monitor viability every 4-6 hours using real-time assays (like Incucyte).
PERK Modulators
Q3: The PERK inhibitor GSK2606414 is cytotoxic in my normoxic controls at published concentrations. What is a suitable starting dose for in vitro tumor models? A: Cytotoxicity is common due to basal PERK activity. Use a dose-response range (0.1 - 1.0 μM) for 24-48 hours. For hypoxia experiments, a lower pre-treatment dose (e.g., 0.1 μM, 1 hour pre-hypoxia) often modulates p-eIF2α without overt toxicity. Always include a vehicle control with equivalent DMSO.
Q4: I cannot detect consistent changes in ATF4 or CHOP protein levels after PERK inhibition in hypoxia, despite seeing p-eIF2α. A: This suggests compensatory signaling. 1) Check timepoints: ATF4/CHOP are transient. Sample at 8h and 16h of hypoxia. 2) Use integrated stress response (ISR) inhibitors (ISRIB) as a control to distinguish PERK-specific effects from general eIF2α signaling. 3) Run a positive control with thapsigargin.
HSP90/GRP78 Blockers
Q5: The HSP90 inhibitor (e.g., 17-AAG) causes massive client protein degradation in normoxia, masking hypoxic-specific effects. How can I refine the treatment? A: Use a pulsed treatment strategy: Treat cells with a low dose (e.g., 50 nM) for 2 hours, wash out, then subject to hypoxia. This primes the UPR without causing maximal proteotoxic shock. Alternatively, use GRP78-specific inhibitors (e.g., HA15) which may have a more direct effect on the UPR.
Q6: My GRP78 knockdown/knockout cells die too quickly in hypoxia to assay UPR inhibitors. Any advice? A: Use an inducible knockout (e.g., CRISPR-i) or shRNA system. Induce knockdown 72h prior to the experiment, which typically reduces but does not abolish GRP78, allowing short-term hypoxic exposure (8-12h). Alternatively, use a co-culture system with wild-type cells to provide paracrine support.
Table 1: Efficacy Profiles of Representative UPR-Targeting Compounds in Hypoxic Tumor Models
| Compound (Target) | Typical In Vitro IC50 / EC50 | Key Readout in Hypoxia | Common Cell Line Models | Key Pitfall |
|---|---|---|---|---|
| 4μ8C (IRE1α RNase) | 5-10 µM | >70% reduction in XBP1s splicing | MDA-MB-231, PC3, HCT116 | Short half-life in culture media |
| GSK2606414 (PERK) | 0.5-2 nM (biochemical) 10-100 nM (cellular) | >80% inhibition of p-eIF2α | HeLa, MEFs, 4T1 | High cytotoxicity in some lines |
| ISRIB (eIF2α signaling) | 5-50 nM | Reversal of p-eIF2α-mediated translation halt | Primary fibroblasts, Panc-1 | Can mask PERK-specific effects |
| 17-AAG (HSP90) | 10-80 nM (varies by client) | >90% depletion of HIF-1α & AKT | A549, SKOV-3 | Activates HSF1, causing compensatory stress |
| HA15 (GRP78) | 1-3 µM | Induction of ER stress markers, caspase-3 cleavage | Melanoma cell lines (A375), MCF-7 | Can induce non-ER stress pathways |
Table 2: Optimized Dosing for Hypoxia Combination Experiments
| Compound | Pre-hypoxia Treatment (Normoxia) | Co-treatment During Hypoxia | Hypoxia Duration | Assay Endpoint |
|---|---|---|---|---|
| IRE1α inhibitor | 1-2 hr, full dose | Yes, replenish if >12h | 4-24h | qRT-PCR for XBP1s |
| PERK inhibitor | 1 hr, low dose (0.1x IC50) | Yes | 8-16h | Immunoblot for p-eIF2α, ATF4 |
| HSP90/GRP78 blocker | No pre-treatment | Add at hypoxia onset | 12-48h | Immunoblot for client proteins, viability |
Experimental Protocols
Protocol 1: Validating IRE1α Inhibition in Hypoxic Conditions Objective: To assess the efficacy of an IRE1α RNase inhibitor in blocking the IRE1α-XBP1 arm of the UPR under hypoxia.
- Cell Seeding: Seed cells in 6-well plates (e.g., 2.5 x 10^5 cells/well) and allow to adhere for 24h.
- Inhibitor Pre-treatment: Add inhibitor (e.g., 10µM 4μ8C or vehicle) in fresh medium for 1 hour under normoxia (21% O2, 5% CO2).
- Hypoxia Induction: Place plates in a pre-equilibrated hypoxia chamber (1% O2, 5% CO2, 94% N2) for a defined period (e.g., 8h).
- RNA Extraction & cDNA Synthesis: Lyse cells with TRIzol. Perform RNA extraction and reverse transcription.
- XBP1 Splicing Assay: Perform PCR with primers flanking the IRE1α cleavage site in human XBP1. Analyze products on a 3% agarose gel (unspliced: 289bp, spliced: 263bp) or use qRT-PCR with spliced-specific probes.
- Controls: Include normoxic vehicle, normoxic inhibitor, and hypoxic vehicle controls.
Protocol 2: Measuring Integrated Stress Response (ISR) Output after PERK Modulation Objective: To quantify the effect of PERK modulators on downstream ATF4/CHOP expression and translational control.
- Cell Treatment: Treat cells with PERK inhibitor (e.g., 100nM GSK2606414) or activator (e.g., 2µM CCT020312) for 1h prior to and during hypoxia (1% O2, 16h).
- Protein Extraction: Harvest cells in RIPA buffer with protease/phosphatase inhibitors.
- Immunoblotting: Run 30-50 µg protein on SDS-PAGE, transfer to PVDF, and probe sequentially for p-eIF2α (Ser51), total eIF2α, ATF4, CHOP, and a loading control (β-actin).
- Puromycin Incorporation Assay (SUnSET): To directly measure translation rates, add 1µM puromycin for the final 10 minutes of hypoxia. Harvest cells and immunoblot for puromycin-incorporated peptides using anti-puromycin antibody.
- Data Analysis: Normalize p-eIF2α to total eIF2α and ATF4/CHOP to loading control. Compare puromycin signal intensity across conditions.
Visualizations
Diagram 1: Core UPR Signaling Pathways & Pharmacological Targets
Diagram 2: Experimental Workflow for Hypoxic UPR Drug Testing
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in UPR/Hypoxia Research | Example Product/Catalog # |
|---|---|---|
| Hypoxia Chamber/Workstation | Provides precise, reproducible low-oxygen (e.g., 0.1-2% O₂) environment for cell culture. | Baker Ruskinn InvivO2 400 |
| pO2 Indicator (Chemical) | Validates hypoxic conditions in culture media (colorimetric). | Image-iT Hypoxia Reagent |
| IRE1α RNase Inhibitor | Specifically blocks the endoribonuclease activity of IRE1α, inhibiting XBP1 splicing. | 4μ8C (Tocris, #412512) |
| PERK Inhibitor | ATP-competitive inhibitor of PERK kinase activity. | GSK2606414 (MedChemExpress, #HY-18072) |
| ISRIB | Reverses the effects of eIF2α phosphorylation, restoring translation. | Integrated Stress Response Inhibitor (Tocris, #5284) |
| HSP90 Inhibitor | Binds to HSP90, disrupting its chaperone function and inducing client protein degradation. | 17-AAG (Tanespimycin) (Selleckchem, #S1141) |
| GRP78/BiP Inhibitor | Specifically targets GRP78 ATPase activity, inducing ER stress. | HA15 (MedChemExpress, #HY-19716) |
| XBP1 Splicing PCR Primer Set | Detects unspliced and spliced XBP1 mRNA via conventional or qPCR. | Human XBP1 Splicing Assay Kit (BioVision, #K822-100) |
| Anti-puromycin Antibody | For SUnSET assay to measure global protein translation rates. | 12D10 (Merck Millipore, #MABE343) |
| ER Stress Antibody Sampler Kit | Contains antibodies for key UPR markers (p-eIF2α, ATF4, CHOP, etc.). | Cell Signaling Technology, #9956 |
Technical Support Center
This support center provides troubleshooting guidance for common experimental challenges in developing TME-targeted drug delivery systems, framed within the thesis context of Addressing protein misfolding in hypoxic tumor environments.
FAQs & Troubleshooting Guides
Q1: Our hypoxia-responsive nanoparticle system shows insufficient drug release (<20%) in our in vitro hypoxia chamber (0.5% O2). What could be the issue? A: This often relates to the sensitivity of the hypoxia-responsive linker. Verify the following:
- Linker Chemistry: Ensure you are using a linker (e.g., nitroimidazole or azobenzene derivatives) with a reduction potential appropriate for the enzymatic milieu of your specific tumor model. The overexpressed reductases (e.g., P450 reductase, NQO1) in hypoxic cells may not efficiently cleave your chosen linker.
- Protocol Check: Confirm hypoxia incubation time. Effective release often requires >24-48 hours under sustained hypoxia. Use a positive control (e.g., a known hypoxia-activated prodrug like Tirapazamine) to validate chamber conditions.
- Nanoparticle Stability: The nanoparticle may be too stable, preventing adequate degradation after linker cleavage. Consider incorporating additional TME-sensitive elements (e.g., MMP-cleavable peptides) for sequential activation.
Q2: When testing our GRP78-targeted liposomes, we observe high non-specific uptake in normoxic cancer cells and fibroblasts, compromising target specificity. How can we improve this? A: Non-specific uptake indicates insufficient reliance on stress-induced GRP78 membrane translocation.
- Validate Target Expression: First, quantify surface GRP78 via flow cytometry in your hypoxic vs. normoxic cells. Surface expression should increase ≥3-fold under hypoxia/ER stress. Use Thapsigargin (2µM, 12h) as a positive control for ER stress induction.
- Ligand Density Optimization: Reduce the density of the targeting ligand (e.g., GRP78-binding peptide or antibody) on the liposome surface. High density can drive Fc receptor or scavenger receptor-mediated non-specific endocytosis. Titrate ligand density from 0.5% to 2% mol ratio.
- Employ a Dual-Targeting Strategy: Use a logic-gated approach where the carrier requires two TME signals (e.g., low pH and MMP-9 presence) to expose the GRP78-targeting moiety, minimizing off-target binding.
Q3: Our proteasome inhibitor-loaded delivery system effectively kills hypoxic cells but also causes severe toxicity in co-cultured tumor-associated macrophages (TAMs). How can we spare TAMs? A: This toxicity likely arises from shared vulnerability due to proteostasis stress.
- Mechanism Investigation: Profile the unfolded protein response (UPR) in your TAMs post-treatment (assay XBP1 splicing, ATF4, CHOP levels). The inhibitor may be exacerbating pre-existing ER stress in TAMs.
- Exploit Differential Metabolism: Utilize a hypoxia-specific prodrug formulation. Since TAMs in the hypoxic core are often metabolically distinct, a linker activated specifically by the exaggerated reductase activity of stressed tumor cells (not just low O2) may help. Consider testing quinone-based bioreductive triggers.
- Dosage & Scheduling: Implement a pulsed dosing regimen in vitro to allow for UPR recovery in TAMs, mimicking potential clinical administration schedules.
Q4: How do we quantitatively distinguish between cell death caused directly by drug action versus that caused by exacerbated protein misfolding in our experiments? A: You need orthogonal assays to deconvolve the mechanisms.
- Direct Cytotoxicity: Measure classic apoptosis/necrosis markers (Annexin V/PI, caspase-3/7 activity) at early time points (12-24h).
- ER Stress & Misfolding: In parallel, assay for UPR terminal markers:
- CHOP/GADD153 upregulation (Western blot, qPCR).
- Phospho-eIF2α levels (indicative of PERK pathway activation).
- ATF6 cleavage (Western blot).
- Correlation: Use chemical chaperones (e.g., 4-Phenylbutyric acid, 2mM) or IRE1α inhibitors (e.g., 4µ8C, 10µM) as rescue agents. If cell death is significantly reduced with these agents, it confirms a major contribution from exacerbated protein misfolding.
Table 1: Common Hypoxia-Responsive Linkers and Their Characteristics
| Linker Type | Activation Trigger | Typical Release Kinetics (0.5-1% O2) | Key Reductase(s) | Potential Off-Target Activation |
|---|---|---|---|---|
| 2-Nitroimidazole | Hypoxic Reduction | 24-48 hours | P450 Reductase, NQO1 | High reductase activity in liver |
| Azobenzene | Hypoxic Reduction | 12-24 hours | Azoreductase | Gut microbiota |
| Quinone | Hypoxic Reduction | 6-12 hours | DT-Diaphorase (NQO1) | Oxidative stress in normoxic cells |
| Nitroaromatic | Hypoxic Reduction | >48 hours | Multiple one-electron reductases | Slow kinetics may limit efficacy |
Table 2: Key Assays for Validating ER Stress Induction in Hypoxic Tumor Cells
| Assay Target | Method | Expected Change in Hypoxia (vs. Normoxia) | Time Point Post-Hypoxia Induction |
|---|---|---|---|
| HIF-1α | Western Blot | >5-fold increase | 4-24 hours |
| GRP78/BiP | Surface Flow Cytometry | 2-5 fold increase | 24-48 hours |
| XBP1 Splicing | RT-PCR / RFLP | Spliced/Un-spliced ratio >0.5 | 12-24 hours |
| CHOP/GADD153 | qPCR | 10-50 fold increase | 24-48 hours |
| Phospho-eIF2α | ELISA | 2-4 fold increase | 6-24 hours |
Experimental Protocols
Protocol 1: Evaluating Hypoxia-Specific Drug Release from Nanoparticles
- Objective: Quantify drug release kinetics from hypoxia-responsive nanoparticles under controlled oxygen tension.
- Materials: Hypoxia chamber, anaerobic jars, or live-cell imaging system with environmental control; Dialysis bags (MWCO appropriate); HPLC system.
- Method:
- Prepare nanoparticle suspensions in PBS (pH 7.4) with 0.1% w/v Tween 80 to simulate sink conditions.
- Place 1 mL of suspension in a sealed dialysis bag.
- Immerse the bag in 50 mL release medium. Place the entire setup inside a hypoxia chamber pre-equilibrated to 0.5% O2, 5% CO2, 37°C. Maintain normoxic control at 21% O2.
- At predetermined intervals (1, 2, 4, 8, 12, 24, 48h), sample 1 mL from the external medium and replace with fresh, pre-equilibrated medium.
- Quantify drug concentration using HPLC. Calculate cumulative release percentage.
Protocol 2: Measuring Surface GRP78 Expression in Stressed Tumor Cells
- Objective: Quantify stress-induced translocation of GRP78 to the cell membrane as a targeting biomarker.
- Materials: Anti-GRP78 antibody (conjugated to Alexa Fluor 488 or unconjugated), Isotype control antibody, Flow cytometer, Thapsigargin.
- Method:
- Induce ER stress by treating cells with 2µM Thapsigargin or incubating in a 0.5% O2 hypoxia chamber for 24-48 hours.
- Harvest cells using non-enzymatic dissociation buffer to preserve surface proteins.
- Wash cells twice with ice-cold FACS buffer (PBS + 2% FBS).
- Incubate 1x10^6 cells with primary anti-GRP78 antibody (or isotype control) on ice for 45 minutes in the dark.
- Wash twice. If using an unconjugated primary, incubate with a fluorescent secondary antibody for 30 minutes on ice, then wash.
- Resuspend in FACS buffer and analyze immediately via flow cytometry. Report results as Median Fluorescence Intensity (MFI) ratio of stained vs. isotype control.
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Hypoxia/Targeting Research |
|---|---|
| Cobalt(II) Chloride Hexahydrate (CoCl2) | A chemical hypoxia mimetic that stabilizes HIF-1α by inhibiting prolyl hydroxylases (PHDs), used for in vitro induction of hypoxic responses. |
| Desferrioxamine (DFO) | An iron chelator that also stabilizes HIF-1α by inhibiting PHDs (iron-dependent), providing an alternative method to induce hypoxic signaling. |
| Thapsigargin | A potent and specific inhibitor of the SERCA Ca2+ pump, causing rapid ER calcium depletion and induction of severe ER stress. Used as a positive control for UPR activation. |
| 4-Phenylbutyric Acid (4-PBA) | A chemical chaperone that reduces ER stress by facilitating protein folding and trafficking. Used in rescue experiments to confirm the role of protein misfolding in cytotoxicity. |
| Tirapazamine (TPZ) | A classic bioreductive prodrug selectively activated under severe hypoxia. Serves as a benchmark compound for validating hypoxia-responsive drug delivery systems. |
| Nitroreductase (NTR) Enzyme | Commonly used in vitro to validate the activation kinetics of nitroimidazole-based hypoxia-sensitive linkers in a controlled enzymatic environment. |
| Anti-HIF-1α Antibody | Critical for validating hypoxia models via Western blot or immunofluorescence. Confirms nuclear accumulation of HIF-1α in experimental conditions. |
| Bafilomycin A1 | A V-ATPase inhibitor that blocks endosomal/lysosomal acidification. Used to study the intracellular trafficking and endosomal escape of nano-delivery systems. |
Technical Support & Troubleshooting Center
Context: This support content is designed for researchers working on the thesis "Addressing protein misfolding in hypoxic tumor environments." It addresses common experimental issues when combining proteostatic stressors (e.g., proteasome inhibitors, HSP90 inhibitors) with chemo/radiotherapy to overcome therapeutic resistance.
FAQs & Troubleshooting Guides
Q1: In our 3D hypoxic spheroid model, the expected synergistic cytotoxicity from combining Bortezomib and Doxorubicin is not observed. What could be the cause? A: This is often due to inadequate hypoxia induction or drug penetration. First, verify hypoxia using a probe like pimonidazole (immunofluorescence) or a HIF-1α activity reporter. For spheroids >500µm diameter, a necrotic core can form, altering drug distribution. Pre-treat spheroids with the proteasome inhibitor for 4-6 hours before adding doxorubicin to ensure proteostatic stress is established. Ensure doxorubicin concentration is titrated (common range: 0.1-1 µM) as synergy windows can be narrow.
Q2: Our Western blots for unfolded protein response (UPR) markers (ATF4, CHOP, XBP1s) are inconsistent after co-treatment with an HSP90 inhibitor and radiation. A: Radiation timing is critical. The UPR is transient. For a standard protocol: Treat cells with 17-AAG (e.g., 100 nM) for 6 hours, then irradiate (e.g., 2-4 Gy). Harvest protein at 3, 6, and 12 hours post-irradiation. Include a hypoxic control (1% O₂ for 24h). Use actin and a loading control for total protein (e.g., Ponceau S) due to potential stress-induced actin changes. Ensure lysis buffer contains fresh protease/phosphatase inhibitors.
Q3: How do we optimize the sequencing depth and analysis for RNA-seq to profile ER stress in treated tumor samples? A: For bulk RNA-seq from in vivo tumors, aim for >40 million paired-end reads per sample to capture low-abundance transcripts. Key steps: 1) Preserve tissue in RNAlater immediately post-resection. 2) Enrich for ER stress/UPR pathways by including spike-in controls for quality assessment. 3) In analysis, focus on the Hallmark "Unfolded Protein Response" gene set from MSigDB. Normalize using DESeq2 or edgeR, and confirm hypoxia signature (e.g., CA9, VEGFA) to contextualize findings.
Q4: Our in vivo experiment shows excessive toxicity when combining carfilzomib with fractionated radiotherapy. How can we adjust the dosing schedule? A: This combination often requires aggressive supportive care and schedule modification. A proven protocol is: Administer carfilzomib (4 mg/kg IV) on Days 1, 2, 15, 16 of a 4-week cycle. Administer radiotherapy (2 Gy/fraction) ONLY on Days 3, 4, 5, 17, 18, 19. This 24-48h gap allows proteostatic stress to prime cells while mitigating overlapping toxicities (e.g., enteritis). Monitor weight, BUN (for renal function), and complete blood counts twice weekly. Use concurrent hydration.
Table 1: Synergistic Cytotoxicity (Combination Index) of Common Proteostatic Stressors with Chemotherapeutics in Hypoxic Cells
| Proteostatic Stressor | Chemotherapeutic | Cell Line | Hypoxia Level (% O₂) | Combination Index (CI) <1 = Synergy | Key Readout |
|---|---|---|---|---|---|
| Bortezomib (10 nM) | Cisplatin (2 µM) | A549 (NSCLC) | 0.5% | 0.45 ± 0.12 | Caspase-3/7 activity |
| 17-AAG (100 nM) | Doxorubicin (0.5 µM) | MCF-7 (Breast) | 1.0% | 0.62 ± 0.09 | Clonogenic survival |
| Celecoxib (40 µM)* | Etoposide (5 µM) | PC3 (Prostate) | 0.2% | 0.78 ± 0.15 | γH2AX foci (DNA damage) |
| AEBSF (20 µM) | Temozolomide (50 µM) | U87MG (Glioblastoma) | 0.5% | 0.31 ± 0.08 | Annexin V/PI flow cytometry |
Celecoxib acts as a proteostatic stressor via ER Ca²⁺ depletion. *AEBSF is a SERCA2b inhibitor inducing ER stress.
Table 2: In Vivo Tumor Growth Delay with Combination Therapies
| Treatment Group | Tumor Model (Subcutaneous) | Radiation Dose | Tumor Doubling Time Delay (vs. Vehicle) | p-value | Notable Toxicity |
|---|---|---|---|---|---|
| Vehicle + RT | MDA-MB-231 (Breast) | 8 Gy x 3 fractions | 4.2 days | - | None |
| Bortezomib + RT | MDA-MB-231 (Breast) | 8 Gy x 3 fractions | 11.7 days | <0.01 | Transient weight loss |
| Vehicle + RT | GL261 (Glioblastoma) | 3 Gy x 10 fractions | 6.5 days | - | None |
| PU-H71 (HSP90i) + RT | GL261 (Glioblastoma) | 3 Gy x 10 fractions | 18.1 days | <0.001 | Mild hepatotoxicity |
Experimental Protocols
Protocol 1: Measuring Proteasome Inhibition Potentiation of DNA Damage Title: Immunofluorescence for γH2AX and 20S Proteasome Activity in Hypoxic Cells.
- Seed cells on glass coverslips in a hypoxic chamber (0.5-1% O₂, 5% CO₂, 94% N₂) for 24h.
- Treat with proteasome inhibitor (e.g., MG-132, 5µM) for 4h under hypoxia.
- Irradiate plates at room temperature using a clinical irradiator (e.g., 4 Gy). Return to hypoxia.
- Fix at 1h post-IR with 4% PFA for 15 min. Permeabilize with 0.5% Triton X-100.
- Stain with primary anti-γH2AX (1:1000) and secondary Alexa Fluor 488 antibody. Counterstain nuclei with DAPI.
- Image using a confocal microscope (>50 cells/condition). Quantify foci/nucleus.
- In parallel wells, lyse cells for 20S proteasome activity assay using a fluorogenic substrate (e.g., Suc-LLVY-AMC).
Protocol 2: Assessing UPR Activation via qPCR Title: Quantitative PCR for ER Stress Marker Genes.
- Treat cells under normoxia/hypoxia with your proteostatic stressor for 8h.
- Extract total RNA using TRIzol, with DNase I treatment.
- Synthesize cDNA from 1µg RNA using a high-capacity reverse transcriptase kit with random hexamers.
- Prepare qPCR reactions in triplicate using SYBR Green master mix. Use 10ng cDNA per reaction.
- Primer sequences (human):
- ATF4: F: 5'-ATGACCGAAATGAGCTTCCTG-3', R: 5'-GCTGGAGAACCCATGAGGTT-3'
- CHOP (DDIT3): F: 5'-GCACCTCCCAGAGCCCTCACTCTCC-3', R: 5'-GTCTACTCCAAGCCTTCCCCCTGCG-3'
- XBP1s (spliced): F: 5'-CTGAGTCCGAATCAGGTGCAG-3', R: 5'-ATCCATGGGGAGATGTTCTGG-3'
- Run on a real-time cycler: 95°C for 3 min, then 40 cycles of 95°C for 10s and 60°C for 30s.
- Analyze using the ΔΔCt method, normalizing to GAPDH or ACTB.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function & Application | Example Product/Catalog # |
|---|---|---|
| Hypoxia Chamber/Workstation | Maintains precise low-oxygen environment (0.1-5% O₂) for cell culture. | Baker Ruskinn InvivO₂ 400 |
| Proteasome Activity Assay Kit | Fluorometric measurement of 20S proteasome chymotrypsin-like activity in cell lysates. | Cayman Chemical #601090 |
| HIF-1α ELISA Kit | Quantifies HIF-1α protein levels in hypoxic tumor lysates. | Abcam #ab216842 |
| ER-Tracker Dye | Live-cell staining of the endoplasmic reticulum for imaging ER morphology under stress. | Thermo Fisher Scientific E34251 |
| Human Stress & Toxicity Pathway Finder PCR Array | Profiles 84 key genes in UPR, hypoxia, and oxidative stress pathways. | Qiagen PAHS-003Z |
| Clonogenic Survival Assay Kit | Essential for measuring long-term cell survival post chemo/radio/proteostatic stress combination. | Cell Biolabs #CBA-151 |
| Lactate Dehydrogenase (LDH) Cytotoxicity Assay | Measures membrane integrity as a marker of compound-induced cell death. | Promega #G1780 |
| In Vivo Imaging System (IVIS) | Tracks tumor growth and can be used with luciferase-based hypoxia reporters. | PerkinElmer IVIS Spectrum |
Visualizations
Diagram 1: Core Signaling Pathway of Combination Therapy
Diagram 2: Experimental Workflow for In Vivo Validation
Overcoming Hurdles: Challenges in Targeting Tumor Proteostasis and Optimizing Therapeutic Efficacy
Technical Support Center: Troubleshooting UPR-Based Cancer Therapeutics
FAQ: Core Concepts & Experimental Design
Q1: Our compound shows promising toxicity in tumor cell lines but is equally toxic to non-transformed epithelial cells in normoxia. How can we improve selectivity for hypoxic tumor cells with active UPR?
- A: This is the central selectivity dilemma. Your compound likely targets a UPR component (e.g., IRE1α, PERK) that is active but transient in normal cells under physiological ER stress. In hypoxic tumors, the UPR is chronically and irreversibly activated. To exploit this, design your screening assay to compare:
- Normal cells: Under a pulse of mild, reversible ER stress (e.g., 2h Tunicamycin treatment, then washout).
- Hypoxic tumor cells: Under chronic hypoxia (e.g., 48h at 0.5% O₂). Measure cell viability 72h later. A selective compound will spare normal cells that recover and show cytotoxicity only in chronically hypoxic cells. Validate by checking UPR marker resolution (e.g., CHOP, XBP1s) in normal cells post-stress.
Q2: When we induce hypoxia in vitro, we don't see a consistent upregulation of UPR markers across our tumor cell panel. What are we doing wrong?
- A: Hypoxia alone may not be sufficient to trigger a strong UPR if glycolytic flux maintains energy levels. Ensure:
- Use physiological hypoxia (<0.5% O₂). Many incubators don't accurately maintain ultra-low O₂. Use an anaerobic workstation or sealed chambers with verified O₂ sensors.
- Combine hypoxia with nutrient deprivation (low glucose/media) to mimic the tumor microenvironment and robustly induce ER stress.
- Check time points. UPR markers like phospho-eIF2α peak early (2-8h), while CHOP peaks later (12-24h). Perform a time course.
- Include a positive control: Treat a normoxic sample with 2µg/mL Tunicamycin for 6h.
Q3: Our IRE1α RNase inhibitor kills hypoxic tumor spheroids, but in vivo mouse models show severe pancreatic toxicity. How do we troubleshoot this?
- A: Pancreatic acinar cells have a high protein folding load and active baseline UPR. This is a classic on-target, off-tissue toxicity.
- Troubleshooting Steps:
- Dose Fractionation: Move from a bolus dose to a metronomic, low-dose schedule to avoid overwhelming normal tissue.
- Biomarker Monitoring: In your pre-clinical trial, monitor serum amylase/lipase and perform IHC for XBP1s splicing in pancreatic tissue. Correlate toxicity with drug levels.
- Prodrug Strategy: Develop a prodrug activated specifically in the hypoxic/acidic tumor microenvironment (e.g., using nitroreductase or low pH-sensitive linkers).
- Troubleshooting Steps:
Experimental Protocols
Protocol 1: Evaluating Compound Selectivity in a Co-culture System
Objective: To test if a UPR-targeting agent selectively kills hypoxic tumor cells while sparing co-cultured normal fibroblasts with an inducible UPR.
Materials: Hypoxia chamber (0.5% O₂), Normoxic incubator (21% O₂), GFP-labeled tumor cells (e.g., MDA-MB-231), red fluorescent CellTracker-labeled normal fibroblasts, test compound, Tunicamycin.
Method:
- Seed co-culture (1:1 ratio) in 96-well plates.
- Pre-condition normal cells: Treat the plate for 2h with 1µg/mL Tunicamycin in normoxia. Wash 3x with PBS to remove.
- Split conditions:
- Group A (Normoxia): Return to 21% O₂ incubator.
- Group B (Chronic Hypoxia): Place in 0.5% O₂ chamber for 48h.
- Add serial dilutions of the test compound to both groups. Incubate for 72h.
- Viability Assay: Use a fluorescent plate reader. Measure GFP signal (tumor cells) and red fluorescence (fibroblasts) separately. Calculate IC50 for each cell type in each condition.
Protocol 2: Quantifying UPR Activation Status via qPCR and Immunoblot
Objective: To definitively profile the UPR branch activity in hypoxic vs. stressed normal cells.
Method:
- Sample Preparation:
- Tumor Cells: Harvest after 24h at 0.5% O₂.
- Normal Cells: Harvest 6h after start of 2µg/mL Tunicamycin treatment (acute stress) AND 24h after Tunicamycin washout (recovery phase).
- qPCR for UPR Target Genes:
- Extract RNA, synthesize cDNA.
- Run triplicate reactions for: XBP1s (IRE1), CHOP (PERK), BiP/GRP78 (all branches), and HPRT1 (housekeeping).
- Use ΔΔCt method to calculate fold change relative to unstressed normoxic control.
- Immunoblot for UPR Proteins:
- Lyse cells in RIPA buffer with phosphatase/protease inhibitors.
- Run 30µg protein on 4-12% Bis-Tris gel.
- Transfer to PVDF membrane.
- Probe with antibodies: Phospho-PERK (Thr980), Total-PERK, Phospho-eIF2α (Ser51), CHOP, XBP1s, BiP/GRP78, β-Actin.
- Use chemiluminescence detection.
Data Presentation
Table 1: Comparative UPR Marker Expression in Selectivity Assay
| Cell Type / Condition | XBP1s Splicing (Fold Change) | CHOP Protein Level (Relative to Actin) | Cell Viability Post-Compound (10µM) |
|---|---|---|---|
| Normal Fibroblasts (Acute Tm Stress) | 12.5 ± 1.2 | 8.3 ± 0.7 | 92% ± 5% |
| Normal Fibroblasts (Recovery) | 1.5 ± 0.3 | 1.2 ± 0.2 | 88% ± 4% |
| Hypoxic Tumor Cells (0.5% O₂, 24h) | 15.8 ± 2.1 | 22.7 ± 3.1 | 35% ± 8% |
| Normoxic Tumor Cells | 1.1 ± 0.2 | 1.0 ± 0.1 | 85% ± 6% |
Table 2: In Vivo Efficacy vs. Toxicity of Candidate UPR Inhibitors
| Compound (Target) | Tumor Growth Inhibition (TGI) | Maximum Tolerated Dose (MTD) | Pancreatitis Incidence (at MTD) | Selective Index (TGI/ Toxicity Score*) |
|---|---|---|---|---|
| Compound A (IRE1α RNase) | 78% | 50 mg/kg | 100% | 0.8 |
| Compound B (PERK Inhibitor) | 65% | 100 mg/kg | 40% | 1.6 |
| Prodrug B (Hypoxia-activated) | 70% | 200 mg/kg | 0% | 8.5 |
*Toxicity Score: 1 (mild) to 5 (severe) based on histopathology & serum markers.
Pathway & Workflow Diagrams
Diagram Title: Mechanism of Selective UPR Targeting in Tumors vs. Normal Tissue
Diagram Title: Co-culture Assay Workflow for Selectivity Screening
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in UPR/Hypoxia Research | Example & Key Consideration |
|---|---|---|
| Hypoxia Chamber / Workstation | Maintains precise, low O₂ environments (<0.5% O₂) for chronic induction. | Coy Lab Products chambers, Baker Ruskinn workstations. Verify O₂ with continuous sensors (e.g., PreSens). |
| UPR Inducers (Positive Controls) | Induce acute ER stress to calibrate assays and as controls. | Tunicamycin (N-glycosylation blocker), Thapsigargin (SERCA inhibitor). Use low, titrated doses. |
| UPR Branch-Specific Reporters | Monitor specific UPR arm activation live or endpoint. | XBP1-splicing reporter (GFP), ATF4-luciferase reporter. Transfer stable cell lines for consistency. |
| Phospho-Specific Antibodies | Detect activation states of UPR sensors via WB/IHC. | Anti-phospho-PERK (Thr980), Anti-phospho-eIF2α (Ser51). Always run with total protein antibody. |
| Metabolic Stress Media | Mimics tumor nutrient deprivation to synergize with hypoxia. | Low Glucose (1mM) DMEM, Dialyzed FBS. Combine with hypoxia for robust UPR. |
| Cytotoxicity Assay (Multiplex) | Distinguish viability of different cell types in co-culture. | CellTracker dyes, GFP-labeled lines, or assays measuring ATP/Protease activity separately. |
| Hypoxia-Activated Prodrugs | Tool compounds to validate selectivity by hypoxia. | Tirapazamine (TPZ), or novel research-grade PERK/IRE1 inhibitor prodrugs. |
| CHOP & XBP1s Knockout Cells | Isogenic controls to confirm on-target mechanism of toxicity. | Use CRISPR-Cas9 generated pools or clones. Validate knockout via WB and sequencing. |
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our western blot analysis for UPR markers (BiP, CHOP, XBP1s) in hypoxic tumor spheroids shows inconsistent results between replicates. What could be the cause and how can we resolve this? A: Inconsistent UPR marker detection often stems from inadequate control of the hypoxic gradient within 3D spheroids. Ensure standardized spheroid size (e.g., 500 ± 50 µm diameter) and precise hypoxic chamber calibration. Use an oxygen probe (e.g., Fibox 4 trace) to log pO₂ throughout the experiment. Pre-equilibrate all media in the target hypoxia (e.g., 0.5% O₂) for >4 hours before use. For lysis, rapidly process spheroids in pre-chilled buffer while maintaining them on ice under a nitrogen blanket to prevent reoxygenation during harvesting.
Q2: When using hypoxia-sensitive fluorescent probes (e.g., Pimonidazole), we observe a heterogeneous staining pattern that is difficult to quantify across tumor sections. What is the best practice for analysis? A: Heterogeneous pimonidazole staining is expected due to tumor hypoxia gradients. For quantification, transition from manual scoring to digital pathology or image analysis software (e.g., QuPath, HALO). Follow this protocol:
- Stain with anti-pimonidazole antibody (e.g., Hypoxyprobe-1) and counterstain with DAPI.
- Scan entire tumor section at 20x magnification.
- Use software to define viable tumor regions (exclude necrosis).
- Set a consistent intensity threshold for positive signal based on an isoxic control.
- Output data as % Positive Area and Mean Signal Intensity for multiple regions of interest (e.g., peri-necrotic, middle, invasive front) to map the gradient. See Table 1 for typical distribution.
Table 1: Representative Quantification of Pimonidazole Staining in Heterogeneous Tumor Models
| Tumor Region | Median % Positive Area (Range) | Approximate pO₂ (mmHg) |
|---|---|---|
| Peri-necrotic core | 65-85% | < 2.5 |
| Intermediate zone | 20-45% | 2.5 - 10 |
| Invasive front / edge | 5-15% | > 10 |
Q3: Our attempts to pharmacologically inhibit the UPR (using compounds like ISRIB or GSK2606414) in hypoxic cells yield variable cytotoxicity in clonogenic assays. How should we design these experiments? A: Variability often arises from differential UPR branch activation across cell subpopulations. Implement this workflow:
- Pre-stratify: Prior to drug treatment, characterize the basal and hypoxia-induced UPR status of your cell lines via qPCR for XBP1s, ATF4, CHOP.
- Schedule Treatment: Add UPR inhibitor after hypoxia establishment (e.g., 24h post-hypoxia induction), as immediate co-treatment can mask adaptive pro-survival effects.
- Use Combination Controls: Include a group treated with a hypoxia-activated prodrug (e.g., Tirapazamine) to compare mechanism-specific cytotoxicity.
- Assay Choice: Use a long-term (10-14 day) clonogenic assay over short-term MTT. Account for hypoxia-induced growth arrest by normalizing colony counts to a hypoxic, vehicle-treated control. See Table 2 for expected trends.
Table 2: Expected Outcomes from UPR Inhibition in Normoxia vs. Hypoxia (Clonogenic Survival)
| Condition | GSK2606414 (PERK inhibitor) | ISRIB (eIF2α signaling blocker) |
|---|---|---|
| Normoxia (21% O₂) | Minimal effect (>90% survival) | Minimal effect (>90% survival) |
| Acute Hypoxia (0.5% O₂, 24h) | Moderate effect (40-60% survival) | Mild effect (70-85% survival) |
| Chronic Hypoxia (0.5% O₂, 72h) | Strong effect (10-30% survival) | Variable effect (30-80% survival) |
Q4: We are having trouble detecting differential activation of the three UPR branches (IRE1α, ATF6, PERK) in our co-culture models of tumor and stromal cells under hypoxia. Any recommendations? A: The stromal compartment can buffer tumor cell stress. You need to isolate the responses. Use a transwell co-culture system and follow this protocol:
- Step 1: Seed fluorescently labeled tumor cells (e.g., GFP+) in the bottom well. Seed stromal cells (e.g., cancer-associated fibroblasts) in the insert.
- Step 2: Expose to hypoxia (0.5-1% O₂) for your desired duration (e.g., 48h).
- Step 3: Rapidly separate compartments. Lyse tumor cells (GFP+) separately using immunoprecipitation-compatible lysis buffer.
- Step 4: Analyze UPR branches specifically from the tumor lysate using:
- IRE1α: Assess XBP1 splicing via RT-PCR or antibody for XBP1s.
- ATF6: Detect cleaved nuclear ATF6 fragment by western blot (Abcam ab122897).
- PERK: Monitor phospho-eIF2α (Ser51) and downstream ATF4.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Hypoxia and UPR in Tumor Heterogeneity
| Reagent / Material | Function & Application Note |
|---|---|
| Hypoxyprobe-1 (Pimonidazole) | Binds to proteins at pO₂ < 10 mmHg. Gold standard for histological hypoxia detection. |
| Portable Oxygen Probe (e.g., Fibox 4) | Validates and logs oxygen concentration in culture chambers or within spheroids/microtumors. |
| GSK2606414 | Potent and selective PERK inhibitor. Used to dissect the PERK-eIF2α-ATF4-CHOP arm of the UPR. |
| 4μ8C | A specific IRE1α RNase domain inhibitor. Useful for blocking the IRE1α-XBP1 splicing pathway. |
| Recombinant Human VEGF | Positive control for HIF-1α activity; hypoxia-induced secretion is often UPR-dependent. |
| HIF-1α Stabilizer (e.g, DMOG) | Prolyl-hydroxylase inhibitor used as a hypoxia mimetic to induce HIF-1α independently of oxygen. |
| 3D Spheroid Matrix (e.g., Matrigel) | Provides an in vivo-like environment for studying hypoxic gradient formation in 3D models. |
| RNAscope Multiplex Assay | Enables in situ visualization of UPR-related mRNA transcripts (e.g., XBP1s, CHOP) in heterogeneous tissues. |
Experimental Protocol: Quantifying Differential UPR Activation Across a Hypoxic Gradient in Tumor Spheroids
Objective: To spatially resolve the activation of the three UPR branches in relation to a hypoxic gradient within a single 3D tumor spheroid.
Materials: HCT116 colorectal carcinoma cells, Ultra-low attachment round-bottom plates, Hypoxic chamber (0.5% O₂), Cryostat, Anti-pimonidazole antibody, Antibodies for IRE1α phosphorylation (p-IRE1α Ser724), XBP1s, Cleaved ATF6, Phospho-PERK (Thr980), Phospho-eIF2α (Ser51), ATF4, CHOP.
Methodology:
- Spheroid Generation: Seed 2000 HCT116 cells/well in a 96-well round-bottom ultra-low attachment plate. Centrifuge at 300xg for 3 min. Culture for 72h in normoxia to form compact spheroids (~500µm).
- Hypoxic Treatment & Probing: Transfer plates to a pre-calibrated hypoxic chamber (0.5% O₂, 5% CO₂, 94.5% N₂) for 48h. Add pimonidazole HCl (100 µM) to the medium 4h before fixation.
- Processing & Sectioning: Harvest spheroids, embed in OCT compound, and flash-freeze. Serially section (10 µm thickness) using a cryostat.
- Multiplex Immunofluorescence Staining:
- Cycle 1: Stain for pimonidazole (FITC channel) and DAPI.
- Image entire spheroid section. Map hypoxia gradient.
- Cycle 2: Perform antibody elution. Stain for p-IRE1α and XBP1s (Cy3/Cy5 channels).
- Cycle 3: Perform antibody elution. Stain for cleaved ATF6 and p-eIF2α (Cy3/Cy5 channels).
- Align all cycle images using DAPI landmarks.
- Image Analysis: Using ImageJ or HALO, divide each spheroid into three concentric zones (Core, Intermediate, Rim) based on pimonidazole signal. Quantify the mean fluorescence intensity for each UPR marker in each zone. Normalize to the Rim zone intensity for each spheroid.
Signaling Pathway & Experimental Workflow Diagrams
Title: Hypoxia-Induced UPR Signaling Pathways Determining Cell Fate
Title: Workflow for Spatially Resolving UPR Activation in Hypoxic Spheroids
Troubleshooting Guides & FAQs
Q1: During siRNA-mediated knockdown of IRE1α in our hypoxic MDA-MB-231 cell model, we observe a paradoxical increase in XBP1s target gene expression instead of the expected decrease. What could be causing this?
A1: This is a classic compensatory adaptation. In chronic ER stress under hypoxia, parallel UPR arms compensate. Knocking down IRE1α likely relieves its reported inhibitory phosphorylation of PERK (a form of UPR crosstalk), leading to enhanced PERK-ATF4 signaling which can upregulate a subset of overlapping target genes. Additionally, loss of IRE1α may activate the ATF6 arm.
- Troubleshooting Steps:
- Monitor All UPR Arms: Simultaneously measure phospho-PERK, ATF4 protein levels, and cleaved ATF6 (p50) via western blot in your knockdown model.
- Use Pharmacological Inhibition: Combine IRE1α RNase inhibitor (4μ8C, 20μM) with PERK inhibitor (GSK2656157, 1μM) to confirm crosstalk.
- Extended Time Course: Assess effects at 24h, 48h, and 72h post-knockdown. Compensatory mechanisms are often time-dependent.
Q2: Our drug candidate, an ER stress inducer, shows potent efficacy in vitro but fails in in vivo xenograft models of hypoxic pancreatic tumors. What adaptive resistance mechanisms should we investigate?
A2: The tumor microenvironment in vivo introduces key adaptive pressures absent in vitro.
- Primary Investigations:
- Autophagy Induction: Tumors may upregulate autophagy to clear drug-induced misfolded protein aggregates. Stain tumor sections for LC3B puncta (immunofluorescence) and measure p62 degradation by western blot.
- Antioxidant Upregulation: Chronic ER stress and hypoxia can co-induce NRF2. Check for increased NRF2 nuclear localization and expression of genes like NOQ1 and HMOX1.
- Immune-Evasive Adaptation: Isolate tumor-infiltrating lymphocytes and check for PD-L1 upregulation on tumor cells via flow cytometry, as ER stress can induce immunomodulatory proteins.
Q3: When quantifying the UPR in hypoxic primary glioblastoma cells, our qPCR data for XBP1s, ATF4, and CHOP are highly variable and do not correlate well with protein-level readouts. How can we standardize measurements?
A3: Hypoxia and metabolic stress directly impact transcription and translation rates, decoupling mRNA and protein levels.
- Standardized Protocol:
- Normalization: For qPCR, use multiple stable reference genes validated for hypoxia/ER stress (e.g., TBP, RPL13A). Avoid GAPDH or ACTB as they can fluctuate.
- Prioritize Protein/Activity Assays:
- IRE1α Activity: Use a fluorescent reporter plasmid (pUPRE-GFP) or quantify XBP1 splicing via capillary electrophoresis.
- PERK Activity: Directly measure phosphorylation of eIF2α (Ser51) by ELISA or western blot.
- ATF6 Activation: Monitor the cleaved nuclear form (p50) by western blot of nuclear extracts.
- Table: Recommended Assays for UPR Quantification in Hypoxia
| UPR Arm | Optimal mRNA Target | Optimal Protein/Functional Assay | Common Pitfall in Hypoxia |
|---|---|---|---|
| IRE1α-XBP1 | XBP1s (spliced) | XBP1s protein (WB) or splicing assay | mRNA decay pathways are altered; protein is more reliable. |
| PERK | ATF4, CHOP | p-eIF2α (Ser51), ATF4 protein | Global translation inhibition delays protein output. |
| ATF6 | HEDJ, GRP78 | Cleaved ATF6 (p50) in nucleus | Full-length ATF6 processing can be rapid and transient. |
Q4: We are trying to chronically induce ER stress with Tunicamycin in hypoxic conditions, but our cells die rapidly via apoptosis. How can we model persistent, adaptive ER stress instead of acute cell death?
A4: Acute, high-dose insults trigger apoptosis. To model adaptive chronic stress, use sub-lethal, prolonged stimulation.
- Detailed Methodology:
- Titrate the Inducer: Perform a dose-response (e.g., Tunicamycin 0.1 - 2.0 μg/mL) under hypoxia (1% O₂) for 24h. Determine the concentration yielding <20% cell death (via Trypan Blue or Annexin V assay).
- Prolonged Exposure Protocol:
- Plate cells and allow adherence for 24h.
- Switch to hypoxic chamber (1% O₂, 5% CO₂).
- After 12h of hypoxia acclimation, add the sub-lethal dose of inducer.
- Refresh medium + inducer every 48h.
- Monitor daily for morphological changes (vacuolization) and culture confluence. The adaptive phase typically shows reduced proliferation but maintained viability beyond 96h.
- Alternative Inducer: Consider milder inducers like Thapsigargin (an SERCA pump inhibitor) at low nanomolar ranges (e.g., 10-50 nM), which may produce a more sustained ER calcium depletion.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Category | Example Product (Vendor) | Key Function in Chronic ER Stress/Hypoxia Research |
|---|---|---|
| Hypoxia Chamber/Workstation | Baker Ruskinn InvivO₂ 400 (Baker) | Maintains precise, low oxygen tension (e.g., 0.1-1% O₂) for cell culture, critical for mimicking tumor microenvironment. |
| Chemical ER Stress Inducers | Tunicamycin (Sigma, T7765), Thapsigargin (Tocris, 1138) | Induces ER stress by inhibiting N-linked glycosylation (Tunica) or SERCA pump activity (Thapsi), respectively. |
| UPR Pathway Inhibitors | 4μ8C (IRE1α RNase) (Sigma, SML0949), GSK2656157 (PERK) (MedChemExpress, HY-15872), AEBSF (ATF6) (Sigma, A8456) | Pharmacologically dissects contributions of specific UPR arms to compensatory signaling. |
| ER-Targeted ROS Probe | ERroGFP (Addgene, plasmid #67815) | Genetically encoded sensor for real-time monitoring of oxidative stress specifically within the ER lumen. |
| Autophagy Flux Inhibitor | Bafilomycin A1 (Sigma, B1793) | Inhibits autophagosome-lysosome fusion; used in tandem with LC3B immunoblotting to measure autophagic flux, a key resistance mechanism. |
| Viability/Proliferation Assay RealTime-Glo MT Cell Viability Assay (Promega, JA1011) | Allows longitudinal, non-destructive monitoring of cell health over extended chronic stress time courses. | |
| siRNA Library | ON-TARGETplus Human UPR & Apoptosis siRNA Library (Dharmacon) | For systematic, high-throughput screening of genes involved in ER stress adaptation and cell fate decisions. |
Experimental Protocols
Protocol 1: Assessing UPR Crosstalk via Combinatorial Pharmacological Inhibition Objective: To delineate compensatory activation between IRE1α and PERK pathways under chronic hypoxic ER stress.
- Seed cells in 6-well plates and acclimatize to hypoxia (1% O₂) for 12h.
- Induce ER stress with a sub-lethal dose (pre-determined) of Tunicamycin (e.g., 0.5 μg/mL).
- At the time of induction, add inhibitors: DMSO (control), 20μM 4μ8C (IRE1α), 1μM GSK2656157 (PERK), or the combination of both.
- Incubate under hypoxia for 24h and 48h.
- Harvest cells for protein extraction.
- Analyze by western blot using antibodies against: p-IRE1α (Ser724), XBP1s, p-PERK (Thr980), p-eIF2α (Ser51), ATF4, and β-Actin loading control.
- Key Interpretation: Combination treatment should show the most complete suppression of adaptive markers (e.g., ATF4, XBP1s) compared to single agents.
Protocol 2: Monitoring Autophagic Flux as an Adaptive Response Objective: To determine if autophagy is upregulated as a compensatory survival mechanism.
- Establish chronic ER stress in hypoxic cells as described in FAQ A4.
- At the desired time point (e.g., 96h), treat cells with 100 nM Bafilomycin A1 or vehicle control for the final 4-6 hours of incubation.
- Lyse cells and perform western blot analysis for LC3B-I/II and p62/SQSTM1.
- Quantification: Calculate the flux as the difference in LC3B-II intensity and p62 intensity with vs. without Bafilomycin A1. Increased flux (greater delta) indicates autophagy induction as an adaptive response.
Diagrams
Optimizing Pharmacokinetics and Bioavailability in the Complex Tumor Microenvironment
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: In our in vivo model, our nanoparticle formulation shows excellent plasma PK but fails to accumulate in the hypoxic core of the tumor. What could be the main issue? A: This is a common issue driven by the abnormal tumor vasculature and increased interstitial fluid pressure (IFP). The Enhanced Permeability and Retention (EPR) effect is heterogeneous and often minimal in hypoxic regions. Solution: Consider active targeting (e.g., ligands for hypoxia-induced cell surface markers like CA-IX) or size/charge optimization. Particles sized 20-200 nm with a slightly positive surface charge may improve penetration into dense, hypoxic matrices. Implement multi-compartment PK modeling that includes a "hypoxic tumor compartment" with distinct parameters for perfusion, permeability, and binding.
Q2: Our prodrug designed for hypoxia-specific activation is showing systemic toxicity. How can we improve its tumor-specific activation? A: Systemic toxicity indicates off-target activation, likely due to basal reductase levels in normal tissues. Troubleshooting Guide:
- Check Prodrug Design: Increase the reduction potential (E1/2) threshold. The prodrug should only be reduced at very low oxygen tensions (<0.1% O2). Use more hypoxia-selective triggers (e.g., nitroimidazole derivatives over quinones).
- Adjust Dosing Schedule: Consider metronomic dosing to minimize peak plasma concentrations that drive normal tissue exposure.
- Combine with Tumor Priming: Use a vascular normalization agent (e.g., low-dose antiangiogenic) transiently to improve oxygen and drug delivery, then administer the prodrug. This can create a more defined activation window.
Q3: How do we accurately measure drug concentration and exposure time in the hypoxic niche to model PK/PD relationships? A: Direct measurement is challenging. Use a combination of:
- Hypoxia Probes: Co-administer pimonidazole. Post-sacrifice, stain tumor sections for pimonidazole adducts (hypoxic regions) and your drug (via immunofluorescence or click chemistry if tagged).
- Microdialysis: Insert microdialysis probes into the tumor, but this technique averages signals from mixed regions.
- Mathematical Modeling: Use data from the above to parameterize a spatial PK model. Key parameters to measure are listed in Table 1.
Table 1: Key Quantitative Parameters for Hypoxic Tumor PK Modeling
| Parameter | Typical Range in Normoxic Tumor | Typical Range in Hypoxic Tumor | Measurement Technique |
|---|---|---|---|
| Vascular Density | 100-200 vessels/mm² | <50 vessels/mm² | CD31 immunohistochemistry |
| Perfusion Rate | Variable, often low | Extremely Low | Dynamic Contrast-Enhanced MRI |
| Interstitial Fluid Pressure (IFP) | 5-20 mmHg | Can exceed 30-40 mmHg | Wick-in-needle technique |
| Extracellular pH | ~6.5-7.0 | ~6.0-6.5 | pH-sensitive MRI or fluorescent probes |
| Drug Diffusion Coefficient (D) | 10-100 µm²/s (size-dependent) | Reduced by 50-90% | Fluorescence Recovery After Photobleaching (FRAP) |
Q4: Protein aggregation is observed in our hypoxia-treated cell lines, interfering with our drug target. How can we mitigate this in our PK/PD assays? A: This directly links to the thesis on Addressing protein misfolding in hypoxic tumor environments. Experimental Protocol:
- Pre-condition Assay: Treat cells with a pharmacological chaperone (e.g., 4-phenylbutyric acid (4-PBA) at 1-5 mM) or a low-dose proteasome inhibitor (e.g., Bortezomib at 5 nM) 2 hours prior to hypoxia induction (1% O2). This can stabilize protein folding or induce HSP expression.
- Co-administration: Include these folding regulators in your drug treatment media during hypoxia experiments.
- Control: Always include a normoxic control with identical drug/chaperone treatment to isolate hypoxia-specific effects on PK (uptake, efflux) from target viability.
Experimental Protocols
Protocol 1: Evaluating Nanocarrier Penetration in 3D Hypoxic Tumor Spheroids Purpose: To simulate and measure drug carrier penetration into the hypoxic core of tumors. Methodology:
- Spheroid Generation: Plate U87-MG or HCT-116 cells in ultra-low attachment 96-well plates (2000 cells/well). Centrifuge at 300xg for 3 min. Culture for 72-96 hours until spheroids reach 400-500 µm diameter.
- Hypoxia Induction: Transfer spheroid plates to a modular incubator chamber. Flush with a gas mixture of 1% O2, 5% CO2, and balance N2 for 15 min. Seal and incubate at 37°C for 48 hours. Maintain normoxic controls.
- Treatment: Add fluorescently labeled nanocarriers (e.g., DiI-labeled liposomes) to the spheroid media.
- Imaging & Analysis: At t=1, 4, 24 hours, wash spheroids and image using confocal microscopy with Z-stacking. Use ImageJ to plot fluorescence intensity from the periphery (0%) to the core (100%). Calculate penetration depth (µm where signal drops to 50% of periphery).
Protocol 2: Testing Hypoxia-Specific Prodrug Activation Purpose: To quantify the selectivity and efficiency of prodrug activation in hypoxic versus normoxic cells. Methodology:
- Cell Preparation: Seed cells in 96-well plates. At 80% confluence, place one set in a hypoxia chamber (0.1% O2) and another in normoxia (21% O2) for 24 hours.
- Drug Treatment: Treat cells with a range of prodrug concentrations. Include the active parent drug as a positive control.
- Viability Assay: After 72 hours, assess cell viability using a resazurin (Alamar Blue) assay. Measure fluorescence (Ex560/Em590).
- Data Analysis: Calculate IC50 values for prodrug and parent drug under both conditions. The Hypoxic Cytotoxicity Ratio (HCR) = IC50 (Normoxia) / IC50 (Hypoxia). A successful prodrug will have an HCR > 10.
Signaling Pathways & Workflows
Diagram 1: PK Barriers in the Hypoxic Tumor Niche
Diagram 2: Strategy for Hypoxia-Targeted PK Optimization
The Scientist's Toolkit: Research Reagent Solutions
| Item Name | Function & Relevance to Hypoxic TME PK Research |
|---|---|
| Hypoxia Chamber (Modular) | Creates a controlled, low-oxygen environment (e.g., 0.1-2% O2) for in vitro cell and spheroid experiments to study hypoxia-specific PK. |
| Pimonidazole HCl | A hypoxia marker probe. Forms protein adducts in cells at pO₂ < 10 mmHg. Used to spatially map hypoxic regions in tumors for correlating with drug distribution. |
| HIF-1α Antibody | Validates hypoxia induction at the molecular level via western blot or IHC. Confirms activation of the primary transcriptional regulator of the hypoxic response. |
| CA-IX (Carbonic Anhydrase IX) Antibody | Marker for chronic hypoxia. Useful for developing active targeting ligands on drug carriers to enhance delivery to hypoxic regions. |
| Resazurin Sodium Salt (Alamar Blue) | Cell viability assay reagent used in hypoxic conditions as it is not oxygen-dependent like MTT, allowing accurate PK/PD endpoint measurement. |
| 3D Spheroid/ULA Plates | For generating multicellular tumor spheroids that develop a hypoxic, necrotic core, providing a more realistic model for penetration studies than 2D monolayers. |
| 4-Phenylbutyric Acid (4-PBA) | A chemical chaperone used to mitigate endoplasmic reticulum stress and protein misfolding in hypoxic cells, clarifying its impact on drug target engagement. |
| Fluorescent Dye (DiI, Cy5.5) | For covalent or non-covalent labeling of nanoparticles, antibodies, or drugs to enable tracking of distribution via fluorescence microscopy or IVIS imaging. |
| Recombinant Human LOX (Lysyl Oxidase) | Enzyme that crosslinks collagen, mimicking hypoxia-induced ECM stiffening. Used to pretreat models to study its barrier effect on drug diffusion. |
Technical Support Center: Troubleshooting UPR Biomarker Assays
This support center provides guidance for common experimental challenges encountered in developing biomarkers for UPR (Unfolded Protein Response)-targeted therapies, within the context of addressing protein misfolding in hypoxic tumor environments.
Frequently Asked Questions (FAQs) & Troubleshooting Guides
Q1: In our qPCR analysis of UPR target genes (e.g., XBP1s, ATF4, CHOP), we are seeing high inter-sample variability and inconsistent fold-change values in hypoxic tumor cell lines. What are the primary causes and solutions?
A1: This is commonly due to inconsistent hypoxia induction or RNA degradation. Follow this protocol:
- Hypoxia Chamber Calibration: Use an independent oxygen probe (e.g., PreSens) to verify and log O₂ levels (e.g., 0.1-1% O₂) throughout the experiment. Do not rely solely on chamber settings.
- RNA Stabilization: Add a RNA stabilization reagent (e.g., RNAlater) directly to culture plates before cell lysis, especially for time-course experiments.
- Reference Genes: Use hypoxia-stable reference genes validated for your model. PPIA and RPLP0 are often more stable than GAPDH or ACTB under hypoxia. Perform geNorm or NormFinder analysis to confirm.
Q2: Our immunohistochemistry (IHC) staining for UPR markers (like p-eIF2α or BiP/GRP78) on formalin-fixed paraffin-embedded (FFPE) tumor sections yields high background or weak specific signal. How can we optimize?
A2: This typically involves antigen retrieval and antibody titration.
- Antigen Retrieval: For UPR markers, a heat-induced epitope retrieval (HIER) method using Tris-EDTA buffer (pH 9.0) at 95-100°C for 20 minutes is often more effective than citrate buffer (pH 6.0).
- Hypoxia Co-Staining: Include a validated hypoxia marker (e.g., CAIX, HIF-1α) on a serial section to confirm the hypoxic region of the tumor. Weak UPR signal may indicate the analyzed area is not hypoxic.
- Blocking: Use a blocking buffer with 5% normal serum from the antibody host species and 2.5% BSA for 1 hour at room temperature to reduce non-specific binding.
Q3: When performing Western blot analysis for UPR proteins from hypoxic tumor tissue lysates, we observe smearing or multiple bands. What steps should we take?
A3: This is frequently caused by protein degradation or improper lysis.
- Lysis Protocol: Use a fresh, cold RIPA buffer supplemented with 1x protease inhibitor cocktail and 1mM PMSF. For phospho-proteins (e.g., p-eIF2α), add phosphatase inhibitors (1mM Na₃VO₄, 10mM NaF).
- Tissue Processing: Snap-freeze tumor tissue in liquid nitrogen immediately upon resection. Homogenize the frozen tissue directly in lysis buffer using a mechanical homogenizer on ice.
- Sample Boiling: Boil samples for 5 minutes, not 10, as over-boiling can aggregate UPR transmembrane proteins like IRE1α.
Q4: Our flow cytometry analysis of cell surface GRP78 in live hypoxic cells shows poor staining resolution. How can we improve it?
A4:
- Antibody Selection: Use a primary antibody validated for extracellular epitope recognition. Perform staining in PBS with 2% FBS on ice.
- Hypoxia Quenching: Keep cells in hypoxic conditions until just before staining. Use pre-reduced, anaerobic buffers if possible to prevent reoxygenation artifacts during the staining procedure.
- Fixation: If fixation is necessary, use 2% PFA for 10 minutes on ice, not methanol.
Table 1: Common UPR Biomarkers and Their Detection Parameters in Hypoxic Tumors
| Biomarker | Assay Type | Sample Type | Key Challenge in Hypoxia | Recommended Control |
|---|---|---|---|---|
| XBP1 Splicing | RT-qPCR, RNase Assay | Cell/RNA | Rapid turnover of spliced variant (XBP1s) | Normoxic cells + Tunicamycin (2µg/ml, 6h) |
| BiP/GRP78 | IHC, Western Blot | FFPE, Lysate | High constitutive expression in tumors | Stain adjacent normal tissue section. |
| p-eIF2α (Ser51) | Western Blot, IF | Lysate, FFPE | Transient phosphorylation kinetics | Include an ISR activator (e.g., Salubrinal 50µM). |
| ATF4 Protein | Western Blot | Lysate | Short half-life; requires proteasome inhibition (MG132) during lysis. | Co-stain for CHOP as downstream verification. |
| CHOP (DDIT3) | IHC, qPCR | FFPE, RNA | Can be induced by non-UPR stressors (e.g., DNA damage). | Correlate with another UPR branch marker. |
Table 2: Troubleshooting Summary: Expected vs. Erroneous Results
| Experiment | Expected Result | Common Erroneous Result | Likely Cause |
|---|---|---|---|
| Hypoxia-Induced XBP1 Splicing | Clear shift from unspliced to spliced XBP1 band. | No shift or faint bands. | RNA degradation, insufficient hypoxia duration (<8h for solid tumor lines). |
| IHC for p-eIF2α in Tumor FFPE | Strong nuclear staining in regions adjacent to necrosis. | Diffuse cytoplasmic stain or no signal. | Over-fixation, incorrect antigen retrieval pH. |
| Western for ATF4 | Strong induction at 4-8h hypoxia, declining by 24h. | No band or very faint band. | Lack of proteasome inhibitors in lysis buffer. |
| Surface GRP78 Flow Cytometry | Clear positive population shift in hypoxic cells. | High background in all samples. | Antibody concentration too high, reoxygenation before staining. |
Experimental Protocols
Protocol 1: Detecting XBP1 Splicing via RT-qPCR from Hypoxic Tumor Cells
Objective: To accurately quantify the spliced/active form of XBP1 (XBP1s) as a marker of IRE1α branch activation.
- Hypoxia Treatment: Culture cells in a calibrated tri-gas incubator (1% O₂, 5% CO₂, 94% N₂) for 8-16 hours. Include a normoxic control (21% O₂) and a positive control (2µg/ml Tunicamycin, 6h).
- RNA Extraction: Lyse cells directly in the culture dish using TRIzol reagent. Isolate RNA following manufacturer's instructions. Include a DNase I digestion step.
- cDNA Synthesis: Use 1µg total RNA with a high-fidelity reverse transcriptase (e.g., SuperScript IV) and random hexamers.
- qPCR Amplification:
- Primers: Use primers flanking the XBP1 splice site. To specifically detect XBP1s, a common method is to use a primer set that yields products of different sizes for spliced vs. unspliced variants, separable by gel electrophoresis post-qPCR, or to use a spliced-form-specific TaqMan assay.
- Mix: 10µL SYBR Green Master Mix, 0.5µM each primer, 2µL cDNA, nuclease-free water to 20µL.
- Cycling: 95°C for 3 min; 40 cycles of (95°C for 10s, 60°C for 30s). Perform melt curve analysis.
- Analysis: Calculate ∆Ct relative to a stable reference gene (PPIA). Compare ∆Ct values between normoxic and hypoxic samples.
Protocol 2: Co-Staining for Hypoxia and UPR Markers in FFPE Tumor Sections
Objective: To spatially correlate hypoxia and UPR activation within the tumor microenvironment.
- Sectioning: Cut 4-5µm serial sections from FFPE tumor blocks. Mount on charged slides.
- Deparaffinization & Retrieval:
- Bake slides at 60°C for 1h.
- Deparaffinize in xylene (3 x 5 min) and rehydrate through graded ethanol.
- Perform HIER in Tris-EDTA (pH 9.0) using a decloaking chamber at 95°C for 20 min.
- Cool for 30 min, then rinse in PBS.
- Immunohistochemistry:
- Blocking: Block endogenous peroxidase with 3% H₂O₂ for 10 min. Block protein with 5% normal goat serum for 1h.
- Primary Antibody: Apply primary antibody (e.g., mouse anti-HIF-1α or anti-CAIX for hypoxia; rabbit anti-BiP for UPR) diluted in blocking buffer overnight at 4°C.
- Detection: Use a polymer-based HRP detection system (e.g., EnVision+) and develop with DAB chromogen (brown stain).
- Counterstaining & Mounting: Counterstain with hematoxylin, dehydrate, clear, and mount with a permanent mounting medium.
- Analysis: Image serial sections using a whole-slide scanner. Use image analysis software to align sections and quantify marker overlap in peri-necrotic regions.
Pathway & Workflow Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for UPR Biomarker Development in Hypoxia
| Item | Function in Research | Example Product/Catalog Number |
|---|---|---|
| Tri-Gas Incubator | Precise control of O₂, CO₂, and N₂ levels to mimic the hypoxic tumor microenvironment in vitro. | Thermo Fisher Scientific Forma Series II |
| Oxygen Probe | Independent verification and logging of O₂ concentration in cell culture media or tissues. | PreSens Fibox 4 trace. |
| Hypoxia Marker Antibodies | IHC validation of hypoxic regions in tumor sections (critical for spatial correlation with UPR). | Anti-CAIX (Abcam, ab109616); Anti-HIF-1α (Novus, NB100-479). |
| UPR Branch-Specific Antibodies | Detection of key UPR protein markers: BiP (all branches), p-eIF2α (PERK), XBP1s (IRE1), ATF6 p50 (ATF6). | Anti-BiP/GRP78 (CST, 3177); Anti-p-eIF2α (Ser51) (CST, 3398). |
| XBP1 Splicing Detection Assay | Gold-standard assay for IRE1 branch activity. Measures the shift from unspliced to spliced XBP1 mRNA. | Human XBP1 Splicing Assay Kit (ImmuneChem, ICPC3011). |
| RNAlater Stabilization Reagent | Preserves RNA integrity immediately upon sample collection, preventing degradation during hypoxia-to-normoxia transition. | Thermo Fisher Scientific AM7020. |
| Proteasome & Phosphatase Inhibitors | Essential additives to lysis buffers for stabilizing labile UPR proteins (e.g., ATF4) and phospho-epitopes (e.g., p-eIF2α). | MG132 (CST, 2194); PhosSTOP (Roche, 4906845001). |
| Validated Reference Genes for Hypoxia | Stable housekeeping genes for qPCR normalization under low oxygen conditions. | PPIA (Cyclophilin A), RPLP0 (Ribosomal Protein Lateral Stalk Subunit P0). |
Bench to Bedside: Validating UPR Targets and Comparing Emerging Therapeutic Candidates
Technical Support Center: Troubleshooting PDX & Immunocompetent Model Experiments
This support center provides targeted guidance for researchers validating protein misfolding-targeting lead compounds in hypoxic tumor models, as part of a thesis on Addressing protein misfolding in hypoxic tumor environments.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our PDX models show unexpectedly low engraftment rates (<20%). What are the primary factors to check? A: Low engraftment in PDX models, particularly for tumors prone to hypoxia-induced protein misfolding, often stems from sample handling or host factors. Key checks:
- Tumor Viability: Ensure tumor tissue is implanted within 1 hour of collection. Use cold preservation media (e.g., HBSS on ice).
- Hypoxia Preservation: For studies on protein misfolding, immediately post-resection, place a fragment of tumor in a stabilizing agent (e.g., RNA/DNA shield) for hypoxic marker analysis (HIF-1α, GRP78) to establish a baseline.
- Host Mouse Strain: Use NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) or similar for maximum engraftment. Ensure mice are 6-8 weeks old.
- Implantation Site: Subrenal capsule or orthotopic sites often yield higher engraftment than subcutaneous for certain cancers.
Q2: How do we reliably maintain and monitor intratumoral hypoxia in our PDX models during compound efficacy testing? A: Sustained hypoxia is critical for studying protein misfolding. Implement these protocols:
- Hypoxia Monitoring: Implant pimonidazole hydrochloride (60 mg/kg, i.p.) 90 minutes before tumor harvest. Detect via immunohistochemistry (IHC) with Hypoxyprobe antibodies.
- Tumor Size Control: Do not let tumors exceed 1500 mm³, as central necrosis can confound hypoxic signaling. Target 500-800 mm³ for treatment initiation.
- Validation Assay: Co-stain for HIF-1α and the misfolded protein client (e.g., mutant p53) via IHC/IF on pretreatment samples to confirm model relevance.
Q3: We observe a disconnect between efficacy in immunodeficient PDX models and failure in syngeneic/immunocompetent models. How should we investigate this? A: This is common for therapies targeting protein misfolding, as the immune microenvironment is a key modifier. Follow this diagnostic workflow:
- Check Immune Cell Infiltration: Perform flow cytometry on treated syngeneic tumors (CD45+, CD3+, CD8+, CD4+, Tregs, Macrophages).
- Analyze Immunogenic Cell Death (ICD): Test if your lead compound induces calreticulin exposure, ATP, and HMGB1 release in vitro using murine cancer cell lines.
- Profile Cytokines: Use a multiplex ELISA (e.g., IFN-γ, TNF-α, IL-6, IL-10) on tumor homogenates from treated immunocompetent models.
Q4: What is the best method to quantify markers of protein misfolding (e.g., ubiquitinated aggregates, ER stress) in tumor tissue post-treatment? A: Use a multi-modal approach on FFPE or snap-frozen tumor sections.
- IHC/Immunofluorescence: For ubiquitin (FK2 antibody), GRP78/BiP, and ATF4. Use tyramide signal amplification (TSA) for low-abundance targets.
- Protein Extraction Protocol: For insoluble aggregates, homogenize tumor tissue in a RIPA buffer with 1% SDS, benzonase, and protease/ubiquitin protease inhibitors. Separate soluble and insoluble fractions via high-speed centrifugation (100,000 x g, 30 min). Analyze the insoluble pellet by solubilizing in 8M urea buffer.
- qRT-PCR: Validate ER stress pathway activation via splicing assay for XBP1 and expression of CHOP (DDIT3).
Q5: How should we dose our lead compound to account for altered pharmacokinetics in hypoxic, poorly vascularized tumors? A: Hypoxia reduces drug perfusion. Consider these steps:
- Pharmacokinetic/Pharmacodynamic (PK/PD) Study: Conduct a pilot with tumor-bearing mice. Measure compound levels in plasma vs. tumor core (hypoxic region) at 1, 6, and 24h post-dose via LC-MS.
- Biomarker-Driven Dosing: If the compound downregulates a misfolding marker (e.g., GRP78), use IHC on serial biopsies to establish the minimum effective concentration and optimal schedule.
- Consider Prodrugs: Explore hypoxia-activated prodrug (HAP) strategies if the lead compound's efficacy is severely limited by oxygenation.
Key Experimental Protocols
Protocol 1: Establishing a Hypoxia-Validated PDX Model for Protein Misfolding Studies
- Implantation: Matrigel-mixed tumor fragments (~2 mm³) implanted subcutaneously into NSG mouse flanks.
- Hypoxia Baseline: At P1 passage, when tumor reaches ~300 mm³, inject pimonidazole (60 mg/kg, i.p.). Harvest tumor 90 min later.
- Validation: Snap-freeze one portion for Western blot (HIF-1α, GRP78). Fix another portion for IHC co-staining (HIF-1α, Pimonidazole, Ubiquitin).
- Passaging: Only passage tumors showing >40% hypoxic area (pimonidazole+) and elevated misfolding markers.
Protocol 2: Evaluating Compound Efficacy in a Syngeneic Model with Hypoxia Monitoring
- Cell Implantation: Inject 0.5e6 murine cancer cells (e.g., 4T1, CT26) orthotopically or subcutaneously into C57BL/6 or BALB/c mice.
- Treatment & Monitoring: Randomize mice at tumor volume 100 mm³ (n=8/group). Administer vehicle or lead compound.
- In Vivo Hypoxia Imaging: On Day 7 of treatment, inject pimonidazole (60 mg/kg) 90 min before harvesting a subset of tumors (n=3/group).
- Analysis: Weigh tumors. Slice for: a) Flow cytometry (immune profiling), b) Snap-freezing (protein/RNA analysis), c) Fixation (IHC: Hypoxia, TUNEL, CD8, target protein).
Table 1: Comparative Efficacy Metrics of Lead Compound X in Different Model Types
| Model Type | Cancer Line | Avg. Tumor Growth Inhibition (TGI) | Hypoxic Area Reduction (vs. Vehicle) | GRP78 Protein Downregulation | Immune Cell Infiltration Change (CD8+/Treg ratio) |
|---|---|---|---|---|---|
| PDX (NSCLC) | LU-01 (NSG mice) | 72% | -35% | -60% | N/A |
| Syngeneic | LLC (C57BL/6 mice) | 40% | -20% | -30% | +2.5 fold |
| Syngeneic (Immunodepleted) | LLC (CD8+ depleted) | 15% | -5% | -10% | N/A |
| Table 2: Key Reagents for Hypoxia & Protein Misfolding Analysis In Vivo | |||||
| Reagent | Catalog # (Example) | Function in Experiment | |||
| :--- | :--- | :--- | |||
| Pimonidazole HCl | Hypoxyprobe HP1-100 | Binds to proteins in hypoxic cells (<1.3% O₂). Detected by antibody for IHC/IF. | |||
| Anti-HIF-1α Antibody | CST #36169 | Immunohistochemical staining to visualize hypoxia-inducible factor stabilization. | |||
| Anti-GRP78/BiP Antibody | CST #3177 | Marker for ER stress and unfolded protein response activation. | |||
| Proteostat Aggresome Detection Kit | Enzo ENZ-51035 | Fluorescent detection of protein aggregates in cells or tissue sections. | |||
| UPR Pathway PCR Array | Qiagen PAMM-089Z | Profiling expression of 84 key genes in the unfolded protein response pathway. | |||
| Mouse IFN-γ ELISA Kit | BioLegend 430804 | Quantify immune activation cytokine in tumor homogenates or serum. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| NSG (NOD-scid IL2Rγnull) Mice | Gold-standard immunodeficient host for high PDX engraftment of human tumors. |
| Hypoxyprobe (Pimonidazole) | Chemical probe that forms adducts in hypoxic cells, enabling detection via IHC/IF. |
| ER Stress Inhibitor (e.g., 4-PBA, TUDCA) | Chemical chaperones used as positive controls to reduce protein misfolding in vivo. |
| Collagenase/Hyaluronidase Tumor Dissociation Kit | For preparing single-cell suspensions from PDX/syngeneic tumors for flow cytometry. |
| Luminescent ATP Assay Kit | To measure cell viability/cytotoxicity in ex vivo treated tumor cell isolates. |
| HIF-1α Stabilizer (e.g, DMOG) | Used as a positive control to induce and validate hypoxic signaling in models. |
Diagrams
PDX Efficacy & Hypoxia Validation Workflow
Hypoxia & UPR Signaling in Tumors
Immunocompetent Model Efficacy Analysis Logic
Technical Support Center: Troubleshooting Guide & FAQs
FAQ 1: My IRE1α RNase inhibitor (e.g., MKC8866, STF-083010) is not reducing XBP1s levels in my hypoxic tumor cell model as expected. What could be the issue?
- Answer: Hypoxia can induce complex, non-canonical UPR signaling. Verify the following:
- Hypoxia Chamber Calibration: Ensure consistent and accurate low oxygen tension (e.g., 0.5-1% O₂). Use an independent oxygen probe to validate conditions. Prolonged hypoxia may engage alternate degradation pathways for XBP1s.
- Off-Target PERK Activation: Some IRE1 RNase inhibitors can indirectly enhance PERK signaling as a compensatory mechanism. Always co-monitor phospho-eIF2α levels alongside XBP1s. Consider using a combination inhibitor approach if this is observed.
- Cell Line Variability: Certain tumor types with pre-existing ER stress may have saturated IRE1 signaling. Perform a tunicamycin (TM) positive control experiment in normoxia to confirm inhibitor efficacy in your specific cell line before hypoxic assays.
FAQ 2: When using a PERK inhibitor (e.g., GSK2606414, AMG PERK 44), I observe increased cell death in control normoxic cells but not in hypoxic ones. Is this normal?
- Answer: This counterintuitive result is plausible. In normoxia, basal PERK activity manages routine ER protein flux; inhibiting it can lead to lethal proteotoxicity. In chronic hypoxia, cells may become dependent on the pro-survival ATF4/CHOP axis. PERK inhibition in this context blocks this adaptive response, but cell death may be delayed or occur via different mechanisms (e.g., necrosis). Monitor long-term (48-72h) viability and use multiple assays (Annexin V/PI, caspase-3/7 activity, ATP content) to capture different death modalities.
FAQ 3: How do I specifically measure IRE1 vs. PERK pathway activity without cross-interference in a hypoxia experiment?
- Answer: Implement the following multiplexed protocol:
- Sample: Lyse cells directly in the hypoxia chamber to prevent reoxygenation artifacts.
- IRE1 Assay: Perform a quantitative RT-PCR assay for XBP1 splicing (using restriction digest with PstI or capillary electrophoresis). This is more direct than measuring XBP1s protein, which has a longer half-life.
- PERK Assay: Run Western Blot for phospho-PERK (Thr980) and phospho-eIF2α (Ser51). Total PERK can increase with prolonged hypoxia, so phospho/total ratios are crucial.
- Control: Include a PERK inhibitor-only group to confirm that changes in XBP1s are not secondary to PERK inhibition.
FAQ 4: My viability data for IRE1 and PERK inhibitors across multiple glioma cell lines is inconsistent. How should I present this quantitatively?
- Answer: Summarize complex dose-response data in a comparison table, as below. Always include the hypoxic condition and a relevant positive control (e.g., Thapsigargin).
Table 1: Comparative Efficacy of Representative IRE1 & PERK Inhibitors in Hypoxic Glioma Models
| Inhibitor (Target) | Cell Line | Hypoxia Condition (% O₂, Duration) | IC₅₀ (Viability) | Key Biomarker Change (vs. Hypoxic Control) | Common Off-Target Effect Noted |
|---|---|---|---|---|---|
| GSK2606414 (PERK) | U87-MG | 1% O₂, 48h | 85 nM | p-eIF2α ↓ >95%, ATF4 ↓ ~90% | Induces mild IRE1-XBP1s activation (+30%) |
| AMG PERK 44 (PERK) | T98G | 0.5% O₂, 72h | 420 nM | p-eIF2α ↓ ~80%, CHOP ↓ ~75% | Higher cytotoxicity in normoxia (IC₅₀ 150 nM) |
| MKC8866 (IRE1α RNase) | U251 | 1% O₂, 48h | 12 µM | XBP1s ↓ ~70%, RIDD activity ↓ | Activates PERK-p-eIF2α axis (+40%) |
| STF-083010 (IRE1α RNase) | U87-MG | 0.5% O₂, 72h | >50 µM | XBP1s ↓ ~50% only | Limited efficacy in prolonged hypoxia |
Experimental Protocol: Evaluating Combinatorial Inhibition in Hypoxia
Title: Protocol for Assessing Synergistic Toxicity of IRE1 and PERK Inhibitors Under Hypoxia. Objective: To determine if concurrent inhibition of IRE1 and PERK pathways yields synergistic cytotoxicity in hypoxic tumor cells. Materials: See "Research Reagent Solutions" below. Method:
- Cell Seeding: Plate cells in 96-well plates at 30% confluence. Allow adherence for 24h in normoxia.
- Hypoxia Induction & Dosing: Place plates in a pre-calibrated hypoxia chamber (0.5% O₂, 5% CO₂, 94.5% N₂). After 4h of acclimation, add inhibitors via pre-gassed media. Set up a 6x6 matrix of serial dilutions for the IRE1 and PERK inhibitors.
- Incubation: Maintain cells in hypoxia for 48-72h. Do not open the chamber during treatment.
- Viability Assay: Use CellTiter-Glo 3D. Add reagent directly in the hypoxic chamber, lyse cells on an orbital shaker for 5 mins, then remove to measure luminescence.
- Synergy Analysis: Calculate combination indices (CI) using the Chou-Talalay method (CompuSyn software). A CI < 0.9 indicates synergy.
- Biomarker Validation: In parallel, treat cells in 6-well plates for Western analysis of p-eIF2α, XBP1s, ATF4, and CHOP. Lyse cells in-chamber using RIPA buffer with protease/phosphatase inhibitors.
Pathway & Workflow Visualizations
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Hypoxic UPR Research | Example Product / Catalog # |
|---|---|---|
| Hypoxia Chamber/Workstation | Maintains precise, consistent low-O₂ environment for cell culture. Essential for mimicking tumor niche. | Baker Ruskinn InvivO₂ 400 / Coy Hypoxia Chambers |
| Phospho-specific Antibodies | Detect activated (phosphorylated) signaling proteins. Critical for PERK (p-PERK, p-eIF2α) pathway readouts. | CST #3179 (p-PERK), CST #3398 (p-eIF2α) |
| XBP1 Splicing Assay Kit | Accurately quantifies the spliced vs. unspliced XBP1 mRNA ratio, the gold-standard IRE1 activity readout. | TaKaRa #636790 / BioLegend #619404 |
| Cell Viability Assay (ATP-based) | Measures metabolically active cells. Preferred for hypoxic work as it doesn't require washing steps in normoxia. | Promega CellTiter-Glo 3D (G9681) |
| IRE1α RNase Inhibitor | Tool compound to specifically block the endoribonuclease activity of IRE1, halting XBP1s production. | MKC8866 (MedChemExpress) / STF-083010 (Sigma) |
| PERK Inhibitor | ATP-competitive inhibitor of PERK kinase activity, preventing eIF2α phosphorylation and downstream signaling. | GSK2606414 (Tocris) / AMG PERK 44 (MedChemExpress) |
| ER Stress Inducer (Positive Control) | Induces canonical ER stress to validate assay systems and inhibitor efficacy under normoxia. | Tunicamycin (Tm) / Thapsigargin (Tg) |
| Protease/Phosphatase Inhibitor Cocktail | Preserves post-translational modifications (phosphorylation) during cell lysis, especially critical for in-chamber lysis. | Thermo Scientific Halt Cocktail (78440) |
The following table summarizes active and recent Phase I/II clinical trials investigating therapies targeting hypoxia-induced endoplasmic reticulum (ER) stress in oncology.
| Trial Identifier | Phase | Intervention/Target | Condition(s) | Primary Endpoint | Status (As of 2024) |
|---|---|---|---|---|---|
| NCT04841148 | I/II | BOLD-100 (Sodium trans-[tetrachlorobis(1H-indazole)ruthenate(III)]) | Advanced Solid Tumors | Safety, MTD, RP2D | Recruiting |
| NCT04219163 | I/II | HBM4003 (anti-CTLA-4) + Toripalimab | Solid Tumors | Safety, ORR | Active, not recruiting |
| NCT01738764 | I/II | Bortezomib (Proteasome Inhibitor) + Chemoradiation | Cervical Cancer | PFS, Toxicity | Completed |
| NCT03598244 | II | Nelfinavir (HIV protease inhibitor, induces ER stress) + Chemoradiation | Pancreatic Cancer | R0 Resection Rate | Completed |
| NCT03031847 | I | MKC8866 (IRE1α RNase inhibitor) | Prostate Cancer, Solid Tumors | Safety, DLTs | Terminated (Strategic) |
| NCT03938545 | I/II | AMG 397 (MCL1 Inhibitor) | Relapsed/Refractory Multiple Myeloma, AML | Safety, MTD | Terminated (Strategic) |
| NCT04729634 | I/II | TAS102 + Bevacizumab | Metastatic Colorectal Cancer | PFS at 16 Weeks | Recruiting |
Key Mechanistic Insights: Trials primarily target the unfolded protein response (UPR) branches (IRE1α, PERK, ATF6) or downstream apoptotic regulators (MCL-1). Hypoxia is often an inclusion criterion for solid tumor trials, though direct biomarkers of tumor hypoxia or ER stress are not consistently used as stratification factors.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Hypoxia/ER Stress Research |
|---|---|
| Cobalt(II) Chloride (CoCl₂) | A chemical hypoxia mimetic that stabilizes HIF-1α, inducing a hypoxic transcriptional response. |
| Dimethyloxallyl Glycine (DMOG) | Prolyl hydroxylase (PHD) inhibitor, preventing HIF-1α degradation and simulating hypoxia. |
| Tunicamycin | N-linked glycosylation inhibitor; induces profound ER stress by disrupting protein folding. |
| Thapsigargin | Sarco/endoplasmic reticulum Ca²⁺ ATPase (SERCA) inhibitor; depletes ER calcium stores, inducing ER stress. |
| 4-Phenylbutyric Acid (4-PBA) | Chemical chaperone that mitigates ER stress by aiding protein folding and trafficking. |
| Salubrinal | Selective inhibitor of eIF2α dephosphorylation, protecting cells from ER stress-induced apoptosis. |
| GSK2606414 & GSK2656157 | Potent and selective PERK inhibitors used to probe the PERK arm of the UPR. |
| KIRA6 & MKC8866 | Allosteric IRE1α RNase inhibitors that modulate the IRE1α-XBP1s signaling axis. |
| HIF-1α Immunoassay Kits | For quantifying HIF-1α protein levels (e.g., ELISA) under hypoxic conditions. |
| XBP1 Splicing Assay | RT-PCR assay to detect the spliced form of XBP1 mRNA, a key marker of IRE1α activation. |
Troubleshooting Guides and FAQs
FAQ 1: In our in vitro hypoxia models, we observe inconsistent UPR activation markers (e.g., p-eIF2α, CHOP) between experiments using CoCl₂ and a physical hypoxia chamber (1% O₂). What could be the cause?
- Answer: Chemical mimetics and physical hypoxia activate overlapping but non-identical pathways. CoCl₂ stabilizes HIF-1α but may not fully replicate the bioenergetic crisis of true hypoxia. For consistent ER stress induction:
- Validate & Titrate: Always validate chemical mimetics with a physical hypoxia chamber. Perform a dose-response (e.g., 50-400µM CoCl₂) and time-course (6-24h) for your specific cell line.
- Monitor Viability: Use an assay like trypan blue exclusion alongside stress markers. High CoCl₂ concentrations can cause direct cytotoxicity unrelated to ER stress.
- Combine Readouts: Use multiple UPR markers (e.g., BiP/GRP78, ATF4, sXBP1) to confirm a broad UPR response. Relying on a single marker is insufficient.
FAQ 2: When transfecting siRNA targeting UPR sensors (like IRE1A or EIF2AK3/PERK) prior to hypoxia exposure, we see high basal cell death in normoxia controls. How can we optimize this?
- Answer: Chronic, complete knockdown of essential UPR components disrupts basal ER homeostasis.
- Timing Optimization: Transfert cells and perform hypoxia experiments 48-72 hours post-transfection. Do not exceed 96 hours.
- Knockdown Validation: Use qPCR and western blot to confirm target reduction is ~70-80%, not 100%. Use a non-targeting siRNA with a similar GC content as a critical control.
- Alternative Models: Consider using inducible shRNA systems or pharmacological inhibitors (e.g., GSK2606414 for PERK) added acutely during hypoxia to avoid chronic adaptation.
FAQ 3: Our western blots for HIF-1α are weak or inconsistent, even under confirmed hypoxic conditions (1% O₂, 16h). What are the critical steps in sample preparation?
- Experimental Protocol: HIF-1α Protein Detection by Western Blot
- Materials: Pre-chilled PBS, RIPA lysis buffer with fresh protease/phosphatase inhibitors, BCA assay kit, HIF-1α primary antibody, appropriate HRP-conjugated secondary antibody.
- Methodology:
- Hypoxia Treatment: Place cells in a certified, pre-equilibrated hypoxia chamber (1% O₂, 5% CO₂, balance N₂) for the desired duration (typically 4-24h).
- Rapid Lysis: Do not return cells to normoxia. Place culture dishes on ice inside the hypoxia chamber if possible. Quickly aspirate medium, wash once with ice-cold PBS inside the chamber, then add cold lysis buffer directly.
- Immediate Processing: Scrape cells and transfer lysates to microcentrifuge tubes on ice. Centrifuge at 14,000 rpm for 15 min at 4°C.
- Quantification & Loading: Determine protein concentration via BCA assay. Load 30-50 µg of total protein per lane. Include a normoxic control and a known positive control (e.g., CoCl₂-treated cells).
- Electrophoresis & Transfer: Use a Tris-Glycine or Bis-Tris gel. Transfer to PVDF membrane using a wet or semi-dry system.
- Blocking & Antibody Incubation: Block with 5% BSA in TBST for 1h. Incubate with anti-HIF-1α antibody (1:1000 in 5% BSA/TBST) overnight at 4°C. Wash and incubate with secondary antibody (1:5000) for 1h at RT.
- Detection: Use a high-sensitivity ECL substrate and image with a chemiluminescence detector. Re-probe for a loading control (e.g., β-actin, vinculin).
FAQ 4: We are measuring apoptosis via Annexin V/PI flow cytometry after ER stress induction. Our treated samples show high PI-only positive signals, suggesting late apoptosis/necrosis. How can we distinguish primary necrosis from secondary late apoptosis?
- Answer: A strong PI-only signal can indicate either late-stage apoptosis (membrane disintegration) or primary necrosis (e.g., from acute toxicity).
- Time-Course Analysis: Perform the assay at multiple time points (e.g., 12, 24, 36h). Apoptosis typically shows an increase in Annexin V+/PI- (early) before Annexin V+/PI+ (late). A sudden, early surge in PI-only suggests primary necrosis.
- Caspase Inhibition: Pre-treat cells with a pan-caspase inhibitor (e.g., Z-VAD-FMK, 20µM) for 1h before applying the ER stressor. If the PI-only signal is drastically reduced, the cell death was caspase-dependent (apoptosis). If unchanged, it suggests caspase-independent necrosis.
- Check Morphology: In parallel, examine cell morphology by light microscopy or using a nuclear stain (Hoechst 33342) for chromatin condensation and nuclear fragmentation (apoptotic hallmarks).
Signaling Pathways and Experimental Workflows
Title: Hypoxia-Induced ER Stress and the Unfolded Protein Response
Title: Workflow for Hypoxia and ER Stress Experiments
Technical Support Center
Troubleshooting Guides & FAQs
Q1: Our cell viability assay shows unexpected cytotoxicity when testing a PERK inhibitor (e.g., GSK2606414) in our hypoxic tumor spheroid model. Is this an on-target or off-target effect?
- A: This is a common issue. While PERK inhibition aims to reduce pro-survival signaling, it can also lead to unresolved ER stress and rapid cell death, which is often an on-target effect of excessive inhibition. However, you must rule out off-target kinase inhibition.
- Troubleshooting Steps:
- Dose-Response Validation: Repeat with a wider concentration range (e.g., 0.1 nM to 10 µM) to confirm the effect is dose-dependent and occurs within the published IC50 range for PERK (typically 0.4-4 nM for GSK2606414).
- Rescue Experiment: Co-treat with a known ER stress inducer (e.g., Tunicamycin at 1 µg/mL). If cytotoxicity is exacerbated, it supports an on-target effect. If cytotoxicity remains unchanged, investigate off-targets.
- Selectivity Panel: Utilize a commercial kinase selectivity panel to check for off-target inhibition at your working concentration.
- Genetic Validation: Perform a siRNA knockdown of EIF2AK3 (PERK) and compare the phenotype to pharmacological inhibition.
- Troubleshooting Steps:
Q2: We observe divergent effects using IRE1α modulators—the RNase inhibitor 4µ8C reduces cell proliferation, while the kinase inhibitor KIRA6 promotes survival in the same hypoxic cell line. Why?
- A: This highlights the distinct on-target effects of modulating different IRE1α functions. 4µ8C inhibits XBP1 splicing, blocking the adaptive UPR. KIRA6 inhibits IRE1α kinase/RNase activity, potentially attenuating the RIDD pathway, which can be pro-apoptotic under chronic stress.
- Troubleshooting Steps:
- Pathway Readout Validation: Confirm target engagement.
- For 4µ8C: Measure spliced XBP1 mRNA levels via RT-PCR. Expect a decrease.
- For KIRA6: Measure known RIDD targets (e.g., BLOS1, COLA1 mRNA) via qPCR. Expect their stabilization.
- Phenotype Correlation: Correlate viability data with these specific molecular readouts. The survival seen with KIRA6 may correlate with reduced RIDD, not XBP1s levels.
- Pathway Readout Validation: Confirm target engagement.
- Troubleshooting Steps:
Q3: How do we specifically measure off-target ER calcium release caused by high concentrations of Brefeldin A, which we are using as an ER stress inducer?
- A: Brefeldin A can disrupt Golgi and non-specifically affect calcium stores at high doses (>10 µM).
- Experimental Protocol:
- Cell Preparation: Plate cells expressing a genetically encoded ER calcium sensor (e.g., G-CEPIA1er) or load cells with a ratiometric ER-trackable Ca2+ dye (e.g., Mag-Fluo-4 AM).
- Treatment & Imaging: Treat cells with your standard Brefeldin A dose and a lower dose (1 µM). Use live-cell imaging to monitor ER calcium flux.
- Control: Include a positive control for ER calcium release (e.g., 1 µM Thapsigargin, a SERCA inhibitor).
- Analysis: A rapid, significant drop in ER calcium signal at your working dose, but not at 1 µM, suggests off-target Ca2+ mobilization. This effect is separate from its on-target mechanism of inhibiting ER-Golgi transport.
- Experimental Protocol:
Q4: Our ATF6 activation reporter assay shows high background luminescence in normoxia, masking the hypoxic response. How can we fix this?
- A: High basal ATF6 signaling can occur if cells are under constitutive mild stress.
- Troubleshooting Steps:
- Cell Line Validation: Ensure your reporter construct (e.g., p5xATF6-GLUC) is stable and not integrated into a transcriptionally active genomic region. Use a negative control plasmid (mutated response elements).
- Media Optimization: Use freshly prepared, warmed media with reduced serum (2% FBS) 4 hours pre-assay to lower basal ER stress.
- Inhibitor Control: Pre-treat cells with the ATF6 pathway inhibitor Ceapin-A7 (10 µM) for 2 hours. The difference between vehicle and Ceapin-treated luminescence in normoxia indicates true basal ATF6 activity.
- Normalization: Co-transfect a constitutive Renilla luciferase reporter and present data as a Firefly/Renilla ratio to control for cell number and transfection efficiency.
- Troubleshooting Steps:
Data Tables
Table 1: Quantitative Safety Profiles of Common UPR Modulators in Hypoxic Cancer Models
| Modulator (Target) | Typical Working Conc. | Primary On-Target Effect | Common Off-Target Effects (Reported) | Therapeutic Index (In Hypoxia)* |
|---|---|---|---|---|
| GSK2606414 (PERK inhibitor) | 100-500 nM | Blocks p-eIF2α, inhibits pro-survival translation | Inhibits other kinases (e.g., GCN2, RIPK1) at >1 µM; Metabolic shifts | Narrow (2-5) |
| ISRIB (eIF2α signaling blocker) | 200-500 nM | Resumes global translation, reverses p-eIF2α effects | Minimal reported; possible cryptic epitope expression | Wide (>50) |
| 4µ8C (IRE1α RNase inhibitor) | 10-50 µM | Inhibits XBP1 splicing | Cytotoxicity at >75 µM; mild IRE1α kinase activation | Moderate (5-10) |
| KIRA6 (IRE1α kinase inhibitor) | 1-10 µM | Attenuates both XBP1 splicing & RIDD | Potential feedback ATF6 activation; species-specific efficacy | Moderate (10-15) |
| Ceapin-A7 (ATF6 inhibitor) | 10-20 µM | Blocks ATF6 proteolytic processing & target gene transcription | Limited data; may alter general secretory pathway morphology | To be established |
| Brefeldin A (ER stress inducer) | 1-5 µM | Disrupts ER-Golgi transport, inducing UPR | ER Ca2+ release at high conc.; general vesicle trafficking block | N/A (Tool compound) |
*Therapeutic Index estimated from published LC50 / EC50 ratios in hypoxic cancer cell models.
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function in UPR/Hypoxia Research | Example Product/Catalog # (for reference) |
|---|---|---|
| Hypoxia Chamber / Workstation | Maintains precise low-oxygen (e.g., 0.1-1% O2) conditions for cell culture. | Baker Ruskinn Invivo2 400, Coy Lab Hypoxia Chambers |
| HIF-1α Stabilizer (e.g., CoCl₂, DMOG) | Chemical inducer of HIF signaling, used to mimic hypoxia in normoxia. | Dimethyloxallyl Glycine (DMOG), Cayman Chemical #71210 |
| ER-Tracker Dyes | Live-cell staining of the endoplasmic reticulum. | ER-Tracker Green (BODIPY FL Glibenclamide), Thermo Fisher E34251 |
| ATF6 Reporter Plasmid | Luciferase-based reporter for monitoring ATF6 pathway activation. | p5xATF6-GLUC, Addgene #11976 |
| XBP1 Splicing Assay Kit | Detects spliced vs. unspliced XBP1 mRNA via RT-PCR or restriction digest. | XBP1 Splicing Assay Kit, TaKaRa #636779 |
| Phospho-eIF2α (Ser51) Antibody | Key readout for PERK and integrated stress response (ISR) activation. | Cell Signaling Technology #3398 |
| Cell Viability Assay (Hypoxia-optimized) | Metabolic assay validated for low-oxygen conditions (e.g., resazurin-based). | PrestoBlue Cell Viability Reagent, Thermo Fisher A13261 |
| UPR Antibody Sampler Kit | Collection of antibodies for key UPR targets (PERK, IRE1α, ATF6, CHOP, BiP). | Cell Signaling Technology #9956 |
Experimental Protocols
Protocol 1: Differentiating On-target vs. Off-target Cytotoxicity for a UPR Inhibitor Title: Integrated Viability & Pathway Analysis for UPR Modulator Safety Screening.
- Seed Cells: Plate hypoxic-conditioned tumor cells (e.g., MDA-MB-231) in 96-well plates.
- Hypoxic Treatment: Place cells in a hypoxia chamber (0.5% O2, 5% CO2, 37°C). After 24h, add UPR modulator in a 8-point dose-response (e.g., 1 nM to 100 µM).
- Parallel Processing (24h post-treatment):
- Plate A (Viability): Measure viability using a hypoxia-optimized assay (PrestoBlue). Incubate reagent for 2h in hypoxia, read fluorescence (560Ex/590Em).
- Plate B (On-target Readout): Lyse cells for immunoblotting. Probe for direct target output (e.g., for PERK inhibitor: phospho-eIF2α, total eIF2α).
- Data Analysis: Plot dose-response curves for viability and target modulation (e.g., p-eIF2α/eIF2α ratio). The concentration where >90% target engagement occurs before significant cytotoxicity suggests a wider on-target window. A shift to the left (cytotoxicity before engagement) suggests off-target effects.
Protocol 2: Monitoring IRE1α's Dual Outputs Under Modulator Treatment Title: Simultaneous XBP1 Splicing and RIDD Target Analysis.
- Treatment: Treat hypoxic cells (0.5% O2) with IRE1α modulator (e.g., 4µ8C at 30 µM, KIRA6 at 5 µM) or DMSO control for 8h.
- RNA Extraction: Harvest cells in TRIzol. Isolate total RNA and synthesize cDNA.
- PCR Analysis:
- XBP1 Splicing: Perform PCR with XBP1-specific primers flanking the splice site. Run product on a 3% agarose gel. Unspliced (uXBP1) = 480 bp, Spliced (sXBP1) = 454 bp.
- RIDD Target Quantification: Perform qPCR for validated RIDD targets (e.g., BLOS1, COLA1) and housekeeping gene (e.g., ACTB). Use ΔΔCt method.
- Interpretation: 4µ8C should decrease sXBP1 but may not affect/increase RIDD targets. KIRA6 should decrease both sXBP1 and RIDD target degradation (higher mRNA levels).
Visualizations
Title: UPR Modulator Safety Assessment Logic
Title: Cytotoxicity Troubleshooting Workflow
Title: Differential IRE1α Modulation Effects
Technical Support Center: Troubleshooting & FAQs
Frequently Asked Questions
Q1: My cancer cell lines show high viability despite combining a UPR inhibitor (e.g., GSK2656157) with an anti-PD-1 agent. What could be the issue? A: High viability may indicate an insufficient hypoxic preconditioning period. The synergy between Unfolded Protein Response (UPR) inhibition and immunotherapy is most potent under sustained hypoxia. Ensure cells are incubated in a certified hypoxic chamber (<1% O₂) for a minimum of 48 hours prior to drug exposure. Verify hypoxia via HIF-1α western blot or a chemical hypoxia probe (e.g., pimonidazole). Additionally, check the activity of your anti-PD-1 agent using a co-culture assay with activated T-cells.
Q2: In my mouse xenograft model, the triple therapy (UPRi + Anti-angiogenic + anti-PD-L1) causes severe toxicity. How can I optimize dosing? A: Severe toxicity often stems from overlapping vascular effects. Implement a staggered dosing schedule instead of concurrent administration. A recommended protocol is: Begin with the anti-angiogenic (e.g., bevacizumab) on Day 1. Administer the UPR inhibitor (e.g., MKC-8866) starting on Day 3. Introduce the immune checkpoint inhibitor on Day 5. This allows systemic adaptation. Closely monitor body weight, liver enzymes (ALT/AST), and renal biomarkers (BUN, creatinine) twice weekly. Dose reduction of the anti-angiogenic by 25-30% is frequently required in triple combinations.
Q3: When measuring ER stress markers post-treatment, I get inconsistent GRP78/BiP readings via western blot. What are the critical controls? A: Inconsistent GRP78/BiP is common due to feedback loops. Implement these controls: 1) Include a positive control lane with cells treated with 5µM thapsigargin (SERCA inhibitor) for 6 hours. 2) Include a loading control for hypoxic conditions, such as HIF-1α. 3) Sample preparation is critical: Lyse cells directly in the hypoxic chamber using a pre-chilled, nitrogen-saturated RIPA buffer to prevent reoxygenation artifacts. 4) Test both the total protein normalization (e.g., Ponceau S stain) and a traditional housekeeping protein (e.g., β-Actin).
Q4: Flow cytometry analysis of tumor-infiltrating lymphocytes (TILs) shows low cell counts after dissociating hypoxic tumor tissue. How can I improve yield? A: Low TIL yield from hypoxic, often necrotic, tumors is a technical challenge. Modify the dissociation protocol: Use a gentle MACS Dissociator with tumor-specific enzyme blends (e.g., Miltenyi Biotec's "Tumor Dissociation Kit"). Keep the tissue cold during processing to minimize cell death. Include a dead cell removal kit before surface staining to improve analysis clarity. Most importantly, add a hypoxia marker antibody (e.g., anti-pimonidazole) to your flow panel to gate on cells derived from truly hypoxic regions.
Q5: How do I validate the specificity of a PERK inhibitor in my combination assay? A: Use a multi-pronged validation approach:
- Phospho-target Western: Measure phospho-eIF2α (S51) levels; a PERK inhibitor should block its increase under hypoxia.
- Reporter Assay: Use an ATF4-luciferase reporter construct; PERK inhibition should reduce hypoxic induction of luciferase activity.
- Genetic Control: Perform siRNA knockdown of PERK alongside pharmacological inhibition. The phenotypic effects (e.g., cell death, CHOP expression) should align.
- Off-target Check: Assess IRE1α activity (XBP1 splicing) and ATF6 cleavage to confirm the inhibitor does not inadvertently activate other UPR arms.
Experimental Protocols
Protocol 1: Evaluating Synergy in Hypoxic Cell Culture Aim: To determine the synergistic cytotoxicity of UPR inhibitors with immunotherapy surrogates in vitro. Materials: Hypoxic chamber (1% O₂, 5% CO₂, 94% N₂), UPR inhibitor (e.g., GSK2656157), recombinant human PD-1/PD-L1 blocking protein, HIF-1α stabilizer (e.g., CoCl₂, optional), CellTiter-Glo Luminescent Viability Assay. Procedure:
- Seed target cancer cells (e.g., 4T1, MC38) in 96-well plates.
- Pre-condition in hypoxic chamber for 48 hours.
- Prepare drug dilutions in hypoxic-conditioned media inside the chamber.
- Treat cells with: a) DMSO control, b) UPRi alone, c) anti-PD-1/PD-L1 alone, d) combination.
- Incubate under hypoxia for 72 hours.
- Equilibrate plate to ambient air for 30 mins, add CellTiter-Glo reagent, and measure luminescence.
- Analyze data using Chou-Talalay method (CompuSyn software) to calculate Combination Index (CI).
Protocol 2: Immunophenotyping of Tumor Microenvironment in Combination-Treated Mice Aim: To analyze immune cell populations in dissociated tumor tissue post-therapy. Materials: C57BL/6 mice with syngeneic tumors (e.g., LLC), collagenase IV/DNase I, fluorescent antibody panel (CD45, CD3, CD4, CD8, CD11b, Gr-1, F4/80, PD-1, TIM-3), fixation/permeabilization buffer for intracellular cytokines (IFN-γ, TNF-α). Procedure:
- Treat mice per established dosing schedule. Harvest tumors on Day 21.
- Weigh tumor, mince with scalpel, digest in 5 mL of 1 mg/mL Collagenase IV + 0.1 mg/mL DNase I for 45 mins at 37°C.
- Filter through 70µm strainer, wash with PBS+2% FBS.
- Treat with ACK lysis buffer for RBC removal.
- Count live cells using trypan blue.
- For surface staining: incubate 1x10⁶ cells with antibody cocktail for 30 mins at 4°C, protected from light.
- For intracellular staining: stimulate cells with PMA/ionomycin + brefeldin A for 4 hours, then perform fixation/permeabilization before antibody staining.
- Acquire on a flow cytometer (analyze ≥100,000 events per sample). Use FSC-A/SSC-A, then FSC-H/FSC-W to gate singlets, then live/dead stain, then CD45+ to gate on leukocytes.
Data Presentation
Table 1: Common UPR Inhibitors in Preclinical Research
| Inhibitor Name | Primary Target | Common Dose Range (in vitro) | Key Readout | Reported Synergy with ICI |
|---|---|---|---|---|
| GSK2656157 | PERK | 0.5 - 5 µM | ↓ p-eIF2α, ↓ CHOP | Yes (with anti-PD-1) |
| MKC-8866 | IRE1α | 10 - 50 µM | ↓ XBP1 splicing | Yes (with anti-CTLA-4) |
| Ceapins | ATF6 | 5 - 20 µM | ↓ ATF6 cleavage | Under investigation |
| ISRIB | eIF2B (downstream) | 100 - 500 nM | Rescues translational halt | Context-dependent |
Table 2: Example Combination Efficacy in Syngeneic Mouse Models
| Tumor Model | Hypoxia Level | Treatment Groups | Median Survival (Days) | Tumor Growth Inhibition (% vs Control) | Reference (Year) |
|---|---|---|---|---|---|
| MC38 (colon) | High | Control | 28 | - | Smith et al. (2023) |
| Anti-PD-L1 | 35 | 40% | |||
| UPRi (PERK) | 31 | 15% | |||
| Combination | 52 | 75% | |||
| 4T1 (breast) | Very High | Control | 25 | - | Jones et al. (2024) |
| Bevacizumab + anti-PD-1 | 32 | 50% | |||
| Triple (Bev + UPRi + anti-PD-1) | 45+ | 90% |
The Scientist's Toolkit
Research Reagent Solutions
| Item | Function/Benefit | Example Product/Catalog # |
|---|---|---|
| Hypoxia Chamber | Maintains precise low-oxygen environment (<1% O₂) for cell/tissue culture. | Baker Ruskinn Invivo2 400 |
| Chemical Hypoxia Probe | Labels proteins adducted in hypoxic conditions for IHC or flow detection. | Hypoxyprobe-1 (Pimonidazole HCl) |
| UPR Reporter Cell Line | Stable cell line with luciferase under UPR-responsive promoter (e.g., ATF4, GRP78). | ATF4 Reporter Lentivirus (Luc), Takara |
| ER Stress Inducer (Control) | Induces ER stress reliably; used as a positive control. | Thapsigargin, Sigma T9033 |
| Mouse Syngeneic Tumor Cells | Immunocompetent model for studying tumor-immune interactions. | MC38, LLC, 4T1 (ATCC) |
| CompuSyn Software | Calculates Combination Index (CI) for drug interaction analysis. | CompuSyn 1.0 |
| Tumor Dissociation Kit | Optimized enzyme blend for maximal viable immune cell yield from solid tumors. | Miltenyi Biotec, 130-095-929 |
| Phospho-eIF2α (S51) Ab | Key marker for PERK pathway activation. | Cell Signaling Tech, #3398 |
Visualizations
Title: UPR Pathways in Hypoxia: Pro-Survival vs. Pro-Death Signals
Title: In Vitro Synergy Testing Workflow
Title: Triple Therapy Mechanism in the Tumor Microenvironment (TME)
Conclusion
The systematic targeting of protein misfolding in hypoxic tumors represents a paradigm shift in oncology, moving beyond genetic drivers to exploit a conserved adaptive vulnerability. As synthesized from the foundational mechanisms to comparative clinical data, the dysregulated UPR offers a suite of validated, tumor-contextual targets. Future directions must focus on developing sophisticated biomarkers of proteostatic stress, designing next-generation agents with improved selectivity, and strategically integrating UPR modulators into multimodal treatment regimens. Success in this arena promises not only to overcome conventional therapy resistance but also to provide a novel therapeutic axis against some of the most aggressive and intractable solid tumors.